Abstract
Cervical disc herniation is a common disorder characterized by neck pain radiating to the arm and fingers as determined by the affected dermatome. This condition has a favorable prognosis, but pain can have a serious detrimental impact on daily activities. Epidural neuroplasty has been applied as a treatment option for cervical disc herniation; however, no study has addressed the clinical outcomes. This retrospective study evaluated the clinical outcomes of epidural neuroplasty on 128 patients for the treatment of cervical disc herniation. To measure pain-related disabilities over time, the changes of pain scores in neck and arm were evaluated using a numerical rating scale (NRS) and the neck disability index (NDI). Compared with preprocedural values, the pain NRS of neck and arm demonstrated significant improvement at day 1, and 1, 3, 6, and 12 months after the procedure (P < 0.001). Likewise, the NDI was significantly reduced at 3, 6, and 12 months after the procedure (P < 0.001). There were no serious complications. Cervical epidural neuroplasty shows good clinical outcomes in the treatment of cervical disc herniation and can be considered a treatment modality for cervical disc herniation refractory to conservative treatment.
Cervical radicular pain is a common disorder characterized by neck pain radiating to the arm and fingers, as determined by the dermatome involved. The most common causes of cervical nerve root compression are spondylosis and cervical disc herniation (1).
Generally, degenerative cervical radicular pain has a favorable prognosis and responds to nonsurgical treatments such as physical rehabilitation, oral anti-inflammatory medication, and minimal intervention, including the 'wait and see' approach (2-4). However, pain in the neck and arm can substantially impair physical and mental functions, and this kind of persistent pain can have a negative impact on mental health (1).
Various treatment modalities, such as cervical interlaminar epidural injections (5), physiotherapy and a cervical collar (6), and percutaneous cervical nucleoplasty (7), have been used to treat cervical radicular pain, and all of these treatment options have been shown to produce moderate to good clinical results. Lumbar epidural neuroplasty is now an established and commonly used treatment modality for the management of chronic low back pain and sciatica due to lumbar disc protrusion or prolapse, or failed back surgery syndrome (8). Cervical epidural neuroplasty was derived from lumbar epidural neuroplasty and has been applied as a treatment option for cervical disc herniation (CDH) (9). However, no study has yet addressed the effectiveness of epidural neuroplasty for CDH. This study was performed to demonstrate the clinical outcomes of epidural neuroplasty for the treatment of CDH.
We retrospectively analyzed the data from 128 patients who underwent epidural neuroplasty for the treatment of a cervical disc herniation at our hospital from August, 2009 to June, 2011.
Inclusion criteria for this study were patients having: symptoms of unilateral radicular pain with or without axial neck pain; cervical disc herniations with concordant radicular pain demonstrated by magnetic resonance imaging (MRI) and/or computed tomography (CT); a numerical rating scale (NRS, 0-100) of 70 or more after appropriate conservative treatment for at least 6 weeks in the form of medication, physiotherapy, and nerve blocks such as epidural interlaminar steroid injections or a nerve root block. Exclusion criteria were patients having: a lack of correlation between radicular symptoms and the level of disc herniation on MRI; and prior spinal surgery, clinical signs of spinal cord compression, bleeding tendency, instability, spondylolisthesis, spinal canal stenosis, ossification of a longitudinal ligament and other traumatic injuries, associated somatic or psychiatric disease, or an underlying systemic disease.
All patients completed the 12-month follow-up, which was conducted through an interview with a physician with responses recorded on the questionnaire chart. The outcomes were measured using the numerical rating scale (NRS) that ranged from 0 (no pain) to 100 (worst pain imaginable), from which the patient selected the number most representative of their pain. In addition, the neck disability index (NDI) was determined for each patient using a self-administrated questionnaire, which had been shown to be reliable, valid and sensitive. The NDI was used to measure neck-related disabilities, including pain intensity and headache, and the ability to perform activities including personal care, lifting, reading, concentrating, working, driving, sleeping, and participating in recreational activities (10, 11). The NDI was calculated as the summation of scores from each of the above 10 items, which ranged from 0 (no activity limitation) to 5 (major activity limitation).
We evaluated the NRS on a preprocedural day, on postprocedural day-1, and after 1, 3, 6, and 12 months after epidural neuroplasty. When a postprocedural NRS was > 50, the patient received an additional single cervical epidural injection; 12 patients received an additional injection 1 month after epidural neuroplasty. NDIs were assessed using a self-administered questionnaire given preprocedurally and postprocedurally at 3, 6, and 12 months after epidural neuroplasty. Overall patient satisfaction was evaluated using the modified MacNab criteria, and categorized as excellent, good, fair, or poor during the final follow-up.
Epidural neuroplasty was performed as previously described by Viesca et al. (9). Briefly, the patient was placed in the prone position on a fluoroscopic table. An epidural needle was placed in C7-T1 or T1-T2 under local anesthesia and advanced to the cervical epidural space using the "loss of resistance" technique. Epidurography was performed to confirm the needle position. The VERSA-KATH® radio-opaque epidural catheter (Epimed International Inc, Johnstown, NY, USA) was placed directly onto the herniated disc level under fluoroscopic control, and 2 to 3 mL of Omnipaque 240 (nonionic contrast) was injected. After confirming the proper position of the catheter tip, hyaluronidase (5 mL containing 1,500 units) in preservative-free normal saline (0.9%) was injected (Fig. 1). An additional small amount of dye was injected to check for anylysis of adhesion, and then 5 mL of a mixture of 0.2% ropivacaine plus 5 mg of dexamethasone was administered slowly. During the drug administration, the patient's head was rotated from side to side to prevent the accumulation of the injectate in the epidural cavity and to enlarge the neural foramina for allowing the injectate to escape (12, 13).
The Pearson's chi-square test was used to determine the statistical significance of qualitative variables and Student's t-test was used to compare quantitative variables. The paired t-test was used for comparing pre- and post-treatment average NRS and NDI scores at pre-epidural neuroplasty against 3, 6, and 12 months after epidural neuroplasty. The analysis was conducted using SPSS version 15 (SPSS Inc., Chicago, IL, USA), and P values of < 0.05 were considered to indicate statistical significance.
In total, 80 males and 48 females completed the 12-month follow-up, and the mean patient age was 47 yr (standard deviation [SD] 7.9; range 29 to 69 yr). The mean duration of pre-procedural pain was 8.2 weeks (SD 2.6; range 6 to 20 weeks), with 63 patients having right-sided pain and 65 having left-sided pain. The most frequently involved nerve root level was C6 (59 patients; 46.1%) followed by C7 (54 patients; 42.1%) (Table 1). The mean duration of medication after epidural neuroplasty was 3.9 weeks (SD 1.8) (Table 2).
Neck pain and arm pain were scored separately. The pre-procedural mean neck and arm pain scores were 73.0 and 77.0 (NRS, 0-100), respectively, and the NRS showed significant improvements at 1-day (42.2 and 44.7), 1 month (25.4 and 24.2), 3 months (14.0 and 9.1), 6 months (9.7 and 5.5), and 12 months (8.3 and 4.1) (post-procedural versus pre-procedural values, P < 0.001) (Table 3). Compared to the pre-procedural mean NDI scores (17.5), the postprocedural mean NDI scores were significantly reduced at 3 months (4.5), 6 months (2.8), and 12 months (2.3) (P < 0.001) (Table 4).
Of the 128 patients, five with a poor outcome converted to open cervical discectomy during the follow-up period. The patient satisfaction at 12 months after the procedure, measured according to the modified MacNab criteria, was excellent in 57 patients (44.5%), good in 65 patients (50.8%), and poor in one patient (0.8%). No serious complications occurred in this series during the short-term and long-term follow-ups.
This is the first study to evaluate the clinical outcomes of epidural neuroplasty in the treatment of CDH. The present study found that epidural neuroplasty in the treatment of CDH resulted in dramatic reductions in neck and arm pain at 1 day after the procedure, and that these improvements were maintained at 12 months after epidural neuroplasty. The functional outcome as measured by NDI scores showed significant improvement at 3, 6, and 12-month follow-ups compared with pretreatment values. Of 123 patients (five were excluded because they underwent surgical treatment), 65 patients achieved complete pain resolution at 12 months after epidural neuroplasty. The remaining 57 patients had average NRS scores from 5 to 30; however, their satisfaction measurements using the Modified MacNab criteria were excellent or good, indicating their ability to perform their normal activities. Only one patient had an average NRS of 50 and her satisfaction value was poor.
Cervical radicular pain is a common condition, with approximately one person in 1,000 suffering from this condition (14). The exact pathogenesis of this pain is unclear, but the development is generally considered to be due to a combination of compression and an inflammatory response of some kind. Furthermore, the blood vessels of compressed nerve roots show increased permeability, which secondarily results in nerve root edema. Chronic edema and fibrosis within a nerve root can alter its response threshold and increase sensitivity to pain (15). Cervical epidural neuroplasty is a minimally invasive and safe therapy that involves the placement of a catheter directly at the herniated disc or scar tissue compromising a nerve root (8). The technique was derived from lumbar epidural neuroplasty and has been adopted as a treatment option for cervical disc herniation (9). This procedure produces good results and has been associated with only minor complications in the treatment of low back pain and radiculopathy (16). In our study, no serious complications occurred during the short-term and long-term follow-ups, and only 2 of 128 patients showed transient vasovagal syncope during the procedure. However, Talu and Erdine (17) concluded that this procedure must be performed by experienced hands in well-equipped centers. Evaluating the immediate and prolonged complications in a total of 250 cases of epidural neuroplasty, they reported several complications, including the tip of the needle bending during entry to the epidural space, sheared catheter remnants remaining in the epidural space, hypotension, and numbness.
The prognosis of CDH can be exceedingly good if no permanent neurological malfunction has occurred; however, 27% of patients experience a persistent degree of neck disability (18). Kuijper et al. (6) carried out a randomized clinical study in 205 patients who presented with symptoms and signs of cervical radiculopathy. Of these patients, 69 were allocated to a semi-hard cervical collar, 70 to standardized physiotherapy, and 66 to a control group treated on a 'wait and see' basis. This study determined that a semi-hard cervical collar and rest for 3 to 6 weeks or physiotherapy accompanied by home exercises for 6 weeks substantially reduced neck and arm pain as compared to the 'wait and see' policy during the early phase. However, treatment did not appear to influence outcome after a follow-up of 6 months. In a comparative clinical trial, Persson et al. (19) compared surgery, physiotherapy, and a cervical collar in patients with cervical radiculopathy. It was found that surgery was superior for pain relief at 4 months, but no difference was found between the three groups in terms of pain intensity, muscle weakness, or sensory loss at 16 months. DePalma and Subin (20) followed one conservatively treated group (n = 255) and one surgically treated group (n = 75) for 1 yr. In the former group, 29% obtained complete relief and 49% improved, whereas 64% in the surgery group were rated as excellent for pain, muscle strength, and sensory loss, and 21% were rated as improved. However, after an additional year, no significant differences were found between the two groups with respect to pain and other sensory disturbances. In a prospective multicenter study, a substantial number of patients who underwent surgery (26%) reported persistent excruciating pain at follow-ups (21). Compared to the average pre-procedural neck NRS score of 73.0 and arm NRS score of 77.0, our study results showed rapid pain reduction at 1-day after the epidural neuroplasty procedure, with neck and arm NRS values of 42.2 and 44.7, respectively, and 95.3% patients with excellent or good satisfaction at the 12-month follow-up.
As mentioned above, inflammatory reactions appear to play important roles in the mechanism responsible for radicular pain (15), and the rationale underlying epidural corticosteroid administration addresses the anti-inflammatory response induced by the inhibition of the phospholipase A2-initiated arachidonic acid cascade (14). Interlaminar and transforaminal injections are common methods for delivering corticosteroid to the epidural space, and Huston (22) reviewed the efficacy, complications, side-effects, and techniques for the two methods. To improve the efficacy of epidural corticosteroid, the transforaminal route has been recommended to deposit the drug near the nerve root in the anterior epidural space, at the interface between a herniated disc or foraminal stenosis and inflamed nerve roots (23). However, several cases of severe neurological disability and even fatal spinal cord infarction have been reported after transforaminal epidural steroid injection (14, 24). Nevertheless, a retrospective cohort study conducted by Botwin et al. (25) concluded that fluoroscopically guided interlaminar cervical epidural injections are safe in patients with cervical radicular pain, based on the low incidence of complications observed and the absence of major complications in their study. Furthermore, Abbasi et al. (26) concluded that when an interlaminar cervical epidural steroid injection is correctly carried out in a cooperative patient using fluoroscopy and contrast medium, the incidence of complications is low. In the present study, no serious complications were encountered. Nevertheless, to ensure the safety of epidural neuroplasty and to maximize its therapeutic benefits, fluoroscopic guidance and great care are required (27).
Cervical radicular pain caused by root compression due to spondylosis or disc herniation is a common cause of neck and arm pain, and has considerable impact on the overall health status of an individual (1). Importantly, almost 5% of affected adults are substantially disabled by neck pain during any 6-month period (28). Ektor-Andersen et al. (29) reported that self-reported health scores decreased with increasing pain in the shoulder-neck area. In the present study, NDI scores were significantly reduced from a mean pre-procedural value of 17.5 to 4.47 and 2.25 at 3 and 12 months after the procedure, respectively (P < 0.001). Accordingly, our findings suggest that epidural neuroplasty dramatically improves the functional status at short- and long-term follow-up.
Our study has several limitations. This was a retrospective study and the lack of a control group is a limitation. Cervical radicular pain is an extremely painful condition, and it is practically difficult to manage patients with conservative treatment only. And we performed an additional cervical epidural injection when a postprocedural NRS was > 50; 12 patients received an additional injection at 1 month after epidural neuroplasty. Also, our patients had been taking oral medication including nonsteroidal anti-inflammatory agents and muscle relaxants for an average of 3.9 weeks after the procedure. Despite these limitations, this study demonstrates the clinical outcomes of cervical epidural neuroplasty for the treatment of cervical disc herniation.
In conclusion, we evaluated for the first time the clinical outcomes of epidural neuroplasty in the treatment of CDH. Cervical epidural neuroplasty is an effective and safe procedure for the treatment of CDH. In cases of normal neurological function, we recommend epidural neuroplasty as the next-step treatment modality in the treatment of CDH refractory to conservative treatment.
Figures and Tables
 | Fig. 1Antero-posterior fluoroscopic view showing a catheter inserted in the affected neural foramen. The contrast dye fully escapes via lateral runoff through the neural foramen along the neural sheath after proper adhesiolysis. |
Table 1
Demographic data of 128 patients treated for cervical disc herniation by epidural neuroplasty
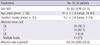
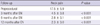
Table 2
Clinical features of 128 patients treated for cervical disc herniation by epidural neuroplasty
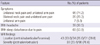
Table 3
Longitudinal changes in neck and arm pain NRS scores in 123 patients
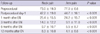
Of a total of 128 patients, five were excluded because they underwent surgical treatment. A significant improvement was observed at post-procedural day-1, and 1, 3, 6, and 12 months after epidural neuroplasty versus pre-procedural values (P < 0.001). EN, epidural neuroplasty; NRS, numerical rating scale.
References
1. Daffner SD, Hilibrand AS, Hanscom BS, Brislin BT, Vaccaro AR, Albert TJ. Impact of neck and arm pain on overall health status. Spine (Phila Pa 1976). 2003. 28:2030–2035.
2. Vinas FC, Wilner H, Rengachary S. The spontaneous resorption of herniated cervical discs. J Clin Neurosci. 2001. 8:542–546.
3. Bush K, Chaudhuri R, Hillier S, Penny J. The pathomorphologic changes that accompany the resolution of cervical radiculopathy: a prospective study with repeat magnetic resonance imaging. Spine (Phila Pa 1976). 1997. 22:183–186.
4. Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine (Phila Pa 1976). 1996. 21:1877–1883.
5. Benyamin RM, Singh V, Parr AT, Conn A, Diwan S, Abdi S. Systematic review of the effectiveness of cervical epidurals in the management of chronic neck pain. Pain Physician. 2009. 12:137–157.
6. Kuijper B, Tans JT, Beelen A, Nollet F, de Visser M. Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomised trial. BMJ. 2009. 339:b3883.
7. Li J, Yan DL, Zhang ZH. Percutaneous cervical nucleoplasty in the treatment of cervical disc herniation. Eur Spine J. 2008. 17:1664–1669.
8. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 2006. 11:365–369.
9. Viesca CO, Racz GB, Day MR. Special techniques in pain management: lysis of adhesions. Anesthesiol Clin North America. 2003. 21:745–766.
10. Ackelman BH, Lindgren U. Validity and reliability of a modified version of the neck disability index. J Rehabil Med. 2002. 34:284–287.
11. Hoving JL, O'Leary EF, Niere KR, Green S, Buchbinder R. Validity of the neck disability index, Northwick Park neck pain questionnaire, and problem elicitation technique for measuring disability associated with whiplash-associated disorders. Pain. 2003. 102:273–281.
12. Kitagawa T, Fujiwara A, Kobayashi N, Saiki K, Tamai K, Saotome K. Morphologic changes in the cervical neural foramen due to flexion and extension: in vivo imaging study. Spine (Phila Pa 1976). 2004. 29:2821–2825.
13. Racz GB, Heavner JE. Cervical spinal canal loculation and secondary ischemic cord injury: PVCS: perivenous counter spread: danger sign! Pain Pract. 2008. 8:399–403.
14. Van Zundert J, Huntoon M, Patijn J, Lataster A, Mekhail N, van Kleef M. Pain Practice. 4. cervical radicular pain. Pain Pract. 2010. 10:1–17.
15. Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: pathophysiology, natural history, and clinical evaluation. J Bone Joint Surg Am. 2002. 84-A:1872–1881.
16. Heavner JE, Racz GB, Raj P. Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 1999. 24:202–207.
17. Talu GK, Erdine S. Complications of epidural neuroplasty: a retrospective evaluation. Neuromodulation. 2003. 6:237–247.
18. Lees F, Turner JW. Natural history and prognosis of cervical spondylosis. Br Med J. 1963. 2:1607–1610.
19. Persson LC, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar: a prospective, controlled study. Eur Spine J. 1997. 6:256–266.
20. DePalma AF, Subin DK. Study of the cervical syndrome. Clin Orthop Relat Res. 1965. 38:135–142.
21. Sampath P, Bendebba M, Davis JD, Ducker T. Outcome in patients with cervical radiculopathy: prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976). 1999. 24:591–597.
22. Huston CW. Cervical epidural steroid injections in the management of cervical radiculitis: interlaminar versus transforaminal: a review. Curr Rev Musculoskelet Med. 2009. 2:30–42.
23. Kolstad F, Leivseth G, Nygaard OP. Transforaminal steroid injections in the treatment of cervical radiculopathy: a prospective outcome study. Acta Neurochir (Wien). 2005. 147:1065–1070.
24. Malhotra G, Abbasi A, Rhee M. Complications of transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2009. 34:731–739.
25. Botwin KP, Castellanos R, Rao S, Hanna AF, Torres-Ramos FM, Gruber RD, Bouchlas CG, Fuoco GS. Complications of fluoroscopically guided interlaminar cervical epidural injections. Arch Phys Med Rehabil. 2003. 84:627–633.
26. Abbasi A, Malhotra G, Malanga G, Elovic EP, Kahn S. Complications of interlaminar cervical epidural steroid injections: a review of the literature. Spine (Phila Pa 1976). 2007. 32:2144–2151.
27. Yadla S, Malone J, Campbell PG, Maltenfort MG, Harrop JS, Sharan AD, Ratliff JK. Early complications in spine surgery and relation to preoperative diagnosis: a single-center prospective study. J Neurosurg Spine. 2010. 13:360–366.
28. Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey: the prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998. 23:1689–1698.
29. Ektor-Andersen J, Isacsson SO, Lindgren A, Orbaek P. The experience of pain from the shoulder-neck area related to the total body pain, self-experienced health and mental distress: the Malmö Shoulder-Neck Study group. Pain. 1999. 82:289–295.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download