Abstract
This study aimed to elucidate the demographic and sleeping environmental factors associated with sudden infant death syndrome (SIDS) in Korea. The autopsy reports of all SIDS cases reported to the National Forensic Service and Seoul National University College of Medicine between 1996 and 2008 were reviewed for data collection and analysis to identify the risk factors for SIDS. Analysis of the 355 SIDS cases reported within the study period revealed that of the 168 (47.3%) cases for which sleeping position before death had been reported, 75 (44.7%) cases had occurred after placement in prone or side position. Of the 204 (57.5%) cases for which bed-sharing situation had been reported, 121 (59.3%) deaths had occurred during bed-sharing, of which 54 (44.6%) infants were under 3 months of age, a significantly younger age than that of the non-bed-sharing cases (P = 0.0279). Analysis of the results indicated no tendency toward an increase or decrease in the use of a prone or side position. Rather, there was a statistically significant increasing trend for bed-sharing over the study period (OR, 1.087; 95% CI, 1.004-1.177; P = 0.04). These findings indicate the need for nationwide educational programs promoting a safe sleeping environment to enhance SIDS prevention.
Sudden infant death syndrome (SIDS) is a diagnosis of exclusion defined as "the sudden death of an infant under one year of age that remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene and review of the clinical history" (1). Although the cause of death should be diagnosed as SIDS only after a thorough examination has been conducted, many cases have been diagnosed as SIDS despite failure to fulfill all the criteria for SIDS diagnosis. To address this problem, the medical community established the diagnosis sudden unexpected death in infancy (SUDI), defined as sudden unexpected death occurring before 12 months of age (2). Analysis of epidemiological data has elucidated modifiable risk factors for SIDS, including the placement of an infant to sleep in certain positions, specifically in a prone or side position, on certain surfaces, particularly on a soft surface, or in a bed with one or more other individuals, as well as the exposure of an infant to nicotine via maternal smoking before birth and second-hand smoke after birth (3-5). Since the identification of these risk factors, the prevalence of SIDS has declined substantially. Nevertheless, SIDS remains the leading cause of death of infants under one year of age in many countries (6-8), having been reported to be the cause of death of between 0.1 and 0.8 per 1000 live births in developed countries (3).
Although many epidemiological reviews of SIDS prevalence have been conducted in an international context, no coronial investigation has been conducted in a Korean context. To fill this research gap, this study reviewed cases of SIDS referred by the National Forensic Service and Seoul National University College of Medicine for autopsy from 1996 to 2008 to identify demographic and sleeping environmental factors that may be risk factors for SIDS.
The SIDS cases analyzed were selected from review of the records of the National Forensic Service and Seoul National University College of Medicine. The inclusion criteria for all cases were age 8 to 364 days at time of death and sudden and unexpected death. The reports of all cases were reviewed by two forensic pathologists. Any cases for which a specific cause of death was subsequently established at autopsy were excluded. The data collected included time of death, position when found deceased, position placed to sleep before death, and sleeping surface. Data were also collected regarding whether the SIDS occurred during bed-sharing, defined as a specific type of co-sleeping pattern in which an infant sleeps with another individual on the same surface (9), and, if so, whether the individual with whom the infant was sleeping had consumed alcohol prior to sharing a bed with the deceased infant. Fisher's exact test was used to compare categorical variables when comparable data were available. The temporal changes of bed-sharing and sleeping position were evaluated using logistic regression model and multinomial logistic regression models, respectively. A P value < 0.05 was considered significant. Statistical tests were performed using SPSS version 17 (SPSS Inc. Chicago, IL, USA).
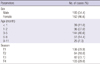
Table 1 shows the demographic data regarding the SIDS cases reviewed. Regarding the number of cases, 355 post-mortems were classified as SIDS between 1996 and 2008, and although no significant trend regarding an increase or decrease in the number of cases could be identified over the study period, 209 (58.9%) SIDS cases were observed in the winter and spring seasons. Regarding the characteristics of the cases, 193 (54.4%) male and 162 (46.6%) female cases diagnosed as SIDS occurred at a median age of 17 weeks, with 135 cases (38.0%) of SIDS occurring under 3 months of age. Among the 193 cases (54.4%) for which maternal age had been reported, the median maternal age was 28 yr (range 18 to 43 yr). Of the 183 cases (51.5%) for which feeding pattern had been reported, 23 infants (14.2%) had been breastfed, 140 (76.5%) had been fed powdered formula, and 17 (9.3%) had been both breastfed and fed powdered formula.
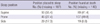
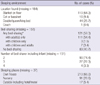
Of 293 SIDS cases for which time when found deceased was known, 109 infants (37.2%) had been discovered between 0601 and 1200h, 71 (23.2%) between 1201 and 1800h, 43 (14.7%) between 1801 and 2400h, and 70 (23.9%) between 2401 and 0600h. Of the 168 (47.3%) of cases for which sleeping position before death had been reported, 75 (44.7%) cases had been placed in a prone or side sleeping position, among which 49.8% had been found in a prone position at the time of death (Table 2). Analysis of the data indicated no tendency toward an increase or decrease in placement in a prone or side sleeping position over the study period (OR, 1.090; 95% CI, 0.960-1.243; P = 0.178) (Fig. 1). As can be observed in Table 3, which shows the data regarding sleeping environment, only 9.4% of infants had been placed to sleep in a bed intended for infants only, such as a cot or bassinet, with the majority being found in a blanket on the floor or in an adult bed. This finding reflects a Korean tradition of placing an infant on a blanket over a Korean-style floor (ondol).
Among the cases for which bed-sharing had been reported, 121 (59.3%) of deaths had occurred in a bed-sharing situation. Of the cases who had died during bed-sharing, 54 (44.6%) cases had been under 3 months of age, a significantly greater number than those who had died while not bed-sharing (P = 0.028). Thirty one (25.6%) of bed-sharing SIDS deaths had occurred during bed-sharing with 2 or more individuals and 21 (17.4%) cases had occurred during bed-sharing with an individual under the influence of alcohol. There was a statistically significant increasing trend (OR, 1.087; 95% CI, 1.004-1.777; P = 0.04) in bed-sharing over the study period (Fig. 2). Of the 52 infants who had been placed in a supine position before death, 28 had been bed-sharing with 1 or more individuals. Regarding the reason for bed-sharing, breastfeeding was reported for 34 (22.5%) cases of all SIDS.
Several international studies have found that the promotion of "back-to-sleep" campaigns based on the findings of many epidemiological studies has led to a dramatic decrease in the global prevalence of SIDS over the last 2 decades (10, 11). However, few studies have examined the prevalence of SIDS specifically within Korea (12, 13), and no coronial data regarding SIDS in Korea have been reported. To redress this lack of research within a Korean context, we examined the factors associated with SIDS cases that had been reported to the National Forensic Services and Seoul National University College of Medicine, the majority of which had occurred in the Seoul-Gyeonggi region of Korea, between 1996 and 2008.
Analysis of the data indicates that the majority of the deaths due to SIDS had occurred while the infants had been sleeping in a hazardous sleep environment. While many were found in a prone sleeping position, which has been reported as one of the established risk factors for SIDS (10), a recent study reported that risk of SIDS in a side position is of a similar magnitude to that of a prone position (14). The risk posed by sleeping in a side position might be due to its inherent instability, as it allows the infant to easily move into a prone position. Therefore, the American Academy of Pediatrics (AAP) strongly recommends that infants always be placed in a supine sleeping position (15). Among the cases in this study, 55.4% (93 cases) had been placed to sleep in a prone position, a rate much higher than rates previously reported, which range from 13% to 43% (16-20), and 17.3% (29 cases) in a side position. Analysis of the data indicated no tendency toward a change in sleeping position to the recommended position (supine) over the 13-yr study period.
Interestingly, 34% (108 cases) of the SIDS analyzed in this study occurred outside the home, including in a nursery/daycare setting or a relative's accommodation, indicating increased risk of SIDS outside the parental residence. This might be due to infants who sleep outside the home being placed in a sleep environment not specifically arranged for infants and/or being placed in a prone position. The study data support this hypothesis, as analysis of the difference between the prevalence in which the infants in this study had been placed in a prone sleeping position in a setting outside the home compared to that in which they had been placed in a prone position in the home was found to be statistically significant (P = 0.002).
Among the cases for which bed-sharing had been reported, the prevalence of bed-sharing was 59.3% (121 cases), a much higher rate than those found in cohort-based studies, which range from 16.0% to 50.4% (21-24). This finding might be explained by cultural factors, such as a Korean belief that bedsharing enables breastfeeding and emotional bonding, and supported by the finding that 22.5% (34 cases) of the mothers in this study reported breast-feeding as the reason for bed-sharing. However, bed-sharing is a known risk factor for SIDS, especially for infants under 3 months of age, infants who share a bed with an individual under the influence of alcohol, and infants who are subjected to bed-sharing for long durations (4, 11). Analysis of the data revealed that 44.6% (54 cases) for which bed-sharing had been reported had been under 3 months of age, a percentage that is statistically significant when compared to that of the non-bed-sharing cases and comprising approximately 69.2% of all cases for which bed-sharing had been reported under 3 months of age. Surprisingly, 17.4% (21 cases) occurred while bed-sharing with adult(s) who were under the influence of alcohol, a factor that may have undermined the ability to respond to the infant. Indeed, several studies have reported a strong association between alcohol consumption prior to bed-sharing and SIDS (4, 25). Furthermore, there was a significantly increasing trend in bed-sharing over 13-yr study period, suggesting that parents and caregivers should be provided with information regarding bed-sharing as a means to decrease the risk of SIDS. This suggestion is supported by the AAP, which recommends that infants in the first year should sleep in their own bed, ideally a bassinet or crib placed in the parental room (15), as well as the findings of this study, specifically that only 16 (9.4%) infants had been sleeping in their own bed.
Regarding other risk and protective factors, a recent meta-analysis study reported that exclusive breast-feeding of any duration is protective against SIDS (26). The prevalence of exclusive breast-feeding in this study was found to be 14.2%, a rate slightly higher than the 10.2% domestic rate reported in 2002 (27). Unfortunately, accurate data regarding maternal smoking, which has been identified as a dependent risk factor contributing to SIDS (28) and the main risk factor for SIDS during bed-sharing (11), could not be collected.
The exact pathogenesis of SIDS remains poorly understood. Accumulating evidence has linked SIDS to a convergence of exogenous stressors, including non-recommended (prone or side) sleeping position, a critical development period in homeostatic condition, and dysfunction of cardiopulmonary and/or arousal system (29). A recent study found a significant association between SIDS and mutations in the cardiac ion-channel protein giving rise to disease, including Long QT Syndrome (LQTS) and Brugada Syndrome, in 10 to 15% of SIDS cases (30). Although there is no evidence of strong heritability for SIDS, the genetic alteration that has been observed could lead to vulnerability to SIDS (3, 29, 30). Thus, continued research into the interaction between genetic and environmental factors is critical for SIDS prevention.
A 2004 study using the capture-recapture method to examine the 1998 and 1999 data estimated the rate of SIDS in Korea to be 0.56 per 1,000 live births (12). However, this estimation is questionable due to lack of scientific validity in diagnosis, with many cases having been diagnosed as SIDS without postmortem examination and death scene investigation. Although autopsies are critical in identifying the cause of death whenever an infant dies suddenly from unknown causes, the autopsy rate in Korea, which is unknown, is presumed to be extremely low compared to those of other developed countries (3).
Due to its retrospective design, this study faced a major limitation in data collection. Although a postmortem protocol for SIDS autopsy had been introduced in 2001, it was not widely used until 2006. Therefore, many data regarding parental smoking, sleeping surface, and breathing at time of death (i.e., whether the face had been covered) were unavailable for cases that occurred before 2006. In contrast, significantly more and better data were available after 2006 because of increased awareness of the environmental risk factors associated with SIDS and increased use of the postmortem protocol.
The findings of this study have crucial implications for health policymaking and practices. Specifically, they indicate the need to develop, adopt, and implement 1) a set of standardized guidelines for SIDS diagnosis; 2) a protocol for the collection of detailed data from medical doctors, scene investigators, caregivers, and medical examiners to determine the precise cause of death; and 3) monitoring systems to collect data with which to identify trends in SIDS prevalence. Moreover, they suggest that educational campaigns for SIDS prevention, which have traditionally-and effectively-emphasized avoidance of bed-sharing and placement in a prone position-should also stress avoidance of all risk factors and be conducted on a nationwide scale using all means of information distribution, including those provided by governmental, media, and medical sources.
In conclusion, this first coronial study of SIDS in Korea found that a considerable proportion of deaths due to SIDS occurred while the infants had been sleeping in an environment characterized by risk factors for SIDS, particularly placement in a prone or side position and/or in a bed-sharing situation. This finding strongly suggests that immediate focus should be placed on making the sleeping environment safer for the next generation.
Figures and Tables
Fig. 1
Annual distribution of positions placed to sleep before death in autopsy-diagnosed Sudden Infant Death Syndrome (SIDS) cases.

Fig. 2
Annual distribution of bed-sharing in autopsy-diagnosed Sudden Infant Death Syndrome (SIDS) cases.

ACKNOWLEDGMENTS
We thank to Jae Kwon Kim (Department of Forensic Medicine, the Catholic University of Korea Medical School) and Hyun Chul Kim for organizing and digitalizing data, and all members of National Forensic Service for their assistance in providing the data for this study. The authors have no conflicts of interest to disclose.
References
1. Willinger M, James LS, Catz C. Defining the sudden infant death syndrome (SIDS): deliberations of an expert panel convened by the National Institute of Child Health and Human Development. Pediatr Pathol. 1991. 11:677–684.
2. Shapiro-Mendoza CK, Tomashek KM, Anderson RN, Wingo J. Recent national trends in sudden, unexpected infant deaths: more evidence supporting a change in classification or reporting. Am J Epidemiol. 2006. 163:762–769.
3. Moon RY, Horne RS, Hauck FR. Sudden infant death syndrome. Lancet. 2007. 370:1578–1587.
4. Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, Jorch G, Schreuder P. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004. 363:185–191.
5. Ruys JH, de Jonge GA, Brand R, Engelberts AC, Semmekrot BA. Bed-sharing in the first four months of life: a risk factor for sudden infant death. Acta Paediatr. 2007. 96:1399–1403.
6. Overpeck MD, Brenner RA, Cosgrove C, Trumble AC, Kochanek K, MacDorman M. National underascertainment of sudden unexpected infant deaths associated with deaths of unknown cause. Pediatrics. 2002. 109:274–283.
7. Martin JA, Kung HC, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, Sutton SR. Annual summary of vital statistics: 2006. Pediatrics. 2008. 121:788–801.
8. Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Hansen SH, Svendsen JH, Haunsø S, Tfelt-Hansen J. Sudden unexpected death in infancy in Denmark. Scand Cardiovasc J. 2011. 45:14–20.
9. McKenna JJ, Ball HL, Gettler LT. Mother-infant cosleeping, breastfeeding and sudden infant death syndrome: what biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am J Phys Anthropol. 2007. 45:133–161.
10. Mitchell EA. The changing epidemiology of SIDS following the national risk reduction campaigns. Pediatr Pulmonol Suppl. 1997. 16:117–119.
11. Blair PS, Sidebotham P, Evason-Coombe C, Edmonds M, Heckstall-Smith EM, Fleming P. Hazardous cosleeping environments and risk factors amenable to change: case-control study of SIDS in south west England. BMJ. 2009. 339:b3666.
12. Ha M, Yoon SJ, Lee HY, Goh UY, Kim CH, Lee YS. Estimation of the incidence of sudden infant death syndrome in Korea: using the capture-recapture method. Paediatr Perinat Epidemiol. 2004. 18:138–142.
13. Moon YO, Choi HK, Her JA, Shin WJ, Kim MA, Lee SY, Jang SH, Dong ES, Kim CJ, Ahn YM, et al. Sudden unexpected death in infancy: analysis of 34 cases including 13 autopsies. J Korean Pediatr Soc. 2002. 45:1065–1074.
14. Li DK, Petitti DB, Willinger M, McMahon R, Odouli R, Vu H, Hoffman HJ. Infant sleeping position and the risk of sudden infant death syndrome in California, 1997-2000. Am J Epidemiol. 2003. 157:446–455.
15. Task Force on Sudden Infant Death Syndrome. Moon RY. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011. 128:e1341–e1367.
16. Escott A, Elder DE, Zuccollo JM. Sudden unexpected infant death and bedsharing: referrals to the Wellington Coroner 1997-2006. N Z Med J. 2009. 122:59–68.
17. Hutchison BL, Rea C, Stewart AW, Koelmeyer TD, Tipene-Leach DC, Mitchell EA. Sudden unexpected infant death in Auckland: a retrospective case review. Acta Paediatr. 2011. 100:1108–1112.
18. Senter L, Sackoff J, Landi K, Boyd L. Studying sudden and unexpected infant deaths in a time of changing death certification and investigation practices: evaluating sleep-related risk factors for infant death in New York City. Matern Child Health J. 2011. 15:242–248.
19. Takatsu A, Shigeta A, Sakai K, Abe S. Risk factors, diagnosis and prevention of sudden unexpected infant death. Leg Med (Tokyo). 2007. 9:76–82.
20. Rouleau C, Bongrand AF, Pidoux O, Roustan E, Martrille L, Picaud JC, Costes-Martineau V, Cambonie G. Sudden infant death syndrome (SIDS): characteristics of deaths since the fall in SIDS in the French region of Languedoc-Roussillon. Arch Dis Child. 2009. 94:894–896.
21. Thogmartin JR, Siebert CF Jr, Pellan WA. Sleep position and bed-sharing in sudden infant deaths: an examination of autopsy findings. J Pediatr. 2001. 138:212–217.
22. Carroll-Pankhurst C, Mortimer EA Jr. Sudden infant death syndrome, bedsharing, parental weight, and age at death. Pediatrics. 2001. 107:530–536.
23. McGarvey C, McDonnell M, Hamilton K, O'Regan M, Matthews T. An 8 year study of risk factors for SIDS: bed-sharing versus non-bed-sharing. Arch Dis Child. 2006. 91:318–323.
24. Hutchison L, Stewart AW, Mitchell E. SIDS-protective infant care practices among Auckland, New Zealand mothers. N Z Med J. 2006. 119:U2365.
25. Blair PS, Fleming PJ, Smith IJ, Platt MW, Young J, Nadin P, Berry PJ, Golding J. Babies sleeping with parents: case-control study of factors influencing the risk of the sudden infant death syndrome: CESDI SUDI research group. BMJ. 1999. 319:1457–1461.
26. Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011. 128:103–110.
27. Seo JW, Kim YJ, Lee KH, Kim JY, Sim JG, Kim HS, Ko JS, Bae SH, Park HS, Park BS. A survey on the understanding of breast-feeding in pregnant woman. J Korean Pediatr Soc. 2002. 45:575–587.
28. Kemp JS, Unger B, Wilkins D, Psara RM, Ledbetter TL, Graham MA, Case M, Thach BT. Unsafe sleep practices and an analysis of bedsharing among infants dying suddenly and unexpectedly: results of a four-year, population-based, death-scene investigation study of sudden infant death syndrome and related deaths. Pediatrics. 2000. 106:E41.
29. Filiano JJ, Kinney HC. A perspective on neuropathologic findings in victims of the sudden infant death syndrome: the triple-risk model. Biol Neonate. 1994. 65:194–197.
30. Van Norstrand DW, Ackerman MJ. Sudden infant death syndrome: do ion channels play a role? Heart Rhythm. 2009. 6:272–278.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download