Abstract
Disturbances in biological rhythms could lead to unfavorable health impact. This study aimed to evaluate the prevalence of functional dyspepsia (FD) and irritable bowel syndrome (IBS) in rotating shift workers, and to determine the factors that have significant association with the prevalence of FD and IBS. The research had been carried out among nurses and nursing assistants working at Ewha Womans University Mokdong Hospital between December 2010 and February 2011. The subjects completed self-reported questionnaires, including the quality of the sleep and the level of stress. The prevalence of FD and IBS defined by ROME III criteria, and factors associated the disorders in rotating shift workers were compared with those of day workers. A total of 207 subjects were included in the study with 147 rotating shift workers (71.0%), and 60 (29.0%) day workers. The prevalence of IBS in rotating shift workers was higher than that in day workers (32.7% vs 16.7%, P = 0.026). However, no significant difference in the prevalence of FD was observed between the two groups (19.7% vs 20.0%, P = 0.964). In the multivariate analysis, the risk factors for IBS were rotating shift work (OR, 2.36; 95% CI, 1.01-5.47) and poor sleep quality (OR, 4.13; 95% CI, 1.82-9.40), and the risk factors for FD were poor sleep quality (OR, 2.31; 95% CI, 1.01-5.28), and severe stress (OR, 2.19; 95% CI, 1.06-4.76). A higher prevalence of IBS among rotating shift workers could be directly associated with the circadian rhythm disturbance. The circadian rhythm disturbance may be related with the pathogenesis of IBS.
Functional dyspepsia (FD) and irritable bowel syndrome (IBS) are common functional gastrointestinal (GI) disorders that are frequently encountered in the general population (1). Although accurate etiologies of functional GI disorders (FGIDs) are unknown, changes in bowel motility, visceral hypersensitivity, disruptions of intestinal barrier and psychological status were involved in its pathogenesis (2-4). A biopsychological model of disorder has been used to explain the connections between GI and emotional and cognitive functions. In this model, stressful life events and psychological distress were found to exacerbate IBS and FD as well as influence their clinical outcomes (5, 6).
In other words, stressful condition can make people to be susceptible to FGIDs, and can increase the occurrence, and change their natural courses. The pathogenesis of FGIDs related with psychological stress is unknown; however, brain-gut interactions are increasingly recognized as the underlying pathogenesis of FGIDs. Various central nervous system (CNS)- and gut-directed stressors stimulate the brain-gut axis. Disturbances at every level of neural control of the GI tract can affect modulation of gastrointestinal motility, secretion, and immune functions as well as perception and emotional response to visceral events (7). To date, significant associations between IBS and psychological distress including depression and anxiety have been reported (8). A recent study also supports this concept by showing the patients with IBS are relieved by psychiatric medications and cognitive behavior therapy (9). Similar associations with psychological stress have been reported for dyspepsia in clinical studies (10, 11).
The effects of poor sleep quality on psychological stress is also commonly reported among rotating shift workers. Several reports have been made that rotating shift workers experience relatively more stress compared to day workers, and have increased level of fatigue and poor sleep quality, resulting in more frequent daytime sleepiness and experience of physiologic change. A recent study in UK hypothesized sleep disturbance increase the risk of chronic disease including cancers, cardiovascular disease, metabolic syndrome, and diabetes, and declared suggestive evidence on the adverse association between night work and breast cancer (12). In addition, another study in the US showed association between night shift work and ischemic stroke and coronary heart disease (13).
Due to the increasing interests in aspect of biopsychological role in FD and IBS, the understanding of the illness pattern in rotating shift workers can be the means to approach to the pathophysiology. However, until now, only several studies with limited data have been published. Therefore, we aimed to estimate the prevalence of FD and IBS in rotating shift workers and the predictive factors significantly affecting the prevalence of the disorder.
The study population consisted of 277 subjects including nurses and nursing assistants working at Ewha Womans University Mokdong hospital between December 2010 and February 2011. The subjects were 18-yr old and older adult participants. Of the 277 participants, 60 were ruled out based on the exclusion criteria, and 207 were divided into daytime and rotating shift worker groups. The following exclusion criteria were applied: 1) the subjects with incomplete assessment questionnaire (n = 53); 2) pregnant or breast-feeding (n = 7); 3) self-reported organic GI disorder (n = 8); 4) having red flag signs (n = 2) such as fever, rectal bleeding and significant weight loss; 5) diagnosed with psychological disorder or current psychiatric medication users. The subjects completed structured self-reported questionnaires.
Eligible subjects who agreed to participate were asked to complete a series of validated questionnaires to assess:
A short-form of Korean version of bowel disease questionnaires (K-BDQ) was utilized to evaluate the prevalence of FD and IBS following ROME III diagnostic criteria. The K-BDQ was validated with direct interview with the median kappa of 0.74 (0.36-1.00) and verified after repeated test for reliability (14). The K-BDQ was composed of 30 items distinguishing several FGIDs such as IBS, FD, functional bloating, functional constipation, and functional diarrhea.
The Pittsburgh Sleep Quality Index (PSQI) was utilized to measure the sleep quality. Korean version of PSQI, a valid and reliable self administrative instrument for assessing quality of sleep (15). PSQI is designed to assess sleep quality for one month prior to examination and contains 19 self-rated questions from which 7 component scores are calculated and summed into a global score (16). Higher score represents worse sleep quality with component scores ranging from 0 to 3, and global scores range from 0 to 21. The Epworth Sleepiness Scale (ESS) is an 8-itemed questionnaire designed to assess general level of daytime sleepiness, and scores on this instrument range from 0 to 24, with higher scores indicating greater sleepiness (17). PSQI score higher than 5 points was set as the marker of poor sleep quality and ESS score higher than 13 points as the marker of daytime sleepiness (16, 18, 19).
The Modified Brief Encounter Psychosocial Instrument (BEPSI) (20, 21) was utilized to measure the stress level. Korean version of BEPSI (BEPSI-K) was a valid and reliable self administrative instrument for assessing stress (22, 23). The BEPSI-K consists of the following five items: 1) extrinsic demand or individual's perception of the balance between external demand and capability; 2) intrinsic demand, or the importance of the individual's expectations as demands one place on oneself; 3) attributional demand or expectations and demands that the individual places on his/her physical or interpersonal environment; 4) uncertainty demand or that uncontrollable events elicit a greater stress response than demands over which the individual has control; 5) demand perspective or the ability to maintain perspective in the face of stressful demand with maximum scores of each question being five points; the sum of each points was divided by five. A subject with a higher score experienced more stress. The internal consistency of the BEPSI-K was high (Cronbach's α: 0.84), and a factor analysis confirmed that the items represent a single dimension (24).
Statistical analysis was performed using SPSS version 18.0 (SPSS Inc, Chicago, IL, USA). The continuous variables were expressed as mean ± SD. Univariate associations were analyzed using the Student's t-test and Fisher extract test for categorical variables. All variables significantly associated with FD and IBS (P < 0.05, two tailed) were included in the multivariate logistic regression models. In addition, to reduce the effect of potential confounding in this observational study, we performed rigorous adjustment for the differences in baseline characteristics using propensity score matching. The propensity scores were estimated without regard to outcome variables, using multiple logistic regression analysis. Results were presented by odds ratio (OR) also with 95% confidence interval (CI).
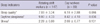
A total of 207 subjects were included in the present study with 147 rotating shift workers (71.0%), and 64 (29.0%) day workers (Table 1). Their mean age was 32.3 yr (± 7.8 SD), ranging from 21 to 53 yr old. The mean age in daytime workers was higher with female predominance. The proportion of married persons in day workers was higher than in the rotating shift workers (35.4% vs 58.3%, P = 0.002). The proportion of workers who had work experience more than 4 yr in day worker was higher in that of rotating shift worker (54.4% vs 78.3%, P = 0.006). Body mass index (BMI) was 21.1 kg/m2 (± 2.52 SD), and no significant difference was observed between two groups. The average length of working time was 9.2 hr (± 1.3 SD) per day, ranging from 5 to 15 and the average length of sleeping time was 6.3 hr (± 1.5 SD) with no significant differences between the two groups. In addition, no significant differences were found depending on regular exercise, drinking habit, and coffee consumption between the two groups, and the proportion of sleeping pill users was only 5 persons (2.3%).
The prevalences of FD and IBS were 19.8% and 28.0%, respectively. The prevalence of FD in rotating shift worker and in day worker were 19.7% (95% CI, 14.3-25.1) and 20.0% (95% CI, 14.6-25.4). The prevalence of IBS in rotating shift worker and in day worker were 32.7% (95% CI, 26.3-39.1) and 16.7% (95% CI, 11.6-21.8), respectively.
The prevalence of IBS in rotating shift worker group was significantly higher than that of daytime worker group (32.7% vs 16.7%, P = 0.026). No significant difference on the prevalence of FD between rotating shift worker group and daytime worker group (19.7% vs 20.0%, P = 0.964) was found (Fig. 1).
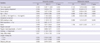
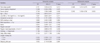
The sleep quality and stress of rotating shift worker group was compared with those of day worker group. Results showed higher daytime sleepiness (ESS 9.80 ± 4.33 vs 8.42 ± 4.10, P = 0.036) in rotating shift worker group. However, no difference in sleep quality (PSQI 7.03 ± 3.34 vs 6.18 ± 2.88, P = 0.086) and stress scale index was observed between the two groups (BEPSI 2.28 ± 0.80 vs 2.09 ± 0.77, P = 0.131) (Table 2).
The presence of FD had an influence on sleep-related indicator, with higher effect on rotating shift workers than day workers. Rotating shift worker with FD showed poorer sleep quality (PSQI 8.10 ± 3.51 vs 6.77 ± 3.26, P = 0.054), and more stressful state (BEPSI 2.60 ± 0.74 vs 2.20 ± 0.80, P = 0.015) than those without FD. In day worker group, the sleep quality in subjects with FD was poorer than in those without FD (PSQI 7.67 ± 2.54 vs 5.81 ± 2.86, P = 0.045). On the other hand, no differences in daytime sleepiness (ESS 9.25 ± 3.55 vs 8.21 ± 4.24, P = 0.436) and stress level (BEPSI 2.40 ± 0.69 vs 2.02 ± 0.77, P = 0.122) were found.
Similar findings are shown for the IBS. In rotating shift worker group, subjects with IBS showed poorer sleep quality (PSQI 8.29 ± 2.92 vs 6.42 ± 3.37, P = 0.001), more frequent daytime sleepiness (ESS 10.90 ± 4.45 vs 9.26 ± 4.19, P = 0.031), and more severe stress (BEPSI 2.50 ± 0.83 vs 2.17 ± 0.77, P = 0.017) compared with those without IBS. However, in daytime worker group, the day time sleepiness in subjects with IBS was severe than in those without IBS (ESS 10.80 ± 4.21 vs 7.94 ± 3.95, P = 0.043). On the other hand, no differences in sleep quality (PSQI 7.30 ± 2.63 vs 5.96 ± 2.90, P = 0.181) and stress level (BEPSI 2.26 ± 1.12 vs 2.06 ± 0.69, P = 0.456) were found. This comparison was summarized in Fig. 2, 3.
Tables 3, 4 show the risk factors for the presence of FD and IBS, respectively. The ORs for each factor, which are known to be involved in the occurrence of the disease, basic demographic factors (e.g. age, gender, marital status, BMI), and factors that reflect the life style (e.g. frequency of weekly exercise and coffee drink, and smoking) were analyzed. In univariate analysis, the factors associated with FD were poor sleep quality (PSQI ≥ 6 vs < 6, OR, 2.79; 95% CI, 1.25-6.21), and severe stress (BEPSI ≥ 2.8 vs < 2.8, OR, 2.75; 95% CI, 1.33-5.69). In multivariate analysis, they were also the predictors for FD.
On the other hand, the factors associated with IBS in univariate analysis were rotating shifting work (rotating vs day, OR, 2.42; 95% CI, 1.13-5.19), poor sleep quality (PSQI ≥ 6 vs < 6, OR, 5.23; 95% CI, 2.40-11.41), severe daytime sleepiness (ESS ≥ 14 vs < 14, OR, 2.25; 95% CI, 1.06-4.78), severe stress (BEPSI ≥ 2.8 vs < 2.8, OR, 2.84; 95% CI, 1.46-5.54), low BMI (< 18.5 kg/m2 vs ≥ 18.5 kg/m2, OR, 2.65; 95% CI, 1.20-5.85), younger age (≤ 29 yr vs ≥ 30 yr, OR, 1.81; 95% CI, 0.98-3.36), and working as a nurse (nurse vs nursing assistant, OR, 1.92; 95% CI, 1.02-3.62). In multivariate analysis, predictors for IBS were participation in rotating shifting work (rotating vs day, OR, 2.36; 95% CI, 1.01-5.47) and poor sleep quality (OR, 4.13; 95% CI, 1.82-9.40). In propensity score adjusted analysis, OR for shifting work was 3.55 (95% CI, 1.35-9.32).
The present study shows that the prevalences of FD 19.8% and IBS were 28.1% in nurses and nursing assistants. Rotating shift workers have a higher risk of IBS, and their significant factor of IBS is poor sleep quality.
Because there are no biological markers for IBS, the diagnosis is usually based on symptoms and exclusion of other known organic disorder (24). The varying nature of symptoms and lack of structural abnormalities present a diagnostic challenge. The altered motility, visceral hypersensitivity, dysfunctional brain-gut interaction, low-grade mucosal inflammation, genetic factors, food allergies, and altered bowel microflora can give rise to the characteristic clinical symptoms of IBS (25). Some studies incited the psychosocial aspects of IBS and FD, revealed altered GI symptoms of rotating shift workers, as a part of a various symptoms (26). Furthermore, several studies have reported a higher prevalence of GI symptoms such as diarrhea, bloating, and heartburn among the rotating shift workers compared to daytime worker (27, 28). However only few studies focused on the prevalence of FGIDs among rotating shift workers (29, 30). In the present study, the prevalence of FD and IBS in hospital workers was higher than general population. In a population-based study in Korea, the prevalence of FD was 8.4% and that of IBS was 6.6% based on ROME II criteria in a local community (31). The results of our study are consistent with those studies from Singapore, which found the prevalence of FGIDs to be 38% in nurses working rotating shift vs 20% in daytime worker nurses (P = 0.04). Studies from the US (399 participants, 214 permanent daytime workers vs 75 rotating shift workers), gave the same results (31.3% vs 48.0%, P < 0.01). Previous studies that attempted to assess the association between sleep disturbances and IBS yielded conflicting results (31-33). However, results of our study suggest that poor sleep quality in rotating shift workers provide an explanation for the higher prevalences of FD and IBS in rotating shift workers. In a logistic regression analysis, an association between IBS and rotating shift worker was recognized even after controlling other confounding factors, such as poor sleep quality and marital status.
Recent studies showed that rotating shift workers suffer more from disruption of circadian rhythm. Therefore, they experience subjective symptoms such as increased fatigue, insomnia, hypersomnia, sleep disturbances, lack of appetite as well as actual medical problems such as GI system, cardiovascular system, and working a rotating shift threatening to general health (33, 34).
Therefore, it is conceivable that disruption of circadian rhythm will lead to alterations in circadian physiology that modulates visceral sensitivity. Furthermore, a recent clinical study showed that administration of melatonin, a known regulator of circadian rhythm, can improve IBS symptoms by decreasing pain without altering colonic motility. The fact that pain was relieved after the administration of melatonin could be results of the restoration of circadian rhythms (34).
Previous studies carried out targeting nurses in Korea as rotating shift workers revealed that rotating shift work, in spite of relatively longer sleep time, brings about poor sleep quality and harmful effects on health (33, 35). Although a cross sectional study from the US focused on the disruption of biological rhythm of shift workers, the prevalence of the IBS is affected not only by disruption of circadian rhythm but also by quality of sleep (36).
The psychological factors are major part of IBS pathogenesis. Approximately two thirds of IBS patients referred to secondary care centers show some form of psychological distress, most commonly anxiety or depression, which may not be easily recognized, as some patients are reluctant to expose their feelings. Nevertheless, multiple unexplained physical symptoms are common in IBS and can be a manifestation of somatization disorder (37). The association of IBS and psychological factors are observed via the meta-analysis that proves the efficacy of tricyclic antidepressants in IBS (38). Moreover, poor sleep quality affects adverse psychological factors in rotating shift workers. Previous reports on psychological status as an etiology of IBS and sleep disturbances in rotating shift workers are compatible with the conclusion of the present study (29).
However, the present study has some limitations, including selection biases. The study population consisted of nurses and nursing assistants of one university hospital. And nurses are thought to be exposed to relatively high level of occupational stress due to the nature of their work. These may influence the possibility of generalizing our results to the general rotating shift workers. Furthermore, it is conceivable that individuals with higher degree of anxiety of psychological distress or those with other health problems including GI disease require more time off work, and therefore more likely to participate in rotating shiftwork. However, there was no significant difference in stress scores between the two groups, because the subjects with significant health problems were excluded in the screening.
Second, the psychological status of each individual is not assessed by an objective method. Therefore, psychological influences of the subjects are not completely ruled out upon analysis of the attributing factors of IBS. Thus, intake of psychiatric medication was checked by questionnaires instead; all subjects were found to be free from psychiatric medication. Therefore, to expand the study, adaptation of psychometric instrument is required to exclude the psychological influences on IBS.
Third, this study covers two hypotheses of different disease simultaneously and does not correct the problem of multiple comparisons. The result is observed as part of an analysis that involves multiple comparisons, rather than an analysis that involves only a single comparison.
In conclusion, participation in rotating shift work and poor sleep quality were significantly associated with IBS, and rotating shift work itself was related with IBS, independent with poor sleep quality. Therefore disruption of circadian rhythm is suggested to have an important role in the pathogenesis of IBS.
Figures and Tables
 | Fig. 1Comparison of prevalence of functional gastrointestinal disorders. The prevalence of Functional Dyspepsia (FD) and Irritable Bowel Syndrome (IBS) is higher in rotating shift worker group, compared with day worker group. |
 | Fig. 2Association between sleep related indicator and functional dyspepsia (FD). Workers with FD shows significantly poorer sleep quality than those without FD. The stress score is significantly higher in rotating shift workers with FD than those without FD. |
 | Fig. 3Association between sleep related indicator and irritable bowel syndrome (IBS). Rotating shift workers with IBS shows poorer sleep quality, more daytime sleepiness and more stress than those without IBS. |
References
1. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006. 130:1480–1491.
2. Lawal A, Kern M, Sidhu H, Hofmann C, Shaker R. Novel evidence for hypersensitivity of visceral sensory neural circuitry in irritable bowel syndrome patients. Gastroenterology. 2006. 130:26–33.
3. Piche T, Barbara G, Aubert P, Bruley des Varannes S, Dainese R, Nano JL, Cremon C, Stanghellini V, De Giorgio R, Galmiche JP, et al. Impaired intestinal barrier integrity in the colon of patients with irritable bowel syndrome: involvement of soluble mediators. Gut. 2009. 58:196–201.
4. Saito YA, Talley NJ. Genetics of irritable bowel syndrome. Am J Gastroenterol. 2008. 103:2100–2104.
5. Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002. 123:2108–2131.
6. Bennett EJ, Tennant CC, Piesse C, Badcock CA, Kellow JE. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut. 1998. 43:256–261.
7. Mulak A, Bonaz B. Irritable bowel syndrome: a model of the brain-gut interactions. Med Sci Monit. 2004. 10:RA55–RA62.
8. Solmaz M, Kavuk I, Sayar K. Psychological factors in the irritable bowel syndrome. Eur J Med Res. 2003. 8:549–556.
9. Hayee B, Forgacs I. Psychological approach to managing irritable bowel syndrome. BMJ. 2007. 334:1105–1109.
10. Haug TT, Svebak S, Wilhelmsen I, Berstad A, Ursin H. Psychological factors and somatic symptoms in functional dyspepsia: a comparison with duodenal ulcer and healthy controls. J Psychosom Res. 1994. 38:281–291.
11. Jones MP, Maganti K. Symptoms, gastric function, and psychosocial factors in functional dyspepsia. J Clin Gastroenterol. 2004. 38:866–872.
12. Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC. Shift work and chronic disease: the epidemiological evidence. Occup Med (Lond). 2011. 61:78–89.
13. Brown DL, Feskanich D, Sánchez BN, Rexrode KM, Schernhammer ES, Lisabeth LD. Rotating night shift work and the risk of ischemic stroke. Am J Epidemiol. 2009. 169:1370–1377.
14. Song HJ, Jung HK, Yeom HJ. Reliability and validity of Korean bowel disease questionnaire and prevalence of functional gastrointestinal disorders in Korea. Gut. 2009. 58:A112.
15. Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012. 16:803–812.
16. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989. 28:193–213.
17. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991. 14:540–545.
18. Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, Reis SE, Matthews KA. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008. 4:563–571.
19. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991. 14:540–545.
20. Baldi F, Ferrarini F, Longanesi A, Ragazzini M, Barbara L. Acid gastroesophageal reflux and symptom occurrence: analysis of some factors influencing their association. Dig Dis Sci. 1989. 34:1890–1893.
21. Gisbert JP, Cooper A, Karagiannis D, Hatlebakk J, Agréus L, Jablonowski H, Nuevo J. Impact of gastroesophageal reflux disease on work absenteeism, presenteeism and productivity in daily life: a European observational study. Health Qual Life Outcomes. 2009. 7:90.
22. Cathébras PJ, Robbins JM, Kirmayer LJ, Hayton BC. Fatigue in primary care: prevalence, psychiatric comorbidity, illness behavior, and outcome. J Gen Intern Med. 1992. 7:276–286.
23. Yim JH, Bae JM, Choi SS, Kim SW, Hwang HS, Heo BR. The validity of modified korean-translated BEPSI (Brief Encounter Psychosocial Instrument) as instrument of stress measurement in outpatient clinic. J Korean Acad Fam Med. 1996. 17:42–49.
24. Agrawal A, Whorwell PJ. Irritable bowel syndrome: diagnosis and management. BMJ. 2006. 332:280–283.
25. Barbara G, De Giorgio R, Stanghellini V, Cremon C, Corinaldesi R. A role for inflammation in irritable bowel syndrome? Gut. 2002. 51:i41–i44.
26. McFarland LV. State-of-the-art of irritable bowel syndrome and inflammatory bowel disease research in 2008. World J Gastroenterol. 2008. 14:2625–2629.
27. Caruso CC, Lusk SL, Gillespie BW. Relationship of work schedules to gastrointestinal diagnoses, symptoms, and medication use in auto factory workers. Am J Ind Med. 2004. 46:586–598.
28. Knutsson A. Health disorders of shift workers. Occup Med (Lond). 2003. 53:103–108.
29. Zhen Lu W, Ann Gwee K, Yu Ho K. Functional bowel disorders in rotating shift nurses may be related to sleep disturbances. Eur J Gastroenterol Hepatol. 2006. 18:623–627.
30. Cremonini F, Camilleri M, Zinsmeister AR, Herrick LM, Beebe T, Talley NJ. Sleep disturbances are linked to both upper and lower gastrointestinal symptoms in the general population. Neurogastroenterol Motil. 2009. 21:128–135.
31. Han SH, Lee OY, Bae SC, Lee SH, Chang YK, Yang SY, Yoon BC, Choi HS, Hahm JS, Lee MH, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. Korean J Neurogastroenterol Motil. 2006. 12:183.
32. Fass R, Fullerton S, Tung S, Mayer EA. Sleep disturbances in clinic patients with functional bowel disorders. Am J Gastroenterol. 2000. 95:1195–1200.
33. Kim YG, Yoon DY, Kim JI, Chae CH, Hong YS, Yang CG, Kim JM, Jung KY, Kim JY. Effects of health on shift-work: general and psychological health, sleep, stress, quality of life. Korean J Occup Environ Med. 2002. 14:247–256.
34. Lu WZ, Gwee KA, Moochhalla S, Ho KY. Melatonin improves bowel symptoms in female patients with irritable bowel syndrome: a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2005. 22:927–934.
35. Ko HJ, Kim MA, Kwon YS. The fatigue experience of shiftwork nurse. J Korea Community Health Nurs Acad Soc. 2004. 18:103–118.
36. Nojkov B, Rubenstein JH, Chey WD, Hoogerwerf WA. The impact of rotating shift work on the prevalence of irritable bowel syndrome in nurses. Am J Gastroenterol. 2010. 105:842–847.
37. Spiller R, Aziz Q, Creed F, Emmanuel A, Houghton L, Hungin P, Jones R, Kumar D, Rubin G, Trudgill N, et al. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007. 56:1770–1798.
38. Rahimi R, Nikfar S, Rezaie A, Abdollahi M. Efficacy of tricyclic antidepressants in irritable bowel syndrome: a meta-analysis. World J Gastroenterol. 2009. 15:1548–1553.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download