Abstract
Despite the noninvasiveness and accuracy of multidetector computed tomography (MDCT), its use as a routine screening tool for occult coronary atherosclerosis is unclear. We investigated whether the ratio of apolipoprotein B (apoB) to apolipoprotein A1 (apoA1), an indicator of the balance between atherogenic and atheroprotective cholesterol transport could predict occult coronary atherosclerosis detected by MDCT. We collected the data of 1,401 subjects (877 men and 524 women) who participated in a routine health screening examination of Asan Medical Center. Significant coronary artery stenosis defined as > 50% stenosis was detected in 114 subjects (8.1%). An increase in apoB/A1 quartiles was associated with increased percentages of subjects with significant coronary stenosis and noncalcified plaques (NCAP). After adjustment for confounding variables, each 0.1 increase in serum apoB/A1 was significantly associated with increased odds ratios (ORs) for coronary stenosis and NCAP of 1.23 and 1.18, respectively. The optimal apoB/A1 ratio cut off value for MDCT detection of significant coronary stenosis was 0.58, which had a sensitivity of 70.2% and a specificity of 48.2% (area under the curve, 0.61; 95% CI, 0.58-0.63, P < 0.001). Our results indicate that apoB/A1 ratio is a good indicator of occult coronary atherosclerosis detected by coronary MDCT.
Coronary heart disease (CHD) is one of the leading causes of morbidity and mortality throughout the world. Dyslipidemias, including high low-density lipoprotein cholesterol (LDL-C) and triglyceride (TG) concentrations and low high-density lipoprotein cholesterol (HDL-C) concentration, are risk factors for CHD (1).
Efforts have been made to determine novel lipoprotein abnormalities, other than conventional dyslipidemias, predictive of future cardiovascular diseases (CVD). The ratio of apolipoprotein B (apoB) to apolipoprotein A1 (apoA1), an indicator of the balance between atherogenic and atheroprotective cholesterol transport (2), has been found to be independently associated with CVD (3). This ratio has been shown to predict cardiovascular risk more accurately and more strongly than either apoB or apoA1 alone or any of the other cholesterol indexes (3).
To reduce the morbidity and mortality associated with CHD, efforts have been made to identify subjects at increased risk of CHD. Coronary multidetector computed tomography (MDCT) is an established quantitative and objective method for the noninvasive evaluation of coronary atherosclerosis, which has been widely used diagnostically to detect significant coronary stenosis and/or atherosclerotic plaques (4). Its diagnostic accuracy has been found to be similar to that of the reference standard conventional coronary angiography (5).
Despite the noninvasiveness and accuracy of MDCT, however, its use as a routine screening tool for occult coronary atherosclerosis is unclear, due to radiation exposure and cost-effectiveness. In addition, the specific patient groups who would benefit from coronary MDCT have not yet been determined (6).
To identify the specific patient groups who would benefit from coronary MDCT, we have investigated whether apoB/A1 ratio could predict occult coronary atherosclerosis detected by coronary MDCT and we determined the optimal cut-off value of apoB/A1 ratio in detecting subjects with occult coronary atherosclerosis.
We retrospectively enrolled 1,844 Korean individuals who had undergone coronary CT angiography using 64-slice MDCT and measurements of serum apoB and apoA1 concentrations during general routine health evaluations at the Asan Medical Center (AMC, Seoul, Korea) from January 2008 to December 2009. Each subject completed a questionnaire assessing medications, history of previous medical and/or surgical diseases, and drinking and smoking habits. Drinking habits were categorized as never or rarely, 1-3 times/week, 4-6 times/week, or almost every day; smoking habits were categorized as never, previous or current.
History of CVD was based on each subject's history of angina, myocardial infarction and/or cerebrovascular accidents. Subjects with diabetes were defined as those with fasting plasma glucose (FPG) levels of ≥ 126 mg/dL and/or taking antidiabetic medications. Hypertension was defined as systolic and/or diastolic blood pressures (BP) ≥ 140/90 mmHg or administration of antihypertensive medications. We excluded subjects with chest pain, a history of CVD or percutaneous coronary intervention, or prior coronary arterial bypass surgery (n = 91), as well as those who had taken drugs for more than 6 months or within the previous 12 months that could potentially affect lipid metabolism (n = 200). In addition, subjects with abnormal liver (aspartate aminotransferase, AST and/or alanine aminotransferase, ALT ≥ 2.5 × upper limit of normal value, n = 78), kidney (serum creatinine > 1.5 in men and > 1.4 in women, n = 5) and thyroid function (TSH < 0.4 or > 5.0 mU/L and/or free T4 < 10.3 or > 24.5 pM/L, n = 69) were excluded as liver disease and thyroid disease have been known to be associated with changes in apolipoproteins (7, 8), and decreased renal function could also affect the metabolism of apolipoproteins (9). After exclusion of ineligible subjects, 1,401 participants (877 men, mean age 53.8 ± 9.8 yr; and 524 women, mean age 53.9 ± 9.8) were deemed eligible and were included in this study.
Height and weight were measured while subjects were wearing light clothing without shoes. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Waist circumference (cm) was measured midway between the costal margin and the iliac crest at the end of a normal expiration. BP was measured on the right arm after a rest ≥ 5 min, using an automatic manometer with an appropriate cuff size.
After overnight fasting, early morning blood samples were drawn from the antecubital vein into vacuum tubes and subsequently analyzed by a central, certified laboratory at the AMC. Measurements included the concentrations of uric acid, fasting glucose, insulin, and high-sensitive C-reactive protein (hsCRP) and concentrations of lipid parameters, including apoB and apoA1.
Fasting total cholesterol, HDL-C, LDL-C, TG, and uric acid concentrations were measured by an enzymatic colorimetric method using a Toshiba 200FR Neo (Toshiba Medical System Co., Ltd., Tokyo, Japan). Serum apoB and apoA1 concentrations were measured by a turbidometric method using a Cobas Integra C-6000 analyzer (Roche Diagnostics, Basel, Switzerland), hsCRP concentrations using an immunoturbidimetric method (Toshiba), and FPG concentrations by an enzymatic colorimetric method using a Toshiba 200 FR autoanalyzer (Toshiba). Hemoglobin A1c (HbA1c) concentrations were determined by ionexchange high-performance liquid chromatography (Bio-Rad Laboratories, Inc., Hercules, CA, USA) and serum insulin concentrations by an immunoradiometric assay (TFB Co., Ltd, Tokyo, Japan). Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated as the product of fasting serum insulin (microunits per milliliter) and fasting plasma glucose (millimoles) concentrations, divided by 22.5. All enzyme activities were measured at 37℃.
MDCT examinations were performed using a VCT XT 64-slice MDCT scanner (GE Healthcare, Milwaukee, WI, USA). Subjects with a heart rate > 70 beats/min were given beta-blocking agents before MDCT. A standard scanning protocol was used, with 64 × 0.624 mm slice collimation, 350 ms rotation time, 100-120 kVp tube voltage, and 500-800 mA tube current, according to subject body habitus. All scans were performed using electrocardiogram-gated dose modulation. A bolus of 80 mL iomeprol (Iomeron 400; Bracco, Milan, Italy) was intravenously injected (4 mL/s), followed by a saline flush of 50 mL.
A region of interest was defined on the ascending thoracic aorta, and image acquisition was automatically initiated once a selected threshold (120 Hounsfield units [HU]) was reached, with bolus tracking. Each subject's electrocardiogram was simultaneously recorded to allow for retrospective segmental data reconstruction. Images were initially reconstructed at middiastolic or end-systolic phase of the cardiac cycle. The average radiation dose for MDCT was 4.7 ± 1.6 mSv.
All data were evaluated on a remote workstation (Advantage Workstation; GE Healthcare). Each lesion was identified using a multiplanar reconstruction technique and the maximal intensity projection of short-axis, two-chamber, and four-chamber views. Coronary artery stenosis and plaque characteristics were analyzed on a segmental basis according to American Heart Association criteria (10).
The contrast-enhanced portion of the coronary lumen was semi-automatically traced at the maximal stenotic site and compared with the mean value of the proximal and distal reference sites. Stenosis > 50% was defined as significant.
Plaques were defined as structures > 1 mm2 within and/or adjacent to the vessel lumen. Plaques consisting of calcified tissue occupying more than 50% of the plaque area (density > 130 HU in native scans) were classified as calcified, plaques with < 50% calcium were classified as mixed, and plaques without any calcium were classified as noncalcified lesions (11).
Coronary artery calcium scores (CACS) were measured as described previously (12). Participants, on the basis of the CACS, were categorized in the following manner: no, 0; mild, 0.1 to 100; moderate to severe, > 100.1.
Continuous variables with normal distribution were expressed as mean ± SD, whereas continuous variables with skewed distribution were expressed as median (and interquartile range). Categorical variables were expressed as proportions (%). The apoB/A1 quartiles were Q1 ≤ 0.47, Q2 = 0.48-0.60, Q3 = 0.61-0.74, and Q4 ≥ 0.75. Demographic and biochemical characteristics of the study population assorted according to apoB/A1 quartiles were compared using one-way analysis of variance (ANOVA) or the Kruskal-Wallis test for continuous variables and the chi-square test for categorical variables. The apoB/A1 ratios of subjects with stenosis and without significant stenosis were compared using the unpaired Student's t-test or the Mann-Whitney U-test.
Multivariate logistic regression analysis, after adjustment for confounding variables, was used to calculate the odds ratios (ORs) of apoB/A1 ratio for significant coronary stenosis or plaques. To assess the utility of apoB/A1 ratio as a marker for significant coronary stenosis, we constructed receiver operating characteristics (ROC) curves and calculated the areas under the curve (AUC). The distance on the ROC curve of apoB/A1 was calculated by plotting the sensitivity against (1-specificity). The AUC and the crucial points were determined using Med-Calc® version 11.6.1.0 for Windows (MedCalc Software, Mariakerke, Belgium). All other statistical analyses were performed using SPSS version 14.0 for Windows (SPSS Inc., Chicago, IL, USA). A P value < 0.05 was considered statistically significant.
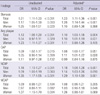
The clinical and biochemical characteristics of the study population classified according to apoB/A1 quartiles are presented in Table 1. We observed positive relationships between apoB/A1 quartiles and BMI, WC, SBP, DBP, FPG, uric acid, total cholesterol, TG, LDL-C, hsCRP, HOMA-IR, and percentages of male subjects and current smokers (P for trend < 0.001 each except for SBP), and a significant negative relationship between apoB/A1 quartiles and HDL-C (P for trend < 0.001). We observed no relationship between apoB/A1 quartiles and the percentages of subjects with diabetes and hypertension.
Significant coronary artery stenosis was detectable in 114 subjects (8.1%), 89 men and 25 women. An increase in apoB/A1 quartiles was associated with an increased percentage of subjects with significant coronary stenosis (P for trend = 0.003, Table 2). Of the 114 patients with significant stenosis, 87 (76.3%) had single-vessel disease. We also observed a positive relationship between apoB/A1 quartiles and increased percentage of subjects with plaques (P for trend = 0.001, Table 2). Among plaque subtypes, only noncalcified plaques (NCAP) differed significantly across the apoB/A1 quartiles (P for trend < 0.001, Table 2). Regarding to CACS, subjects with higher CACS were observed in those with higher apoB/A1 quartiles (P for trend = 0.001, Table 2)
Fig. 1 shows the distribution of apoB/A1 ratios according to the presence of significant coronary stenosis. We found that apoB/A1 ratios were significantly higher in subjects with than without stenosis.
Among the 114 subjects with significant stenosis detected by MDCT, 51 (44.7%, 41 men and 10 women) underwent conventional coronary angiography. Angiography indicated coronary stenosis consistent with the lesions detected by MDCT in 45 subjects (88.2%), but milder coronary stenosis than indicated by MDCT in 6 subjects (11.8%). Revascularization was performed in 31 subjects (68.9%), 28 (62.2%) by percutaneous coronary intervention and 3 (6.7%) by coronary artery bypass surgery.
Table 3 shows the relationship between apoB/A1 ratio and risk of significant coronary stenosis. For each 0.1 increment in apoB/A1 ratio, the ORs for significant stenosis, and any plaques in all subjects increased significantly, even after adjustment for confounding variables such as age, sex, BMI, SBP, DBP, WC, smoking and drinking habits, hypertension, diabetes, FPG, hsCRP and HOMA-IR. Multivariate analysis showed that, among plaque subtypes, only NCAP showed a significant association with apoB/A1 ratio. When we calculated the ORs for significant coronary stenosis in men and women separately, we observed significance only in men (Table 3).
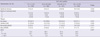
ROC analysis revealed that the optimal apoB/A1 ratio cutoff for detecting significant coronary stenosis by MDCT was 0.58, which had a sensitivity of 70.2% and a specificity of 48.2% (Fig. 2, AUC, 0.61; 95% CI, 0.58-0.63, P < 0.001). Using this cut-off value, the OR for significant coronary stenosis was 2.06 (95% CI, 1.31-3.24, P = 0.002) after adjusting for age, sex, BMI, SBP, DBP, WC, smoking and drinking habits, hypertension, diabetes, FPG, hsCRP and HOMA-IR.
We assessed the association between serum apoB/A1 ratios and significant coronary artery stenosis, as determined by MDCT, in a large number of Koreans without typical chest pain and/or a previous history of CVD. Furthermore, we attempted to determine the optimal apoB/A1 ratio to identify subjects who might benefit from coronary MDCT. To our knowledge, this is the first study to investigate the ability of serum apoB/A1 ratios to predict coronary atherosclerosis detected by coronary MDCT. We found that an increase in serum apoB/A1 ratio was associated with significant coronary atherosclerosis and NCAP, independent of conventional risk factors. In addition, we found that an apoB/A1 ratio > 0.58 was optimal for identifying subjects with significant coronary atherosclerosis by MDCT.
Atherosclerosis is a diffuse pathological process characterized by the deposition of lipids and other blood-borne materials within the arterial wall of almost all vascular territories (13). Cholesterol accumulation within vascular walls plays a central role in atherogenesis (13). Although, lipid abnormalities have been considered major risk factors for the development of CHD, many individuals who develop CHD have normal serum lipid concentrations (14). Apolipoproteins play pivotal roles in cholesterol transport and metabolism (2), and apoB/A1 ratio, a marker of the balance between proatherogenic and antiatherogenic lipoproteins (2), may be a good indicator of atherosclerosis including coronary artery disease.
A high apoB/A1 ratio has been shown to be good marker of future CVD, including myocardial infarction and stroke (3, 15). Moreover, this ratio has been shown to be a better indicator than any other lipid measurements, including conventional lipid ratios, of the presence and/or severity of coronary artery disease detected by conventional coronary angiography (16-18). However, despite the close relationship between serum apoB/A1 ratio and CHD detected by conventional coronary angiography, no previous study attempted to determine the optimal apoB/A1 cut-off value for identifying the subjects with significant coronary stenosis, especially using coronary MDCT.
Approximately 3%-5% of asymptomatic individuals have coronary artery disease (19, 20), and about 5.2% of asymptomatic individuals have significant coronary artery stenosis, as detected by MDCT (21). In comparison, we found that 8.1% of our subjects had significant stenosis on MDCT. Of these subjects, 27.2% underwent revascularization via percutaneous coronary intervention or coronary artery bypass surgery. These findings indicate the importance of identifying asymptomatic individuals who are at high risk for CHD, in preventing future morbidity and mortality.
The recent introduction of 64-slice MDCT has enabled the noninvasive characterization of atherosclerotic lesions and the determination of luminal and vessel wall alterations (22). MDCT has been shown to have a high diagnostic accuracy as compared with invasive coronary angiography (23). In addition, MDCT allowed us to recognize the plaque burden in subjects with normal perfusion (24, 25). However, despite these advantages and accuracy, its routine use for screening of occult CHD is controversial due to its radiation exposure and cost-effectiveness. Despite this controversy, it is currently widely used as a screening tool for CHD in Korea (26). Furthermore, the prevalence of occult CHD in apparently healthy individuals was not negligible (21). In this background, our study attempted to use apoB/A1 ratios to identify groups of subjects who might benefit from MDCT.
We found that serum apoB/A1 ratios were associated with the presence of plaques, especially NCAPs. Although the amount of calcified plaque (CAP) is highly related to overall plaque burden, CAP represents only about 20% of the total atherosclerotic plaque burden (27), and has been associated with advanced stages of atherosclerosis; in contrast, NCAPs are considered a feature of early atherosclerosis (28). Furthermore, there is increasing evidence suggesting that NCAPs may be associated with acute coronary syndrome (29, 30). Although no study to date has investigated the association between serum apoB/A1 ratio and the type of coronary plaques, our results indicate that serum apoB/A1 ratio may be especially useful in detecting lesions with early atherosclerosis.
We observed positive relationships between apoB/A1 quartiles and BMI, WC, and smoking habits, in agreement with previous results showing that BMI, waist-to-hip ratio, and cigarette smoking were positively correlated with apoB and negatively correlated with apoA1 concentrations (31). Even after adjusting for these confounding factors, however, we observed an independent association between elevated apoB/A1 ratio and significant coronary stenosis on MDCT.
There are many advantages to measuring serum apoB and apoA1 concentrations. For example, these measurements do not require samples from fasting individuals (32). In addition, the methods used to measure apoB and apoA1 have been internationally standardized in reference materials from the World Health Organization and the International Federation of Clinical Chemistry and Laboratory Medicine (32). Therefore, measurement of serum apoB/A1 ratio may be easily accessible for detecting subjects at risk for occult CHD.
Our study had several limitations. First, due to its cross-sectional design, we could not determine whether there was a causal relationship between apoB/A1 ratio and coronary artery stenosis. Second, participants were relatively healthy, and although large numbers were analyzed, only small percentages, especially of women, had significant stenosis on MDCT. Third, the study population consisted exclusively of Koreans, so our results may not be applicable to other ethnic groups. Forth, MDCT only reflects the anatomic severity, not functional ischemia and it has limitation in judging the vulnerability of plaque (33). Finally, as we did not perform conventional coronary angiography in all subjects with significant stenosis on MDCT, we may have overdiagnosed significant coronary stenosis. This possibility was unlikely, however, due to the 88.2% concordance rate we observed between conventional coronary angiography and MDCT.
In conclusion, our results indicate that apoB/A1 ratio is a good indicator of occult coronary atherosclerosis detected by coronary MDCT and that subjects with apoB/A1 ratio greater than 0.58 are good candidates for coronary MDCT.
Figures and Tables
 | Fig. 1Box-whisker plots of apoB/A1 ratios according to the presence of significant coronary stenosis in total subjects (A), men (B), and women (C). The ends of each whisker indicate the 5th and 95th percentiles of apoB/A1 ratio. |
 | Fig. 2Receiver operating characteristic (ROC) curve and optimal apoB/A1 ratio cutoff value (•) for detecting significant coronary stenosis by multidetector computed tomography (MDCT). |
Table 1
Baseline patient characteristics according to apoB/A1 ratio quartiles

BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; LDL-C, low density lipoprotein-cholesterol; HDL-C, high density lipoprotein-cholesterol; ApoB, apolipoprotein B; ApoA1, apolipoprotein A1; hsCRP, high sensitive C-reactive protein; HOMA-IR, homeostasis model of insulin resistance.
References
1. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
2. Marcovina S, Packard CJ. Measurement and meaning of apolipoprotein AI and apolipoprotein B plasma levels. J Intern Med. 2006. 259:437–446.
3. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART Study): case-control study. Lancet. 2004. 364:937–952.
4. Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006. 114:1761–1791.
5. Foster G, Shah H, Sarraf G, Ahmadi N, Budoff M. Detection of noncalcified and mixed plaque by multirow detector computed tomography. Expert Rev Cardiovasc Ther. 2009. 7:57–64.
6. Achenbach S, Daniel WG. Current role of cardiac computed tomography. Herz. 2007. 32:97–107.
7. Peppa M, Betsi G, Dimitriadis G. Lipid abnormalities and cardiometabolic risk in patients with overt and subclinical thyroid disease. J Lipids. 2011. 2011:575840.
8. Seidel D. Lipoproteins in liver disease. J Clin Chem Clin Biochem. 1987. 25:541–551.
9. Batista MC, Welty FK, Diffenderfer MR, Sarnak MJ, Schaefer EJ, Lamon-Fava S, Asztalos BF, Dolnikowski GG, Brousseau ME, Marsh JB. Apolipoprotein A-I, B-100, and B-48 metabolism in subjects with chronic kidney disease, obesity, and the metabolic syndrome. Metabolism. 2004. 53:1255–1261.
10. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB. A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975. 51:5–40.
11. Leber AW, Becker A, Knez A, von Ziegler F, Sirol M, Nikolaou K, Ohnesorge B, Fayad ZA, Becker CR, Reiser M, et al. Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol. 2006. 47:672–677.
12. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990. 15:827–832.
13. Badimon JJ, Ibanez B, Cimmino G. Genesis and dynamics of atherosclerotic lesions: implications for early detection. Cerebrovasc Dis. 2009. 27:38–47.
14. Holmes DR Jr, Elveback LR, Frye RL, Kottke BA, Ellefson RD. Association of risk factor variables and coronary artery disease documented with angiography. Circulation. 1981. 63:293–299.
15. Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet. 2001. 358:2026–2033.
16. Noma A, Yokosuka T, Kitamura K. Plasma lipids and apolipoproteins as discriminators for presence and severity of angiographically defined coronary artery disease. Atherosclerosis. 1983. 49:1–7.
17. Reinhart RA, Gani K, Arndt MR, Broste SK. Apolipoproteins A-I and B as predictors of angiographically defined coronary artery disease. Arch Intern Med. 1990. 150:1629–1633.
18. Enkhmaa B, Anuurad E, Zhang Z, Pearson TA, Berglund L. Usefulness of apolipoprotein B/apolipoprotein A-I ratio to predict coronary artery disease independent of the metabolic syndrome in African Americans. Am J Cardiol. 2010. 106:1264–1269.
19. Thaulow E, Erikssen J, Sandvik L, Erikssen G, Jorgensen L, Cohn PF. Initial clinical presentation of cardiac disease in asymptomatic men with silent myocardial ischemia and angiographically documented coronary artery disease (the Oslo Ischemia Study). Am J Cardiol. 1993. 72:629–633.
20. Pilote L, Pashkow F, Thomas JD, Snader CE, Harvey SA, Marwick TH, Lauer MS. Clinical yield and cost of exercise treadmill testing to screen for coronary artery disease in asymptomatic adults. Am J Cardiol. 1998. 81:219–224.
21. Choi EK, Choi SI, Rivera JJ, Nasir K, Chang SA, Chun EJ, Kim HK, Choi DJ, Blumenthal RS, Chang HJ. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol. 2008. 52:357–365.
22. Schuijf JD, van Werkhoven JM, Pundziute G, Jukema JW, Decramer I, Stokkel MP, Dibbets-Schneider P, Schalij MJ, Reiber JH, van der Wall EE, et al. Invasive versus noninvasive evaluation of coronary artery disease. JACC Cardiovasc Imaging. 2008. 1:190–199.
23. Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, Decramer I, Van Hoe LR, Wijns W, Hunink MG. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology. 2007. 244:419–428.
24. Hacker M, Jakobs T, Hack N, Nikolaou K, Becker C, von Ziegler F, Knez A, König A, Klauss V, Reiser M, et al. Sixty-four slice spiral CT angiography does not predict the functional relevance of coronary artery stenoses in patients with stable angina. Eur J Nucl Med Mol Imaging. 2007. 34:4–10.
25. Schuijf JD, Wijns W, Jukema JW, Atsma DE, de Roos A, Lamb HJ, Stokkel MP, Dibbets-Schneider P, Decramer I, De Bondt P, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006. 48:2508–2514.
26. Nam HJ, Jung IH, Kim J, Kim JH, Suh J, Kim HS, Kim HK, Jung YJ, Kang JW, Lee S. Association between brachial-ankle pulse wave velocity and occult coronary artery disease detected by multi-detector computed tomography. Int J Cardiol. 2012. 157:227–232.
27. Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation. 1995. 92:2157–2162.
28. Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: a report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1995. 92:1355–1374.
29. Hoffmann U, Moselewski F, Nieman K, Jang IK, Ferencik M, Rahman AM, Cury RC, Abbara S, Joneidi-Jafari H, Achenbach S, et al. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol. 2006. 47:1655–1662.
30. Fujii K, Kobayashi Y, Mintz GS, Takebayashi H, Dangas G, Moussa I, Mehran R, Lansky AJ, Kreps E, Collins M, et al. Intravascular ultrasound assessment of ulcerated ruptured plaques: a comparison of culprit and nonculprit lesions of patients with acute coronary syndromes and lesions in patients without acute coronary syndromes. Circulation. 2003. 108:2473–2478.
31. Kinlay S, Dobson AJ, Heller RF, Dickeson JE, Ryan S. Lipid and apolipoprotein levels in an Australian community. Med J Aust. 1991. 154:170–175.
32. Marcovina SM, Albers JJ, Kennedy H, Mei JV, Henderson LO, Hannon WH. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B: IV. comparability of apolipoprotein B values by use of International Reference Material. Clin Chem. 1994. 40:586–592.
33. Waxman S, Ishibashi F, Muller JE. Detection and treatment of vulnerable plaques and vulnerable patients: novel approaches to prevention of coronary events. Circulation. 2006. 114:2390–2411.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download