Abstract
The aim of this study was to determine antimicrobial susceptibility of recent clinical Stenotrophomonas maltophilia isolates from Korea, and to compare the activity levels of several combinations of antimicrobials. A total of 206 non-duplicate clinical isolates of S. maltophilia was collected in 2010 from 11 university hospitals. Antimicrobial susceptibility testing was performed using the Clinical Laboratory Standards Institute agar dilution method. In vitro activity of antimicrobial combinations was tested using the checkerboard method. The susceptibility rates to trimethoprim-sulfamethoxazole and minocycline were 96% and 99%, respectively. The susceptibility rate to levofloxacin was 64%. All of four antimicrobial combinations showed synergy against many S. maltophilia isolates. A combination of trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate was most synergistic among the combinations. None of the combinations showed antagonistic activity. Therefore, some of the combinations may be more useful than individual drugs in the treatment of S. maltophilia infection. Further clinical studies are warranted to validate our in vitro test results.
Stenotrophomonas maltophilia is an environmental global emerging Gram-negative multiple-drug-resistant organism that is most commonly associated with respiratory infections (1). Isolation of S. maltophilia from human specimens may represent colonization rather than infection. Although not highly virulent, S. maltophilia can infect immunocompromised hosts and hospitalized patients being predisposed to infection (2). The mortality rates ranged from 14% to 69% in patients with bacteremia by S. maltophilia (3, 4). S. maltophilia exhibits high-level intrinsic resistance to a broad spectrums of antibiotics, including β-lactams, quinolones, aminoglycosides, tetracycline, disinfectants, and heavy metals (5, 6). S. maltophilia can also acquire resistance through the uptake of resistance genes located integrons, transposons, and plasmids (7). Therefore, infections caused by S. maltophilia are particularly difficult to manage because they show resistance to many classes of antimicrobial agents. The recommended therapeutic agents for S. maltophila infection is trimethoprim-sulfamethoxazole by the evidences of case reports and in vitro susceptibility studies (2). Recently, combinations of antimicrobials have been recommended as treatment for S. maltophilia infection, especially in severe septic, neuropenic, debilitated or immunocompromised patients, or when trimethoprim-sulfamethoxazole cannot be used or tolerated (2, 8, 9). However, there is no study focused on the antimicrobial activity of the antibiotics combinations to S. maltophilia in Korea.
The aim of this study was to determine antimicrobial susceptibility of recent clinical S. maltophilia isolates from Korea, and to compare the activity levels of several combinations of antimicrobials.
A total of 206 non-duplicate clinical isolates of S. maltophilia were collected in 2010 from 11 university hospitals. The species were identified using conventional methods and/or the VITEK2 system (bioMerieux, Marcy l'Etoile, France). Among the 206 isolates, 30 were selected for the checkerboard method based on susceptibility: 10 isolates with resistant to trimethoprim-sulfamethoxazole, 26 with resistant to ceftazidime, 22 with nonsuceptible to ticarcillin-clavulanate, and 25 with nonsusceptible to levofloxacin.
Antimicrobial susceptibility testing was performed using the CLSI agar dilution method (10). The antimicrobial agents used were trimethoprim-sulfamethoxazole (Dong Wha, Seoul, Korea), levofloxacin (Daiichi, Tokyo, Japan), moxifloxacin (Bayer Korea, Seoul, Korea), minocycline (SK Chemicals Life Science, Seoul, Korea), tigecycline (Wyeth Research, Pearl River, NY, USA), ceftazidime (Sigma Chemical, St. Louis, MO, USA), ticarcillin-clavulanate (Dong-A, Yongin, Korea), chloramphenicol (Chong Kun Dang, Seoul, Korea), and amikacin (Sigma Chemicals). The breakpoints recommended by CLSI for S. maltophilia were applied to interpret the minimum inhibitory concentrations (MICs) (10). Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as controls.
In vitro activity of antimicrobial combinations was tested by the checkerboard method. The antimicrobial combinations tested were trimethoprim-sulfamethoxazole + ticarcillin-clavulanate, levofloxacin + ceftazidime, ceftazidime + amikacin, and ticarcillin-clavulanate + amikacin. Fractional inhibitory concentration (FIC) index was calculated according to the following formula:
The FIC indices were interpreted as follows: ≤ 0.5, synergistic; > 0.5 to 4, indifferent; > 4, antagonistic (11).
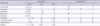
MIC ranges, MIC50s, MIC90s, and the percentages of resistant isolates for various antimicrobial agents are shown in Table 1. The MIC of trimethoprim-sulfamethoxazole ranged from ≤ 0.06 to 128 µg/mL, and the MIC50 and MIC90 were 1 and 2 µg/mL, respectively. The susceptibility rate was 96%. The MIC of levofloxacin ranged from 0.12 to 64 µg/mL, and the MIC50 and MIC90 were 2 and 16 µg/mL, respectively, which were higher than those of moxifloxacin (0.5 and 8 µg/mL, respectively). The resistance rate to levofloxacin was 20%. The MIC50 and MIC90 of minocycline were 0.5 and 2 µg/mL, respectively, and only one isolate was resistant to minocycline (the resistance rate < 1%). The MICs of tigecycline ranged from ≤ 0.06 to 8 µg/mL, and the MIC50 and MIC90 were 1 and 4 µg/mL, respectively, which were two-fold higher than those of minocycline. The MIC50 of amikacin was > 128 µg/mL. The MIC50 of ceftazidime 64 µg/mL and the resistance rate was 71%. The MIC50 of ticarcillin-clavulanate was 32 µg/mL and the resistance rate was 24%. The MIC range of chloramphenicol was 8-128 µg/mL, the MIC50 and MIC90 were 16 and 64 µg/mL, restectively. The resistance rate to chloramphenicol was 49%.
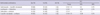
All of four antimicrobial combinations showed synergy against many S. maltophilia isolates. A combination of trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate was most synergistic among the combinations. FIC index of a combination of ticarcillin-clavulanate plus amikacin was 0.38 for 50% of S. maltophilia isolates. None of the combinations showed antagonistic activity (Table 2). The FIC index for synergistic S. maltophilia ranged 0.09 to 0.5.
Antimicrobial combinations of trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate, ceftazidime plus amikacin, and ticarcillin-clavulanate plus amikacin were synergistic for majority of trimethoprim-sulfamethoxazole-resistant isolates. Trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate demonstrated synergy for the four trimethoprim-sulfamethoxazole-resistant isolates with high MIC levels of trimethoprim-sulfamethoxazole (≥ 64 µg/mL), but MIC values of trimethoprim-sulfamethoxazole did not decrease below susceptibility breakpoints (16-32 µg/mL). On the other hand, synergistic FICs were not found against the two trimethoprim-sulfamethoxazole-resistant isolates with low MIC levels of trimethoprim-sulfamethoxazole (4 µg/mL), but MICs of trimethoprim-sulfamethoxazole in combination with ticarcillin-clavulanate were within susceptible range. Trimethoprim-sulfamethoxazole MICs of trimethoprim-sulfamethoxazole-susceptible isolates for trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate became 2 to 8-fold lower than those used alone (data not shown).
Trimethoprim-sulfamethoxazole showed the lowest MIC90 (2 µg/mL) and the isolates showed a high susceptibility rate of 96% to this agent. Trimethoprim-sulfamethoxazole is still considered the treatment of choice for suspected or culture-proven S. maltophilia infections. Resistance rates to trimethoprim-sulfamethoxazole have been reported to vary geographically, which were generally less than 10% (2, 12, 13). In this study, all hospitals showed low resistance rate of 5%-10% except one hospital (26%). Some studies with isolates from cystic fibrosis patients and from some Asian countries, such as Taiwan and Turkey, showed high resistance rates (31.3%-100%) (13-25).
In this study, the resistance rate to levofloxacin was 20%, which was higher than the rates of 3% to 11% seen in previous studies (13, 20, 21, 26). Especially, three of hospitals showed high resistance rates over 30%. MIC90 of levofloxacin was also higher than our previous study (27). Moxifloxacin was more active than levofloxacin considering low MICs. Moxifloxacin could be suggested as an alternative to levofloxacin. Further clinical studies are necessary to evaluate the effectiveness of moxifloxacin in treating S. maltophilia infections, because there is little data published on the clinical efficacy of moxifloxacin.
The tetracycline derivatives minocycline and tigecycline have shown good in vitro activity against clinical isolates of S. maltophilia, but there is little clinical data for treating S. maltophilia infections (28, 29). In this study, two isolates were intermediate and one isolate were resistant to minocycline. But, minocycline shows highest in vitro activity against S. maltophilia strains, and this data was similar to that of Taiwan, Brazil, Spain, and the USA (16, 21, 22, 30). MICs of tigecycline ranged from ≤ 0.06 to 8 µg/mL, and MIC50 and MIC90 were 1 and 4 µg/mL, respectively. Antimicrobial susceptibilities of a worldwide collection of 1,586 S. maltophilia tested against tigecycline, MIC50 and MIC90 of tigecycline were 0.5 and 2 µg/mL (31). The tigecycline in vitro surveillance in Taiwan collected a total of 903 S. maltophilia, MIC range of tigecycline was from 0.13 to 16 µg/mL, and MIC50 and MIC90 were 2 and 4 µg/mL (32).
The rates of susceptibility to ceftazidime and ticarcillin-clavulanate were similar with other studies (13-25). The β-lactams and/or β-lactamase inhibitor combinations show little activity against S. maltophilia, because the organism has a high intrinsic resistance to most penicillins and cephalosporins, and to all carbapenems (7). Chloramphenicol showed similar resistant rate with previous reports, but much lower susceptibility rate due to high intermediate rate (45%) (15, 19, 21, 23).
Considering of the highest MIC, amikacin demonstrated the least active drug to S. maltophilia among the tested drugs. The aminoglycosides show poor activity against S. maltophilia because of high intrinsic resistance and therefore is not useful in monotherapy (7).
Because of historical evidence, case reports and high in vitro susceptibility rates, cotrimoxazole is usually considered the treatment of choice for S. maltophilia infection (2). However, increasing resistance to cotrimoxazole and the alternate antimicrobials may cause problems for the empirical treatment of S. maltophilia infections. Therefore, combination therapy may be indicated in the setting of severe sepsis, neutropenia or polymicrobial infections, but clinical evidence is still lacking (2, 7). Combination therapy may be more practical when cotrimoxazole therapy is contraindicated. We assessed the activity of four antimicrobial combinations by the checkerboard method, since these combinations had been reported to have synergistic effects to S. maltophilia (7). Synergistic effect was demonstrated by all combinations (34%-66%) (Table 2). Synergy for trimethoprim-sulfamethoxazole resistant S. maltophilia isolates were shown by trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate (4/6), ceftazidime plus amikacin (4/6), and ticarcillin-clavulanate plus amikacin (5/6).
Poulos et al. (33) demonstrated synergy between trimethoprim-sulfamethoxazole and ticarcillin-clavulanic acid by the chequerboard method and by the time-kill assay in 19 different trimethoprim-sulfamethoxazole-resistant strains. In our study, synergistic activities by trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate were shown in 67% of trimethoprim-sulfamethoxazole-resistant S. maltophilia, MIC values of trimethoprim-sulfamethoxazole were not decreased below susceptible breakpoint. Likewise, other antimicrobial combinations (ceftazidime plus amikacin, ticarcillin-clavulanate plus amikacin) were synergistic, MIC value of each antibiotic agent sometimes was not clearly decreased (data not shown). Antibiotics for combination therapy should be chosen on the basis of in vitro susceptibility test (7). Therefore, it is uncertain and needs to be evaluated that combination therapy with trimethoprim-sulfamethoxazole plus ticarcillin-clavulanate inhibit the growth in vivo of trimethoprim-sulfamethoxazole resistant S. maltophilia.
Although the choice of monotherapy or combination therapy is a controversial issue, several authors suggest combination treatment, especially in patients at risk (2, 7). Synergy testing may help determine the most appropriate combination in each special setting, but the problem is a lack of standardization of the techniques to determine synergy (34). Clinical data of in vivo combination therapy should be warranted.
Figures and Tables
ACKNOWLEDGMENTS
The microorgnisms were provided by the National Biobank of Korea - Chonbuk National University Hospital, which is supported by the Ministry of Health, Welfare and Family Affairs. All materials derived from the National Biobank of Korea were obtained with informed consent under institutional review board-approved protocols. The authors have no conflicts of interest to disclose.
References
1. Brooke JS. Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev. 2012. 25:2–41.
2. Abbott IJ, Slavin MA, Turnidge JD, Thursky KA, Worth LJ. Stenotrophomonas maltophilia: emerging disease patterns and challenges for treatment. Expert Rev Anti Infect Ther. 2011. 9:471–488.
3. Jang TN, Wang FD, Wang LS, Liu CY, Liu IM. Xanthomonas maltophilia bacteremia: an analysis of 32 cases. J Formos Med Assoc. 1992. 91:1170–1176.
4. Victor MA, Arpi M, Bruun B, Jonsson V, Hansen MM. Xanthomonas maltophilia bacteremia in immunocompromised hematological patients. Scand J Infect Dis. 1994. 26:163–170.
5. Zhang L, Li XZ, Poole K. Multiple antibiotic resistance in Stenotrophomonas maltophilia: involvement of a multidrug efflux system. Antimicrob Agents Chemother. 2000. 44:287–293.
6. Alonso A, Martinez JL. Multiple antibiotic resistance in Stenotrophomonas maltophilia. Antimicrob Agents Chemother. 1997. 41:1140–1142.
7. Looney WJ, Narita M, Muhlemann K. Stenotrophomonas maltophilia: an emerging opportunist human pathogen. Lancet Infect Dis. 2009. 9:312–323.
8. Liaw SJ, Teng LJ, Hsueh PR, Ho SW, Luh KT. In vitro activities of antimicrobial combinations against clinical isolates of Stenotrophomonas maltophilia. J Formos Med Assoc. 2002. 101:495–501.
9. Muder RR, Harris AP, Muller S, Edmond M, Chow JW, Papadakis K, Wagener MW, Bodey GP, Steckelberg JM. Bacteremia due to Stenotrophomonas (Xanthomonas) maltophilia: a prospective, multicenter study of 91 episodes. Clin Infect Dis. 1996. 22:508–512.
10. Clinical Laboratory and Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Twenty-first Informational Supplement. 2011. Wayne:
11. Odds FC. Synergy, antagonism, and what the chequerboard puts between them. J Antimicrob Chemother. 2003. 52:1.
12. Gales AC, Jones RN, Forward KR, Linares J, Sader HS, Verhoef J. Emerging importance of multidrug-resistant Acinetobacter species and Stenotrophomonas maltophilia as pathogens in seriously ill patients: geographic patterns, epidemiological features, and trends in the SENTRY Antimicrobial Surveillance Program (1997-1999). Clin Infect Dis. 2001. 32:Suppl 2. S104–S113.
13. Sader HS, Jones RN. Antimicrobial susceptibility of uncommonly isolated non-enteric Gram-negative bacilli. Int J Antimicrob Agents. 2005. 25:95–109.
14. Fedler KA, Biedenbach DJ, Jones RN. Assessment of pathogen frequency and resistance patterns among pediatric patient isolates: report from the 2004 SENTRY Antimicrobial Surveillance Program on 3 continents. Diagn Microbiol Infect Dis. 2006. 56:427–436.
15. Laing FP, Ramotar K, Read RR, Alfieri N, Kureishi A, Henderson EA, Louie TJ. Molecular epidemiology of Xanthomonas maltophilia colonization and infection in the hospital environment. J Clin Microbiol. 1995. 33:513–518.
16. Wang WS, Liu CP, Lee CM, Huang FY. Stenotrophomonas maltophilia bacteremia in adults: four years' experience in a medical center in northern Taiwan. J Microbiol Immunol Infect. 2004. 37:359–365.
17. San Gabriel P, Zhou J, Tabibi S, Chen Y, Trauzzi M, Saiman L. Antimicrobial susceptibility and synergy studies of Stenotrophomonas maltophilia isolates from patients with cystic fibrosis. Antimicrob Agents Chemother. 2004. 48:168–171.
18. Saiman L, Chen Y, Gabriel PS, Knirsch C. Synergistic activities of macrolide antibiotics against Pseudomonas aeruginosa, Burkholderia cepacia, Stenotrophomonas maltophilia, and Alcaligenes xylosoxidans isolated from patients with cystic fibrosis. Antimicrob Agents Chemother. 2002. 46:1105–1107.
19. Betriu C, Sanchez A, Palau ML, Gomez M, Picazo JJ. Antibiotic resistance surveillance of Stenotrophomonas maltophilia, 1993-1999. J Antimicrob Chemother. 2001. 48:152–154.
20. Zhanel GG, DeCorby M, Nichol KA, Wierzbowski A, Baudry PJ, Karlowsky JA, Lagace-Wiens P, Walkty A, Mulvey MR, Hoban DJ. Antimicrobial susceptibility of 3931 organisms isolated from intensive care units in Canada: Canadian National Intensive Care Unit Study, 2005/2006. Diagn Microbiol Infect Dis. 2008. 62:67–80.
21. Valdezate S, Vindel A, Loza E, Baquero F, Canton R. Antimicrobial susceptibilities of unique Stenotrophomonas maltophilia clinical strains. Antimicrob Agents Chemother. 2001. 45:1581–1584.
22. Vartivarian S, Anaissie E, Bodey G, Sprigg H, Rolston K. A changing pattern of susceptibility of Xanthomonas maltophilia to antimicrobial agents: implications for therapy. Antimicrob Agents Chemother. 1994. 38:624–627.
23. Nicodemo AC, Araujo MR, Ruiz AS, Gales AC. In vitro susceptibility of Stenotrophomonas maltophilia isolates: comparison of disc diffusion, Etest and agar dilution methods. J Antimicrob Chemother. 2004. 53:604–608.
24. Weiss K, Restieri C, De Carolis E, Laverdiere M, Guay H. Comparative activity of new quinolones against 326 clinical isolates of Stenotrophomonas maltophilia. J Antimicrob Chemother. 2000. 45:363–365.
25. Travassos LH, Pinheiro MN, Coelho FS, Sampaio JL, Merquior VL, Marques EA. Phenotypic properties, drug susceptibility and genetic relatedness of Stenotrophomonas maltophilia clinical strains from seven hospitals in Rio de Janeiro, Brazil. J Appl Microbiol. 2004. 96:1143–1150.
26. Wu H, Wang JT, Shiau YR, Wang HY, Yang Lauderdale TL, Chang SC. A multicenter surveillance of antimicrobial resistance on Stenotrophomonas maltophilia in Taiwan. J Microbiol Immunol Infect. 2012. 45:120–126.
27. Chung HS, Hong SG, Lee Y, Kim M, Yong D, Jeong SH, Lee K, Chong Y. Antimicrobial susceptibility of Stenotrophomonas maltophilia isolates from a Korean tertiary care hospital. Yonsei Med J. 2012. 53:439–441.
28. Belvisi V, Fabietti P, Del Borgo C, Marocco R, Di Vincenzo E, Soscia F, Mastroianni CM. Successful treatment of Stenotrophomonas maltophilia soft tissue infection with tigecycline: a case report. J Chemother. 2009. 21:367–368.
29. Blanquer D, De Otero J, Padilla E, Gomez F, Mayol A, Irigaray R, Espejo P, Rada MA, Makrantoni G, Perez AR. Tigecycline for treatment of nosocomial-acquired pneumonia possibly caused by multi-drug resistant strains of Stenotrophomonas maltophilia. J Chemother. 2008. 20:761–763.
30. Galles AC, Jones RN, Sader HS. Antimicrobial susceptibility profile of contemporary clinical strains of Stenotrophomonas maltophilia isolates: can moxifloxacin activity be predicted by levofloxacin MIC results? J Chemother. 2008. 20:38–42.
31. Farrell DJ, Sader HS, Jones RN. Antimicrobial susceptibilities of a worldwide collection of Stenotrophomonas maltophilia isolates tested against tigecycline and agents commonly used for S. maltophilia infections. Antimicrob Agents Chemother. 2010. 54:2735–2737.
32. Chen YH, Lu PL, Huang CH, Liao CH, Lu CT, Chuang YC, Tsao SM, Chen YS, Liu YC, Chen WY. Trends in the susceptibility of clinically important resistant bacteria to tigecycline: results from the Tigecycline In Vitro Surveillance in Taiwan study, 2006 to 2010. Antimicrob Agents Chemother. 2012. 56:1452–1457.
33. Poulos CD, Matsumura SO, Willey BM, Low DE, McGeer A. In vitro activities of antimicrobial combinations against Stenotrophomonas (Xanthomonas) maltophilia. Antimicrob Agents Chemother. 1995. 39:2220–2223.
34. Gulmez D, Cakar A, Sener B, Karakaya J, Hascelik G. Comparison of different antimicrobial susceptibility testing methods for Stenotrophomonas maltophilia and results of synergy testing. J Infect Chemother. 2010. 16:322–328.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download