Abstract
We aimed to compare the immune response induced by natural infection with 2009 pandemic influenza A/H1N1 (pH1N1) virus and by monovalent pH1N1 vaccination in children and adolescents. This cross-sectional clinical study was conducted at 3 hospitals in Korea from February to May 2010. A total of 266 healthy subjects aged from 6 months to 18 yr were tested for the presence of the antibody against pH1N1 using hemagglutination inhibition (HI) test. Information about pH1N1 vaccination and laboratory-confirmed pH1N1 infection history was obtained. The overall rate of HI titers of ≥ 1:40 against pH1N1 was 38.7%, and the geometric mean titer (GMT) was 20.5. Immunogenicity of pH1N1 vaccination only was reflected by a 41.1% of seroprotection rate and a GMT of 22.5. Immunogenicity of natural infection only was reflected by a 61.0% of seroprotection rate and a GMT of 40.0. GMT was significantly higher in the subjects of natural infection group than in the subjects of pH1N1 vaccination group (P < 0.001). The immune responses induced by natural pH1N1 infection exceed those induced by pH1N1 vaccinations.
Novel swine-origin influenza A/H1N1 virus infection originated in Mexico in April 2009 and was determined to be the cause of febrile respiratory illness (1, 2). The World Health Organization declared a pandemic in June 2009. Novel swine-origin influenza A/H1N1 virus rapidly spread to many countries, causing a worldwide pandemic. The active use of oseltamivir and large-scale vaccination with the pandemic influenza vaccine during the pandemic period controlled the spread of infection. The 2009 pandemic influenza A/H1N1 (pH1N1) virus infection was also present in Korea. At that time, oseltamivir was provided to treat the suspicious influenza-like illness at nearly all hospitals and clinics nationwide. Under government direction, the monovalent 2009 pH1N1 vaccine (Green Cross Corporation, Yongin, Korea) was developed and national vaccination was started in late October 2009. With these efforts, pH1N1 was resolved in the early part of 2010.
The most probable reason for the end of pandemic was the acquisition of immunity against the pH1N1 virus by most people. Vaccination-acquired immunity might account for a great part of this immunity, but the proportion of immunity acquired by natural infection may be also considerable. It is important to characterize the immunogenicity induced by natural infections to evaluate herd immunity, especially against pH1N1 infection. Immune responses that are induced by wild-type infection are generally superior to those induced by inactivated vaccination. Live-attenuated vaccines can induce mucosal immune and cellular immune responses in a manner similar to those in infection (3). The immunogenicity induced by natural infection may also be dependent on several factors including personal immune status, age, and concurrent use of medications (4).
Seroprevalence studies in children are rare (5) but significant owing to their important role in the transmission of influenza (6, 7). Few studies have compared the antibody titers against pH1N1 after natural infection and vaccination (8). The aim of this cross-sectional study was to compare the immune response induced by natural infection with pH1N1 to that induced by monovalent pH1N1 vaccination in children.
Enrollment was conducted at 3 hospitals from February to May 2010 (Department of Pediatrics, Korea Cancer Center Hospital, 2 pediatric practices located in Seoul and Gyeonggi-do). Healthy children aged 6 months to 18 yr who were free of illnesses impeding immune response were enrolled in the study.
After written informed consent was obtained, 3-4 mL of venous blood was obtained from all subjects. Serum was centrifuged and stored at -70℃ until analysis. A questionnaire pertaining to the child's age and sex, history of pandemic or seasonal influenza vaccination, and history of laboratory-confirmed influenza infection was completed by the parents. According to the questionnaire responses, the subjects were classified into the following 4 groups: subjects who had monovalent pH1N1 vaccination and no history of pH1N1 infection, subjects who had no monovalent pH1N1 vaccination and a history of pH1N1 infection, subjects reporting neither monovalent pH1N1 vaccination nor pH1N1 infection, and subjects who were infected with pH1N1 after monovalent pH1N1 vaccination. The primary outcome of the present study was comparison of the immunogenicity among the 4 groups. We also compared the immune response against pH1N1 in 3 different age groups (< 3 yr, 3-8 yr, 9-18 yr) to evaluate the differential effect of immunogenicity with respect to age. Virological confirmation of pH1N1 infection at that time period was performed using pH1N1-specific real-time reverse transcriptase-polymerase chain reaction (RT-PCR) in most hospitals. An influenza A-positive result from the rapid antigen test was also included because > 95% of influenza isolates were pH1N1 viruses (9). The monovalent pH1N1 vaccine administered to the participants was inactivated and unadjuvanted vaccine (Greenflu-S®, Green Cross Corporation, Yongin, Korea) containing 7.5 µg (subjects < 3 yr of age) or 15 µg (subjects ≥ 3 yr of age) of the recommended pH1N1 antigen A/California/7/2009 (H1N1). Two doses of the vaccine were administered to the subjects aged < 9 yr-old and one dose was administered to the aged ≥ 9 yr old.
Antihemagglutinin antibody titers were determined using the HI test according to the "WHO Manual on Animal Influenza Diagnosis and Surveillance" (10), which is the most commonly used reference. All assays were performed in duplicate and the mean value of each was taken. The pH1N1 vaccine seed virus was used for the HI tests. An HI titer of < 10 was assigned a value of 5 for computation of the geometric mean titer (GMT).
Immunogenicity was assessed according to the seroprotection rate and GMT of HI. Seroprotection rate was defined as the proportion of subjects with HI titers of ≥ 1:40 (11).
Descriptive data are reported as numbers of subjects and as percentages or GMT, with 95% confidence intervals (95% CI). Comparisons of immunogenicity (seroprotection rate) among groups were performed using the chi-squared test. P values of < 0.05 were considered significant (2-tailed test). SPSS software version 12.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analyses.
A total of 266 healthy children and adolescents with nearly equal gender distribution were enrolled in the present study (Table 1). The mean participant age was 5.8 yr (0.5-18.7 yr). For pH1N1, the overall seroprotection rate (HI ≥ 1:40) was 38.7% and the GMT was 20.5 (95% CI, 18.5-22.4). Of the children aged < 3 yr, the seroprotection rate and GMT was 28.1% and 16.5 (95% CI, 13.2-19.7), respectively. Of the children aged 3-8 yr, the seroprotection rate and GMT was 50.0% and 18.2 (95% CI, 15.3-21.1), respectively. Of the children aged 9-18 yr, the seroprotection rate and GMT was 51.1% and 33.4 (95% CI, 28.3-38.6), respectively.
Of the 266 subjects, 196 were vaccinated with the pH1N1 vaccine. The mean age of 196 vaccinated subjects was 6.2 yr and 100 subjects were male. The mean duration from pandemic influenza vaccination to the HI test was 58 days (21-148 days). The overall seroprotection rate and GMT among the subjects who received the pH1N1 vaccination was 40.8% and 22.4, respectively (Fig. 1). Of the 196 children who received the pH1N1 vaccine, 57 were aged < 3 yr, 87 were aged 3-8 yr, and 52 were aged 9-18 yr. The immunogenicity induced by each vaccine was stratified by age. Of the children aged < 3 yr, the seroprotection rate and GMT was 28.1% and 17.9 (95% CI, 14.5-21.4), respectively (Fig. 2). Of the children aged 3-8 yr, the seroprotection rate and GMT was 43.7% and 21.3 (95% CI, 16.7-25.9), respectively. Of the children aged 9-18 yr, the seroprotection rate and GMT was 51.9% and 31.1 (95% CI, 22.9-39.2), respectively.
Of the 266 subjects, 27 (15 male, 12 female) had confirmed pH1N1 virus infection. The mean duration of the pH1N1 diagnosis to the sampling was 94.7 days (52-177 days). The mean age of the infected subjects was 5.5 yr; 21 (77.8%) were aged 3-8 yr. The rate of infection by age was 4.9% in the group of aged < 3 yr (4/82), 16.7% (21/126) in the group of aged 3-8 yr, and 3.4% (2/58) in the group of aged 9-18 yr. The seroprotection rate and GMT by pH1N1 virus infection was 59.3% and 36.1 (95% CI, 24.8-37.0), respectively.
Of the 196 children who received the monovalent pH1N1 vaccine, 192 had no history of clinical infection with the pH1N1 virus and 4 had a history of laboratory-confirmed pH1N1 virus infection. Of the 70 children who did not receive the monovalent pH1N1 vaccine, 23 had laboratory-confirmed pH1N1 virus infection, and 47 had no history of clinical infection with pH1N1 virus (Table 2). In the subjects who received the monovalent pH1N1 vaccination but did not have a history of pH1N1 virus infection, the seroprotection rate was 41.1% and the GMT was 22.5 (group A). The immunogenicity induced by vaccine increased with age.
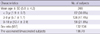
On the other hand, the immunogenicity induced by pH1N1 natural infection without monovalent pH1N1 vaccination was reflected by a 61.0% seroprotection rate and a GMT of 40.0 (group B). GMT of group B was significantly higher than that of group A (P < 0.001). When we compared GMT between the vaccination and infection groups including the 18 subjects who had HI titers > 10 (presumed as asymptomatic infection) from group C, GMT was still significantly different (22.5 vs 36.1, 95% CI, 28.2-44.1, P < 0.001). The mean duration from the day of vaccination/infection to sampling day was significantly different (58 vs 95 days, P < 0.05). To reduce the influence by this different duration of the vaccination/infection to sampling between group A and B, we limited the duration from 50 to 150 days. The age of subjects was also limited as between 6 months and 10 yr old. After matching the age within the limited duration, the difference of GMT between group A and B was more prominent (Table 3). A total of 31.4% of the subjects who had neither pH1N1 vaccination nor pH1N1 virus infection (group C) had HI titers of ≥ 1:40.
Among the 196 monovalent pH1N1-vaccinated subjects, 191 subjects answered questions about their history of previous seasonal influenza vaccination (2009-2010 season). A total of 131 of 191 (68.6%) children were vaccinated with seasonal influenza vaccine. Of the children vaccinated with monovalent pH1N1 vaccine after seasonal influenza vaccination, the seroprotection rate was 37.1% and the GMT was 20.7 (95% CI, 17.7-23.8). Of the subjects vaccinated with monovalent pH1N1 vaccine alone, 49.2% achieved HI titers ≥ 1:40 and the GMT was 30.2 (95% CI, 21.8-38.6). There was a significant difference between the 2 groups (P < 0.05, Fig. 3).
The overall seroprotection rate provided by the monovalent pH1N1 vaccine was 40.8%. This rate is lower than those reported by most studies on immunogenicity among children (12, 13). In a clinical trial on immunogenicity against the same pH1N1 vaccine with our study, which has been carried out in Korea in 2009, seroprotection rate in subjects 6 months to < 9 yr of age were lower than the previous results. HI titers ≥ 1:40 were observed in 55.9% of subjects < 3 yr, 69.5% of subjects 3-8 yr, and 90.5% of subjects 9-18 yr of age by day 21 after the second dose (14). Relatively low seroprotection rate against the vaccine might be applied similarly to our study subjects. This may be the main reason for the weak immune response in our study. The second reason for the weak response is delayed post-vaccination sampling (mean 58 days after vaccination) to evaluate the immunogenicity. Antihemagglutinin antibody titers of inactivated influenza vaccination peak at 3-4 weeks after vaccination. Therefore, most of the studies that evaluate vaccine immunogenicity show the antibody titers at that time point. Low antibody titers of children aged < 3 yr, which comprised 29% of our study subjects, also contribute to the weak immunogenicity. The seroprotection rate of this age group was 28.1% compared with 50% in the older age groups. The immune response in infants and young children by vaccination is lower than that in older children and adults (8, 13-15). Even at an age of < 2 yr, the antibody responses increase with age (16).
There have been a few studies focusing on pH1N1-induced immunogenicity. One seroprevalence study of pandemic influenza among children demonstrated that subjects vaccinated against the pH1N1 virus exhibited lower titers than subjects with laboratory-confirmed pH1N1 virus infection (8). We also demonstrated that natural infection-induced immunogenicity was higher than that induced by inactivated vaccine. However, only 61% of the subjects with natural influenza infection had protective antibody titers against pH1N1. This result is short of the expected natural infection-induced immunogenicity. Except for the obviously delayed sampling, after confirmation of the infection (mean 95 days), one possible reason for the weak immune response is the aggressive use of oseltamivir by the infected subjects during the pandemic period. Medication with oseltamivir was the most different point in coping with the influenza pandemic wave compared with previous seasonal influenza seasons. All infected subjects were treated with oseltamivir for 5 days in the present study. This might have influenced the natural H1N1 infection-induced immunogenicity in this study.
Since influenza viruses invade the respiratory mucosal surface, mucosally produced secretory immunoglobulin A (IgA) antibodies are thought to be the most effective and immediate defense (17). One recent study about the effect of oseltamivir on the immune response showed that oseltamivir significantly suppressed respiratory mucosal secretory IgA responses and decreased the neutralizing activities of the airway fluids (18). Oseltamivir treatment reduces the viral load of patients with pH1N1 virus infection (19). Consequently, the decrease of viral load and suppression of mucosal immune system by oseltamivir treatment might negatively influence immune responses to the influenza virus.
It was notable in our study that 31% of the subjects who neither received pH1N1 vaccination nor had a history of pH1N1 virus infection had HI titers of ≥ 1:40 against pH1N1 virus. Older adults born before 1950 had HI titers of ≥ 1:80 at a rate of 34% against pH1N1 virus via previous natural infection with seasonal H1N1 viruses (20). On the other hand, children had little evidence of cross-reactive antibodies to pH1N1. Therefore, our result suggests subclinical or asymptomatic infection with pH1N1 virus. Studies have described a 25%-30% rate of subclinical or asymptomatic pH1N1 infection (8, 21). Subjects with milder symptoms or non-symptoms might not consider themselves infected with influenza and not visit the hospital for laboratory test confirmation. Further, the inclusion of only laboratory-confirmed cases as the infected subjects in this study might have underestimated the proportion of infected subjects. Underestimation of the rate of asymptomatic infection may contribute to the spread of infections and make it difficult to measure the exact incidence of influenza infection. Serological diagnosis of subclinical infections could be performed by the identification of 4-fold or greater increases in antibody titer after infection, compared with baseline titers.
We found that the rate of HI titers of ≥ 1:40 against pH1N1 in subjects vaccinated with both the seasonal and the pH1N1 vaccine (37.1%) was lower than in those who received the pH1N1 vaccine only (49.2%). Several studies have suggested a possible suppressive impact of the seasonal influenza vaccine on the immune response to pH1N1 (12, 22-24). An association between prior receipt of the 2008-2009 trivalent inactivated seasonal influenza vaccine and pH1N1 illness was suggested in 1 study performed in Canada (24). One of the hypotheses suggested by that study is that repeat immunization blocks the more complex and cross-protective immunity afforded by prior infection. Similarly, other studies found a diminution of antibody response in patients with higher baseline titers of pH1N1 and prior seasonal vaccine exposure (12, 22). We obtained similar results in this study in spite of not evaluating the baseline pH1N1 titers. Further, research is needed to confirm the findings about this effect.
The main limitation of this study was that we could not evaluate the baseline antibody titers before vaccination and could not rule out the asymptomatic infection in the vaccinated group. Another limitation was the small number of subjects in the infected group (n=23, group B).
In summary, this study demonstrated that the immune response to wild-type pH1N1 virus infection exceeds that to vaccination and that aggressive use of antiviral agents may influence natural infection-induced immunogenicity. Subclinical pH1N1 infections were assumed in approximately 30% of the children with neither pH1N1 vaccination nor a history of lab-confirmed pH1N1 virus infection. In addition, previous seasonal influenza vaccination seems to have a negative impact on the immune response to pH1N1 vaccination. Evaluation of the influence of natural infection and vaccination on herd immunity is important and necessary. Several factors including age, prior influenza exposure, and the type of prior vaccination should be considered to evaluate vaccine efficacy and develop an ideal vaccine.
Figures and Tables
Table 2
Immune response against pH1N1 among 4 groups
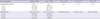
*GMT of group B was significantly higher than that of group A (P < 0.001). A, monovalent pH1N1 vaccination (+)/pH1N1 infection (-) group; B, monovalent pH1N1 vaccination (-)/pH1N1 infection (+) group; C, monovalent pH1N1 vaccination (-)/pH1N1 infection (-) group; D, monovalent pH1N1 vaccination (+)/pH1N1 infection (+) group.
ACKNOWLEDGMENTS
We acknowledge pediatricians Drs. Jang HO and Park KW (Star Pediatrics Clinic, Gyeonggi-do and Love for Neighbor Pediatrics Clinic, Seoul, Korea, respectively) for enrolling the healthy volunteers in this study. The authors have no conflicts of interest to disclose.
References
1. CDC. Swine influenza A (H1N1) infection in two children-Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009. 58:400–402.
2. CDC. Outbreak of swine origin influenza A (H1N1) virus infection-Mexico, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009. 58:467–470.
3. Kreijtz JH, Fouchier RA, Rimmelzwaan GF. Immune responses to influenza virus infection. Virus Res. 2011. 162:19–30.
4. Demicheli V, Jefferson T, Rivetti D, Deeks J. Prevention and early treatment of influenza in healthy adults. Vaccine. 2000. 18:957–1030.
5. Broberg E, Nicoll A, Amato-Gauci A. Seroprevalence to influenza A (H1N1) 2009 virus: where are we? Clin Vaccine Immunol. 2011. 18:1205–1212.
6. Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010. 375:1100–1108.
7. Kim JH, Yoo HS, Lee JS, Lee EG, Park HK, Sung YH, Kim S, Kim HS, Shin SY, Lee JK. The spread of pandemic H1N1 2009 by age and region and the comparison among monitoring tools. J Korean Med Sci. 2010. 25:1109–1112.
8. Von Kries R, Weiss S, Falkenhorst G, Wirth S, Kaiser P, Huppertz HI, Tenenbaum T, Schroten H, Streng A, Liese J, et al. Post-pandemic seroprevalence of pandemic influenza A (H1N1) 2009 infection (Swine flu) among children <18 years in Germany. PLoS One. 2011. 6:e23955.
9. Korea Centers for Disease Control and Prevention. Current status of selected infectious diseases. Public Health Wkly Rep. 2009. 2:886.
10. WHO. WHO manual on animal influenza diagnosis and surveillance. accessed on 27 Nov 2011. Available at: www.who.int/csr/resources/publications/influenza/whocdscsrncs20025rev.pdf.
11. Potter CW, Oxford JS. Determinants of immunity to influenza infection in man. Br Med Bull. 1979. 35:69–75.
12. Nolan T, McVernon J, Skeljo M, Richmond P, Wadia U, Lambert S, Nissen M, Marshall H, Booy R, Heron L, et al. Immunogenicity of a monovalent 2009 influenza A (H1N1) vaccine in infants and children: a randomized trial. JAMA. 2010. 303:37–46.
13. Plennevaux E, Sheldon E, Blatter M, Reeves-Hoché MK, Denis M. Immune response after a single vaccination against 2009 influenza A H1N1 in USA: a preliminary report of two randomised controlled phase 2 trials. Lancet. 2010. 375:41–48.
14. Oh CE, Lee J, Kang JH, Hong YJ, Kim YK, Cheong HJ, Ahn YJ, Kim SH, Lee HJ. Safety and immunogenicity of an inactivated split-virus influenza A/H1N1 vaccine in healthy children from 6 months to <18 years of age: a prospective, open-label, multi-center trial. Vaccine. 2010. 28:5857–5863.
15. Fiore AE, Neuzil KM. 2009 influenza A (H1N1) monovalent vaccines for children. JAMA. 2010. 303:73–74.
16. Walter EB, Rajagopal S, Zhu Y, Neuzil KM, Fairchok MP, Englund JA. Trivalent inactivated influenza vaccine (TIV) immunogenicity in children 6 through 23 months of age: do children of all ages respond equally? Vaccine. 2010. 28:4376–4383.
17. Wright P. Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Influenza viruses. Nelson textbook of pediatrics. 2007. 18th ed. Philadelphia, PA: Saunders;1384–1386.
18. Takahashi E, Kataoka K, Fujii K, Chida J, Mizuno D, Fukui M, Hiro-O Ito, Fujihashi K, Kido H. Attenuation of inducible respiratory immune responses by oseltamivir treatment in mice infected with influenza A virus. Microbes Infect. 2010. 12:778–783.
19. Li IW, Hung IF, To KK, Chan KH, Wong SS, Chan JF, Cheng VC, Tsang OT, Lai ST, Lau YL, et al. The natural viral load profile of patients with pandemic 2009 influenza A(H1N1) and the effect of oseltamivir treatment. Chest. 2010. 137:759–768.
20. Hancock K, Veguilla V, Lu X, Zhong W, Butler EN, Sun H, Liu F, Dong L, DeVos JR, Gargiullo PM, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009. 361:1945–1952.
21. Jackson ML, France AM, Hancock K, Lu X, Veguilla V, Sun H, Liu F, Hadler J, Harcourt BH, Esposito DH, et al. Serologically confirmed household transmission of 2009 pandemic influenza A (H1N1) virus during the first pandemic wave-New York City, April-May 2009. Clin Infect Dis. 2011. 53:455–462.
22. Chao DY, Cheng KF, Hsieh YH, Li TC, Wu TN, Chen CY, Tsai CA, Chen JH, Chiu HT, Lu JJ, et al. Serological response and persistence in schoolchildren with high baseline seropositive rate after receiving 2009 pandemic influenza A (H1N1) vaccine. Vaccine. 2011. 29:617–623.
23. Choi YS, Baek YH, Kang W, Nam SJ, Lee J, You S, Chang DY, Youn JC, Choi YK, Shin EC. Reduced antibody responses to the pandemic (H1N1) 2009 vaccine after recent seasonal influenza vaccination. Clin Vaccine Immunol. 2011. 18:1519–1523.
24. Skowronski DM, De Serres G, Crowcroft NS, Janjua NZ, Boulianne N, Hottes TS, Rosella LC, Dickinson JA, Gilca R, Sethi P, et al. Association between the 2008-09 seasonal influenza vaccine and pandemic H1N1 illness during Spring-Summer 2009: four observational studies from Canada. PLoS Med. 2010. 7:e1000258.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download