Abstract
Chromogranin A (CgA) is widely used as an immunohistochemical marker of neuroendocrine neoplasms and has been measurable in plasma of patients. We assessed the clinical role of plasma CgA in diagnosing pancreatic neuroendocrine neoplasm (PNEN). CgA was checked in 44 patients with pancreatic mass who underwent surgical resection from 2009 through 2011. The cutoff value for diagnosing PNEN and the relationships between CgA and clinicopathologic variables were analyzed. Twenty-six patients were PNENs and 18 patients were other pancreatic disorders. ROC analysis showed a cutoff of 60.7 ng/mL with 77% sensitivity and 56% specificity, and the area under the curve (AUC) was 0.679. Among PNEN group, the sensitivity and specificity of diagnosing metastasis were 100% and 90% respectively when CgA cutoff was 156.5 ng/mL. The AUC was 0.958. High Ki-67 index (160.8 vs 62.1 ng/mL, P = 0.001) and mitotic count (173.5 vs 74.6 ng/mL, P = 0.044) were significantly correlated with plasma CgA, but the tumor size was not. In conclusion, CgA has a little value in diagnosing PNEN. However, the high level of CgA (more than 156.5 ng/mL) can predict the metastasis. Also, plasma CgA level correlates with Ki-67 index and mitotic count which represents prognosis of PNENs.
There are many kinds of pancreatic neoplasms including ductal adenocarcinoma, endocrine tumors, cystic tumors, solid pseudopapillary tumors, acinar cell carcinoma, squamous cell carcinoma, lymphoma, and metastatic lesions of pancreas (1). Also, the incidence of incidental pancreatic masses has risen rapidly over the past three decades, partly as a result of the increased detection on endoscopic or cross-sectional imaging (2-4). However, there is a limitation in the differential diagnosis of diverse pancreatic tumors by imaging diagnostic methods alone (5, 6).
Pancreatic neuroendocrine neoplasms (PNENs) are rare neoplasms which have an incidence of approximately one per 100,000 individuals per year and represent approximately 3% of all pancreatic tumors (2, 7). Several studies have documented a trend towards the increasing incidence and prevalence in recent years (8). PNENs are typically hyperdense and spherical on the arterial phase of imaging, but sometimes they are described as hypovascular or cystic lesions (9). Thus, non-invasive parameters indicating PNENs are required.
Chromogranin A (CgA) is a 439-amino-acid protein that is present in the secretory dense core granules of neuroendocrine tissues (10). CgA is widely used as an immunohistochemical marker of neuroendocrine neoplasms (11). In addition, CgA is overproduced and released into the circulation by neuroendocrine neoplasms and has consequently been measurable in plasma of patients (12). The previous studies reported different ranges of sensitivity and specificity for circulating CgA, according to histological characteristics of the tumor and to disease spread (13-15). Besides, previous studies included all the neuroendocrine neoplasms originating in gastroenteropancreatic system. Therefore, we enrolled PNENs only in this study to analyze the usefulness of CgA in differentiating PNENs with other pancreatic neoplasms. Furthermore, we aimed to investigate the relationship between plasma CgA level and characteristics of PNENs.
We reviewed electronic medical records of Seoul National University Hospital for the patients who had pancreatic tumors in imaging methods and checked plasma CgA between January 2009 and November 2011. Plasma CgA level was measured by ELISA (Cisbio US, Bedford, MA, USA) with a normal range of 24-97 ng/mL. The maximal measurable level of plasma CgA was 760.0 ng/mL.
Patient characteristics including gender, age and plasma CgA level were collected. Histopathologic characteristics including tumor size, tumor location, metastasis, releasing hormones, Ki-67 index and mitotic count were also obtained. Ki-67 index and mitotic count were dichotomized into high and low group by 2% and 2 per 10 high power fields respectively according to 2010 WHO classification of PNENs (16). Exclusion criteria were chronic renal failure, liver failure or the presence of any other malignancy (17, 18).
The cutoffs for diagnosis were identified by receiver-operating characteristic (ROC) curve. The area under the ROC curve (AUC) was calculated to describe the capability of plasma CgA to discriminate between PNENs and controls. The relationships between CgA and clinicopathologic variables were evaluated. The comparisons of values between PNENs and control groups or within PNENs were performed using the Mann-Whitney U test or Fisher's exact test.
A P value of < 0.05 was considered to be statistically significant. Statistical analysis was conducted by using the IBM SPSS Statistics version 19.0 (SPSS Inc, Chicago, IL, USA).
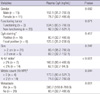
A total of 44 patients were enrolled and the diagnosis for each patient was established by histopathological examination and immunohistochemistry. CgA was elevated above normal range (> 97 ng/mL) in 11 patients. The median CgA level was 81.6 ng/mL and ranged from 22.5 to 760.0 ng/mL. Twenty-six patients had PNENs and 18 patients had other pancreatic diseases (11 pancreatic ductal adenocarcinomas, 2 intraductal papillary mucinous neoplasms, 1 acinic cell carcinomas, 1 solid pseudopapillary neoplasm, 1 myoepithelial hamartoma and 2 autoimmune pancreatitis). There was no significant difference between PNENs and control groups except plasma CgA level (92.9 vs 58.4 ng/mL, P = 0.025, Table 1). However, when excluded 6 patients with distant metastases in PNENs group, there was no significant difference of plasma CgA level between non-metastasis PNENs and control group (80.4 vs 58.4 ng/mL, P = 0.335)
In order to identify the cutoff value of CgA in diagnosing PNENs, ROC analysis was performed among 26 patients with PNENs and 18 controls. The most optimal cutoff value was 60.7 ng/mL with 77% sensitivity and 56% specificity, and the AUC was 0.679 (Fig. 1). Positive predictive value, negative predictive value and accuracy were 71%, 63%, and 68% respectively.
In PNENs group, six patients had metastatic lesions, and CgA was significantly higher in these patients than in those who had no metastasis (380.2 vs 80.4 ng/mL, P = 0.001) (Table 2). The sensitivity and specificity of detecting metastasis were 100% and 90% respectively when CgA cutoff was 156.5 ng/mL, and the AUC was 0.958 (Fig. 2). Positive predictive value, negative predictive value and accuracy were 75%, 100%, and 92% respectively. High Ki-67 index (160.8 vs 62.1 ng/mL, P = 0.001) and mitotic count (173.5 vs 74.6 ng/mL, P = 0.044) were significantly associated with plasma CgA, but tumor size was not (Fig. 3). Immunohistochemical staining of CgA from obtained tissue was performed in 22 patients. Six patients showed weak positive for CgA staining and 16 patients showed positive for CgA staining. However, there was no significant difference in plasma CgA level according to intensity of CgA staining (125.6 vs 80.4 ng/mL, P = 0.417). Plasma CgA level was higher in functioning PNENs than non-functioning PNENs, but showed no statistical significance (534.5 vs 92.3 ng/mL, P = 0.071). There were two gastrinomas and one somatostatin-producing tumor in functioning PNENs. Both plasma CgA levels of the two gastrinomas were 760.0 ng/mL, which was the highest measurable level.
There are some studies identifying the role of plasma CgA as a neuroendocrine neoplasm marker and the diagnostic value of CgA was relatively low (13, 14, 19, 20). Most of the previous studies enrolled all kinds of gastrointestinal neuroendocrine neoplasms because neuroendocrine neoplasms are a rare disease. They compared neuroendocrine neoplasms with healthy subjects as well. Therefore, it is difficult to determine the role of CgA in PNENs with previous studies. In present study, we had included the only patients who were suspected to be PNENs and defined a control group as the patients with pancreatic disease other than PNENs which were ambiguous to distinguish PNENs with diagnostic imaging methods only. This study design made it possible to evaluate the clinical usefulness of CgA in differentiating PNENs.
The diagnostic value of plasma CgA for differentiating PNEN from other pancreatic neoplasm was minimal in this study. The difference of plasma CgA between PNEN and control group was disappeared after excluding six patients with metastases in PNENs group. The sensitivity and the specificity of plasma CgA for diagnosing PNENs were 77% and 56% respectively, when the cutoff was 60.7 ng/mL in this study. This result is consistent with previous reports showing a relatively low diagnostic value of plasma CgA in PNEN, but the specificity of this study was lower (13, 20). This could be explained by incomplete exclusion of the patients with treatment of proton pump inhibitors or chronic atrophic gastritis in this study, which causes high plasma CgA levels (17, 21). However, only 2 patients took proton pump inhibitors at the time of measuring plasma CgA in this study: one had gastrinoma with liver metastasis and the other had nonfunctioning PNEN without metastasis. The plasma CgA levels of 2 patients were 760.0 ng/mL and 147.0 ng/mL respectively.
We found higher plasma CgA levels in metastatic PNEN patients than in those without metastases and this finding is in line with previous studies (20, 22, 23). When the cutoff was 156.5 ng/mL, the sensitivity and the specificity for the presence of metastases were 100% and 90% respectively. Consequently, high plasma CgA level suggests metastases and when CgA is greater than 156.5 ng/mL in patients with PNENs, careful examinations about metastases should be performed. Besides, metastases indicate poor prognosis of PNENs (9, 24). It means plasma CgA would have a clinical emphasis for predicting prognosis.
Plasma CgA was thought to be correlated with tumor volume and disease extent of neuroendocrine neoplasms (13, 14). However, there was no significant correlation between tumor size and plasma CgA level in present study. CgA was significantly associated with Ki-67 index and mitotic count of PNENs. It suggests that plasma CgA might correlate with tumor property rather than quantity. PNEN grading system identifies three different degrees of tumor malignancy basing on Ki-67 index and the major risk factor for progression of PNEN is Ki-67 index (16, 25). On the contrary, tumor size does not indicate prognosis (9), and there was no significant difference in tumor size according to metastases in this study. Thus, it emphasizes that the evaluation of plasma CgA would be helpful in predicting the prognosis of PNENs.
It is controversial whether functioning tumors reflect high plasma CgA level (15, 19). Although CgA was higher in functioning tumors, it showed no statistical difference because there were only three patients with functioning PNENs in this study. Therefore, it is hard to conclude the relationship between functioning tumor and CgA, and would require analyzing plasma CgA of a greater number of patients with functioning PNEN. There were two patients with gastrinoma and both of them had highest plasma CgA level. CgA is known to be much higher in gastrinoma (26). However, we should be careful in interpreting this result because the patients with gastrinoma had taken proton pump inhibitors at the time, which could cause plasma CgA level overestimated.
In conclusion, CgA has little diagnostic value for differentiating PNENs from other pancreatic diseases. However, when CgA level is greater than 156.5 ng/mL in patients with PNENs, metastases should be carefully examined. Also, plasma CgA level correlates with Ki-67 index and mitotic count which represents prognosis of PNENs.
Figures and Tables
Fig. 1
Receiver-operating characteristics curve obtained with 26 patients with pancreatic neuroendocrine tumors and 18 controls. The most optimal cutoff value of chromogranin A was 60.7 ng/mL with 77% sensitivity and 56% specificity, and the area under the curve was 0.679.
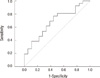
Fig. 2
Receiver-operating characteristics curve obtained with six patients with metastases and 20 patients without metastasis in pancreatic neuroendocrine tumor group. The most optimal cutoff value of chromogranin A was 156.5 ng/mL with 100% sensitivity and 90% specificity, and the area under the curve was 0.958.

Fig. 3
Plasma chromogranin A level according to tumor characteristics in pancreatic neuroendocrine tumors. There are no significant association between chromogranin A and tumor size (A). However, chromogranin A is significantly associated with Ki-67 index (B) and mitotic count (C).

References
1. Mulkeen AL, Yoo PS, Cha C. Less common neoplasms of the pancreas. World J Gastroenterol. 2006. 12:3180–3185.
2. Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008. 26:3063–3072.
3. Halfdanarson TR, Rubin J, Farnell MB, Grant CS, Petersen GM. Pancreatic endocrine neoplasms: epidemiology and prognosis of pancreatic endocrine tumors. Endocr Relat Cancer. 2008. 15:409–427.
4. Cheema A, Weber J, Strosberg JR. Incidental detection of pancreatic neuroendocrine tumors: an analysis of incidence and outcomes. Ann Surg Oncol. 2012. 19:2932–2936.
5. Furukawa T, Tsukamoto Y, Naitoh Y, Mitake M, Hirooka Y, Hayakawa T. Differential diagnosis of pancreatic diseases with an intraductal ultrasound system. Gastrointest Endosc. 1994. 40:213–219.
6. Sakamoto H, Kitano M, Kamata K, El-Masry M, Kudo M. Diagnosis of pancreatic tumors by endoscopic ultrasonography. World J Radiol. 2010. 2:122–134.
7. Eriksson B, Oberg K. Neuroendocrine tumours of the pancreas. Br J Surg. 2000. 87:129–131.
8. Milan SA, Yeo CJ. Neuroendocrine tumors of the pancreas. Curr Opin Oncol. 2012. 24:46–55.
9. Paik WH, Yoon YB, Lee SH, Park JK, Woo SM, Yang KY, Seo JK, Ryu JK, Kim YT. Pancreatic endocrine tumors: clinical manifestations and predictive factors associated with survival. Korean J Gastroenterol. 2008. 52:171–178.
10. Deftos LJ. Chromogranin A: its role in endocrine function and as an endocrine and neuroendocrine tumor marker. Endocr Rev. 1991. 12:181–187.
11. O'Connor DT, Deftos LJ. Secretion of chromogranin A by peptide-producing endocrine neoplasms. N Engl J Med. 1986. 314:1145–1151.
12. Sobol RE, Memoli V, Deftos LJ. Hormone-negative, chromogranin Apositive endocrine tumors. N Engl J Med. 1989. 320:444–447.
13. Nobels FR, Kwekkeboom DJ, Coopmans W, Schoenmakers CH, Lindemans J, De Herder WW, Krenning EP, Bouillon R, Lamberts SW. Chromogranin A as serum marker for neuroendocrine neoplasia: comparison with neuron-specific enolase and the alpha-subunit of glycoprotein hormones. J Clin Endocrinol Metab. 1997. 82:2622–2628.
14. Zatelli MC, Torta M, Leon A, Ambrosio MR, Gion M, Tomassetti P, De Braud F, Delle Fave G, Dogliotti L, degli Uberti EC. Chromogranin A as a marker of neuroendocrine neoplasia: an Italian Multicenter Study. Endocr Relat Cancer. 2007. 14:473–482.
15. Baudin E, Bidart JM, Bachelot A, Ducreux M, Elias D, Ruffié P, Schlumberger M. Impact of chromogranin A measurement in the work-up of neuroendocrine tumors. Ann Oncol. 2001. 12:S79–S82.
16. Rindi G, Klöppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M, Komminoth P, et al. TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006. 449:395–401.
17. Campana D, Nori F, Piscitelli L, Morselli-Labate AM, Pezzilli R, Corinaldesi R, Tomassetti P. Chromogranin A: is it a useful marker of neuroendocrine tumors? J Clin Oncol. 2007. 25:1967–1973.
18. Ferolla P, Faggiano A, Mansueto G, Avenia N, Cantelmi MG, Giovenali P, Del Basso De Caro ML, Milone F, Scarpelli G, Masone S, et al. The biological characterization of neuroendocrine tumors: the role of neuroendocrine markers. J Endocrinol Invest. 2008. 31:277–286.
19. Stivanello M, Berruti A, Torta M, Termine A, Tampellini M, Gorzegno G, Angeli A, Dogliotti L. Circulating chromogranin A in the assessment of patients with neuroendocrine tumours: a single institution experience. Ann Oncol. 2001. 12:S73–S77.
20. Tomassetti P, Migliori M, Simoni P, Casadei R, De Iasio R, Corinaldesi R, Gullo L. Diagnostic value of plasma chromogranin A in neuroendocrine tumours. Eur J Gastroenterol Hepatol. 2001. 13:55–58.
21. Syversen U, Ramstad H, Gamme K, Qvigstad G, Falkmer S, Waldum HL. Clinical significance of elevated serum chromogranin A levels. Scand J Gastroenterol. 2004. 39:969–973.
22. Nobels FR, Kwekkeboom DJ, Bouillon R, Lamberts SW. Chromogranin A: its clinical value as marker of neuroendocrine tumours. Eur J Clin Invest. 1998. 28:431–440.
23. Peracchi M, Conte D, Gebbia C, Penati C, Pizzinelli S, Arosio M, Corbetta S, Spada A. Plasma chromogranin A in patients with sporadic gastro-entero-pancreatic neuroendocrine tumors or multiple endocrine neoplasia type 1. Eur J Endocrinol. 2003. 148:39–43.
24. Tomassetti P, Campana D, Piscitelli L, Casadei R, Santini D, Nori F, Morselli-Labate AM, Pezzilli R, Corinaldesi R. Endocrine pancreatic tumors: factors correlated with survival. Ann Oncol. 2005. 16:1806–1810.
25. Panzuto F, Boninsegna L, Fazio N, Campana D, Pia Brizzi M, Capurso G, Scarpa A, De Braud F, Dogliotti L, Tomassetti P, et al. Metastatic and locally advanced pancreatic endocrine carcinomas: analysis of factors associated with disease progression. J Clin Oncol. 2011. 29:2372–2377.
26. Hirschowitz BI, Worthington J, Mohnen J, Haber M. Chromogranin A in patients with acid hypersecretion and/or hypergastrinaemia. Aliment Pharmacol Ther. 2007. 26:869–878.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download