Abstract
Interleukin-1 receptor antagonist (IL-1ra), tumor necrosis factor soluble receptors (sTNF-R) type I and II, and regulated upon activation, normal T-cell expressed and secreted (RANTES) play an important role in the modulation of primary glomerulonephritis (GN) course. The aim of the study was to assess whether pre-treatment measurements of IL-1ra, sTNF-R, and RANTES assessed conjointly may be useful as predicting factors in patients with GN. In 84 patients (45 males and 39 female) serum concentration (pg/mL) and urinary excretion (pg/mgCr) of cytokines were measured. After 12 months of therapy with steroids and cyclophosphamide the patients were divided into two subgroups: Responders (R) and Non-Responders (NR) according to the treatment results. The urinary IL-1ra, TNF-RI and RII were significantly higher in R than NR (1,732 vs 646 with P < 0.001, 13.1 vs 6.3 with P = 0.005, and 33.6 vs 14.4 with P = 0.012). The urinary RANTES excretion was increased in NR (79.6 vs 28.5; P < 0.001). The multivariable analysis showed that if conjointly assessed, only urinary IL-1ra, TNF-R I and R II, RANTES with 85% probability pointed the feature remission (R). In conclusion, the urinary excretion of IL-1ra, TNF-R I and R II, and RANTES examined conjointly are effective in predicting favorable response to immunosuppressive treatment in patients with GN.
It has been well documented that both interleukin-1 and tumor necrosis factor are major pro-inflammatory cytokines and their continuous or uncontrolled release may lead to activation of local immunological response in the kidneys (1, 2). Some authors assume that cytokine receptors and antagonists may serve as sensitive and specific markers of their activity (3). Several studies have also demonstrated that interleukin -1 receptor antagonist (IL-1ra) and soluble tumor necrosis factor receptors (sTNF-R I and II) may modulate inflammatory reactions by decreasing the activity of locally produced IL-1 and TNF (4-6). Thus we assume that measuring IL-1ra and TNFR I, II serum concentration and their urinary excretion may be helpful in the assessment of the initial activity of the glomerular disease and a subsequent response to immunosuppressive treatment. Regulated upon Activation, Normal T-cell Expressed and Secreted (RANTES) in patients with primary glomerulonephritis has been isolated from tubular epithelial cells. Once expressed, it may increase the risk of renal impairment (7).
Patients with primary glomerulonephritis (GN) are often affected by kidney failure. This unfavorable outcome is generated by a glomerular influx of activated inflammatory cells-glomerular injury and interstitial tissue damage with subsequent fibrosis. The introduction of aggressive immunosuppressive therapy comprising of corticosteroids and cyclophosphamide has significantly improved GN outcome in the majority of patients. However, a minority independent of glomerulonephritis grade may still be resistant to immunosuppressive regimens, despite routine treatment. Therefore in severe courses of GN an aggressive therapy still remains a clinical trial and may be instituted in patients who would not have remission but only a series of adverse events during the treatment. The optimization and individualization of the treatment should multiply the chances for remission making it more adequate. The pre-treatment assessment of IL-1ra, TNF-R, and RANTES may become an argument which may help to decide whether aggressive therapy should be introduced or resigned.
The aim of the study was to evaluate the potential of conjointly examined IL-1ra, TNF-R I and II and RANTES serum concentration (s) and urine excretion (u) in predicting the response to immunosuppressive treatment in patients with primary glomerulonephritis.
The study was conducted on 84 primary glomerulonephritis patients (45 males and 39 females) whose mean age was 41.44 ± 13.25 yr. The control group consisted of 18 age-matched healthy subjects. The structure of the study group (including glomerulonephritis subgroups) and the control group is shown in Table I. Only patients with severe course of GN i.e. nephrotic range proteinuria or deterioration of kidney function (indicated by an increase of serum creatinine concentration of more than 50% of the baseline, obtained on the first visit in outpatient clinic) were included in this study. The diagnosis was based on clinical symptoms, laboratory tests and kidney biopsy. All biopsy specimens were evaluated by light and immunofluorescence microscopy, and followed by a computerized morphometric analysis of interstitium quantity which was also used to calculate interstitial volume percentage (8, 9). The degree of interstitial mononuclear cell infiltration glomerulosclerosis (GSC) was examined on the basis of number of involved glomeruli. Intraglomerular extent of sclerosis was semi-quantitatively estimated according to a scoring system proposed by Fuiano et al. (10). The GSC was graded 0, 1, 2, or 3, corresponding respectively to mild, moderate, and severe. The type of primary glomerulonephritis was made by microscopic evaluation. Mesangio-prolifetative GN diagnosis was established after the exclusion of other proliferative glomerulonephritis (8-10).
Kidney function was evaluated according to serum creatinine (Cr) concentration (normal range 0.7 to 1.3 mg/dL). Also objective measurements of the urinary excretion of proteins were expressed in milligrams per milligram of creatinine in urine (mg/mg Cr). This calculation allowed to avoid the pitfall of different temporary urinary excretion and made it independent to kidneys preserved or affected function. All participants were treated with antihypertensive drugs (angiotensin converting enzyme inhibitors and calcium channel blockers) to establish and maintain blood pressure values according to recommendations (11, 12). Also statins were administrated to stabilize lipid profile (atorvastatin in mean dose of 20 mg/day). The primary aim of statin administration was to reduce low density lipoprotein (LDL) serum concentration to below 100 mg/dL (13). Those variables were assessed at baseline and serially throughout the treatment to monitor status of the patients. Finally all tests were repeated 1 yr (± 3 months) after the completion of chosen immunosuppressive treatment protocol. All of the subjects received an identical immunosuppressive therapy which consisted of initial pulse therapy with methylprednisolone (a calculated aggregate dose 1,000 mg per 20 kg body weight, administered 1,000 mg in every other day) and cyclophosphamide (CPH) given once a month for six months pulses in dose 0.6 g/body surface area. The cumulative dose of cyclophosphamide did not exceed 6 g. Before the initiation of treatment, in all participants, the potential foci of infection were diagnosed and eliminated as routine. The treatment scheme including pulses of steroids and CPH was restricted to cases of progressive GN with decreasing of eGFR. The introduction of CPH treatment is controversial in some types of GN although many papers describe it as better than other immunosuppressive agents. CPH pulse treatment combined with steroids is regarded as well tolerated and effective (14-20). However to prevent adverse events of the treatment scheme H2-blockers (2 × 20 mg) and mesna (sodium 2-mercaptoethane sulfonate) injections, each of 20% of the CPH dose at intervals of 4 hr intravenously were administered to all participants in our study. Additionally the hydration was properly maintained. No CPH side effects in the period of the study were noted.
Blood and urine samples from the patients and from healthy participants were collected prospectively before the treatment to EDTA (ethylenediaminetetraacetic acid) tubes, centrifuged and stored at -70℃ until analyzed. When completed, serum concentrations and urinary excretion of interleukin-1 receptor antagonist, tumor necrosis factor receptors type I and II, RANTES were measured by enzyme-linked immunosorbent assay (ELISA) using commercial immunoassays according to the manufacturer's instructions (Biosource® Europe S.A., Nivelles, Belgium). All tests were performed in certified local laboratory. Additionally to make the results of measured urine cytokines excretion irrespective to kidney function and truly objective the results were calculated according to scheme previously described for proteinuria (i.e. calculated per urinary creatinine excretion).
After the completion of 1 yr of treatment, patients were divided into two subgroups according to their response to the therapy, i.e. R-Responders (proteinuria lower than 0.5 g/day - i.e. < 6 mg/mg urine Cr, and improved or stable kidney function) and NR-Non-Responders (proteinuria higher than 0.5 g/day-i.e. > 6 mg/mg urine Cr, and/or deterioration of kidney function). The patients subgroups divided by type of primary glomerulonephritis, are presented in Table 1.
Comparisons between patients, controls and between R and NR groups were made with the non-parametrical Mann-Whitney U test (Z). Fisher's exact probability test was used for sex comparison and Wilcoxon's rank sum test for the changes of clinical parameters during the treatment. Differences were considered significant if P was less than 0.05. The results are expressed as mean ± standard deviation.
No differences in distribution between the R and NR subgroups were noticed-Fischer's exact test and chi-square with Yates's modification. The gender structure in subgroups and control group was homogenous. The subgroups and the control group were sex and age matched. No comorbidities (including diabetes, obesity and severe infections) which may affect the final evaluation in both subgroups were noted.
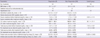
As shown in Table 2, before treatment, statistically significant differences were not observed in biopsy findings (percentage of interstitium volume and glomerulosclerosis grade) nor biochemical parameters (total serum proteins, serum creatinine concentration and protein urine excretion) between R and NR subgroups (P = 0.24 and P = 0.26). The only difference between the both subgroups was that pre-treatment LDL serum concentration (Z = 4.201, P = 0.002) increased in Non-Responders.
The post-treatment statistically significant differences observed between subgroups R and NR with regarded to total serum protein (Z = -5.490, P < 0.001), serum creatinine concentration (Z = 4.581, P < 0.001) and protein urine excretion (Z = 3.018, P = 0.003) were expected and followed from assumed subdivision to Responders and Non-Responders. Although the introduction of statins to the treatment may result in post-treatment LDL reduction, there was no statistically significant difference between its serum concentration values in R and NR subgroups (P = 0.31).
Before treatment, total serum proteins were lower in R and NR than in healthy control (Z = -5.582, P < 0.001 and Z = -5.490, P < 0.001); serum creatinine concentration was higher (Z = 3.502, P < 0.001 and Z = 4.351, P < 0.001), protein urine excretion increased (Z = 6.312, P < 0.001 and Z = 5.802, P < 0.001) and serum LDL levels were (Z = 4.019, P = 0.001 and Z = 4.299, P < 0.001), respectively higher.
The introduction of statins ameliorated LDL reduction in both subgroups, resulting in a similar serum concentration to that of the control group (P = 0.18 and P = 0.16). The results are summarized in Table 2.
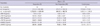
The patients in both the R and NR subgroups did not differ with respect to the pre-treatment serum concentration of IL-1ra, TNFR I and II, or RANTES (P = 0.32, P = 0.38, and P = 0.29, respectively). In contrast, the two groups demonstrated significant differences in the urinary excretion of: IL-1ra (Z = -6.243, P < 0.001), TNF-R I (Z = -2.786, P = 0.005), TNF-R II (Z = -2.517, P = 0.012) and RANTES (Z = 4.704, P < 0.001). In the Responders subgroup, the urinary excretion of IL-1ra, TNFR I and II was increased.
Serum interleukin-1 receptor antagonist concentrations were significantly lower in patients (both R and NR) than in healthy control (Z = 5.181, P < 0.001 and Z = 4.594, P < 0.001, respectively). In contrast, urinary IL-1ra excretion was decreased only in Non-Responders (Z = -3.608, P < 0.001); the Responders maintained similar with the level of excretion in control group (P = 0.11).
The serum concentration of TNF-R types I and II were higher in patients groups than in healthy control: R versus healthy sTNF-R I (Z = 5.227, P < 0.001), NR-healthy sTNF-R I (Z = 5.227, P < 0.001) and R versus healthy sTNF-R II (Z = 6.054, P < 0.001), R versus healthy uTNF-R II (Z = 5.010, P < 0.001). Similarly, TNF-R I and II urinary excretion values were increased in both patients subgroups compared to the control group: R versus healthy uTNF-R I (Z = 4.305, P < 0.001), NR versus healthy uTNF-R I (Z = 4.305, P < 0.001) and NR versus healthy sTNF-R II (Z = 5.786, P < 0.001), NR versus healthy uTNF-R II (Z = 3.785, P < 0.001).
The serum RANTES comparisons between the Responders and Non-Responders subgroups versus the control group showed highly elevated concentration R (Z = 3.020, P = 0.003) and NR (Z = 3.608, P < 0.001). Greater urinary excretion was observed in NR than in healthy subjects (Z = 2.893, P = 0.004) but no differences in uRANTES were noticed between R and the control group (P = 0.39). The results are shown in Table 3.
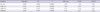
All of the biochemical data (including LDL), biopsy findings, serum concentration and urinary excretion values of uIL-1ra, uTNF-R I, II, uRANTES and chances for remission (Responders) were evaluated using logistical regression. The analysis of all the variables showed that only uIL-1ra, uTNF-R I and R II, uRANTES had a statistically significant influence on chance of remission - the Responders subgroup (R). These variables if conjointly assessed with 85% probability pointed the feature remission (R). No other parameters (biochemical or biopsy findings) demonstrated any connection with the remission (Table 4).
In the present study only the patients who demonstrated severe proteinuria and/or an increase of serum creatinine were enrolled. Subjects who did not demonstrate sustained remission after the initial steroid therapy received combined treatment with steroids and cyclophosphamide. Despite the intensive treatment no improvement in proteinuria and/or kidney function was observed in one third of the patients; in which case, their therapy was prolonged to 1 yr. It is noteworthy that no correlations between the initial biochemical or biopsy parameters and the chances for remission were observed which confirms that the clinical course of primary glomerulonephritis remains unpredictable in a substantial proportion of the patients, and therefore no uniform therapeutic strategy may be proposed based on a routine initial clinical and biochemical assessment (21).
In this study the potential usefulness of an assessment of the urinary excretion of IL-1 and TNF-α activity inhibitors, and RANTES was tested in predicting the course of GN. Although the role of those cytokines in the induction of inflammatory reactions remains well established, the complex assessment of their antagonists has rarely been a subject of clinical investigations (5, 22, 23).
Injections of IL-1ra have been shown to arrest the inflammatory reactions in the kidneys in several experimental models of glomerulonephritis (4). Chen et al. (24) observed that intraperitoneal administration of IL-1ra led to a decrease of proteinuria, hematuria and partially prevented the progression of spontaneously occurring experimental IgA nephritis in mice. Therefore it can be assumed that the amount of IL-1ra produced and/or excreted by patients with primary glomerulonephritis could be related to the disease prognosis. In the presented study IL-1ra serum concentrations were lower in the patients than in the controls. In contrast, uIL-1ra concentrations in Responders was similar to IL-1ra urinary excretion in healthy controls and nearly three times higher than in Non-Responders. These findings may suggest that urinary excretion and not serum concentration, of IL-1ra may indicate its anti-inflammatory activity. Furthermore, lower serum and urinary levels of IL-1ra in NR may be explained by the binding of IL-1ra to excessively synthesized IL-1; these conglomerates are prevented from penetrating to the urine by their size (23), which reduces their protective potency.
Although IL-1ra treatment is ineffective in the induction phase of glomerular injury, it may significantly suppress the progression of tubulointerstitial changes and renal impairment by preventing leukocyte infiltration (4). However, IL-1 up-regulates the expression of VCAM-1 and ELAM-1 and may inhibit their induction (4). The results of this study suggest that increased IL-1ra excretion in urine may reflect its tissue protecting and anti-inflammatory roles. A tubulointerstitial injury was also assessed by measuring the percentage of interstitial volume in kidney biopsy specimens and assessing the glomerulosclerosis grade. The percentage of interstitium in the Non-Responders subgroup tended to be higher than in the Responders subgroup but that difference was not statistically significant. The systemic administration of both IL-1 and TNF or RANTES may exacerbate not only glomerular but also tubulointerstitial injury (25, 26).
It is well known that TNFα takes part in the induction of the inflammatory reaction. Its activity may be modulated by two types of receptors (I and II) existing as membrane or soluble forms (27). The pro-inflammatory effects of TNF may be inhibited by increased expression of its soluble receptors (1). In the present study, the urinary excretion of TNF soluble receptors was higher in the R than in the NR subgroup and also higher than in the controls. That suggests that increased production of TNF receptors may be secondary to inflammatory reactions which develop in the course of GN. Increased TNF receptor levels may, hence, be a part of the natural anti-inflammatory response. Their protective role has been confirmed in experimental models in which the neutralization of TNFα with its soluble receptors effectively prevented inflammation and glomerular injury (1).
The significantly decreased RANTES urinary excretion values in the R in comparison to the NR subgroup and the similar uRANTES values between the R group and healthy participants suggest its involvement in kidney injury mechanisms (26). Under physiological conditions, RANTES is produced by all the tissues of the kidney, and its secretion is increased by any damaging factor as well as by IL-1 and TNF. RANTES expression occurs mainly in cells and the tubular mesangium (28). The presence of RANTES is one of the factors which cause tubular and interstitial changes, as confirmed in experimental studies of anti-GBM GN and in humans (26). Proteinuria, the main symptom of primary glomerulonephritis, increases the migration of macrophages and T lymphocytes increasing the expression of RANTES (26).
Since tubulointerstitial fibrosis, but not just glomerular changes, had been linked to the deterioration of kidney function (9) it was decided to carry out a computerized morphometric analysis of the interstitium to study the relationship between chronic renal damage and renal function. Computer-assisted quantification of fibrosis appears to be a useful prognostic indicator in primary glomerulonephritis (9). In the present study, the percentage of interstitium volume in biopsy specimens evaluated in light microscopy was calculated to describe the degree of tubulointerstitial injury. It is noteworthy that not only the biopsy findings but also the parameters of kidney function (i.e. initial serum creatinine concentration and proteinuria) did not predict the patients' chances for remission. Currently, the standard biopsy result may establish a diagnosis of glomerulonephritis and describes the stage of kidney injury in most cases by enumerating the glomeruli involved and describing interstitum infiltration or tubular damage (9, 29). However, no matter how precise the biopsy interpretation, the nephrologists institutes the therapy based on the patient's clinical status, fluctuations in biochemical parameters and his own experience. A criterion differentiating treatment according not only to primary glomerulonephritis type would be a valuable tool in the diagnostic process (30-34). The obligation of treatment individualization shall still rest with the clinician.
It is discouraging that few reliable markers exist that can predict the outcomes of primary glomerulonephritis and few indications, which can establish fail-safe immunosuppressive regiments. Despite all of those disadvantages, nephrologists are not released from the obligation of optimizing therapy.
In this study, the increased urinary excretion but not the serum concentration of IL-1ra, TNF R I and II indicates a good prognosis for remission after immunosuppressive treatment in patients with primary glomerulonephritis, and increased RANTES urinary excretion indicates a worse course of GN.
Although there are many doubts whether the measurements of cytokines and their inhibitors may be useful in predicting a prognosis of GN, it appears that the urinary excretion of IL-1ra, TNF-R I, TNF-R II and RANTES examined conjointly suggests the opposite. The examinations of IL-1ra, TNF R I and II, RANTES seem to be effective in predicting the results of immunosuppressive treatment and argue for its optimization, and dose individualization, which may reduce patients' therapy risk and even prevent unnecessary complications inseparably connected with inadequate immunosuppressive treatment.
This study had some limitations. This was a single center study so that the sample size was rather small, thus the evaluation of particular types of GN would increase limitations. Therefore the retrospective analysis according to response to the immunosuppressive therapy in entire cohort was performed. The statistical analysis was restricted to non-parametrical tests due to participants' number. Additionally, as shown, a few outliners were included what is easily noticeable especially in urinary IL-1ra.
In this study only a selected group of patients with aggressive course of GN were evaluated and immunosuppressive treatment protocol selected in the site was not widely accepted, but undoubtedly efficient (14-20). However, described disadvantages should not influence pre-treatment variables analysis or multivariable logistic evaluation indicated selected cytokines as exclusively contributory predictor of therapy outcomes.
In conclusion, the urine excretions of IL-1ra, soluble TNF-R I and II, and RANTES examined conjointly are effective in predicting the good response to immunosuppressive treatment in patients with primary glomerulonephritis.
Figures and Tables
Table 1
The structure of the study group according to primary glomerulonephritis type and the control group
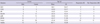
Table 2
Biopsy findings and biochemical parameters in the Responders and the Non-Responders subgroups
References
1. Karkar AM, Smith J, Pusey CD. Prevention and treatment of experimental crescentic glomerulonephritis by blocking tumor necrosis factor alpha. Nephrol Dial Transplant. 2001. 16:518–524.
2. Noronha IL, Fujihara CK, Zatz R. The inflammatory component in progressive renal disease: are intervention possible? Nephrol Dial Transplant. 2002. 17:363–368.
3. Roux-Lombard P, Fenner H, Dayer JM. Relation between soluble adhesion molecule, TNFα and TNF soluble receptors serum levels in patients with systemic lupus erythematosus and systemic vasculitis. Lupus. 1995. 4:110–115.
4. Lan HY, Nicolic-Paterson DJ, Zarama M, Vannice JL, Atkins RC. Suppression of experimental crescentic glomerulonephritis by the interleukin-1 receptor antagonist. Kidney Int. 1993. 43:479–485.
5. Wei-An H, Shui-Ling L, Tan-Shiny Y, Kuo-Tong H, Hey-Chi H, Chien-Chen T. Serum and urinary soluble tumor necrosis factor receptors in patients with glomerular diseases: correlation with disease severity and prognosis. Nephrol Dial Transplant. 1997. 26:762–770.
6. Timoshanko JR, Kitching AR, Iwakura Y, Holdsworth SR, Tipping PG. Leukocyte-derived interleukin-1beta interacts with renal interleukin-1 receptor I to promote renal tumor necrosis factor and glomerular injury in murine crescentic glomerulonephritis. Am J Pathol. 2004. 164:1967–1977.
7. Mezzano SA, Droguett MA, Burgos ME, Ardiles LG, Aros CA, Caorsi I, Edigo J. Overexpression of chemokines, fibrogenic cytokines and myofibroblasts in human membranous nephropathy. Kidney Int. 2000. 57:147–158.
8. D'amico G. Tubulo-interstitial damage in glomerular diseases: its role in the progression of the renal damage. Nephrol Dial Transplant. 1998. 13:80–85.
9. Okoń K, Sułowicz W, Smoleński O, Sydor A, Chruściel B, Kirker-Nowak A, Rosiek Z, Sysło K, Stachura J. Predicting kidney function from renal biopsy. Semiquantitative versus quantitative approach. Pol J Pathol. 2007. 58:65–71.
10. Fuiano G, Sund S, Mazza G, Rosa M, Caglioti A, Gallo G, Natale G, Andreucci M, Memoli B, De Nicola L, et al. Renal hemodynamic response to maximal vasodilating stimulus in healthy elderly subjects. Kidney Int. 2001. 59:1052–1058.
11. Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res. 2009. 32:3–107.
12. Fujita T, Ando K, Nishimura H, Ideura T, Yasuda G, Isshiki M, Takahashi K. Cilnidipine versus amlodipine randomised trial for evaluation in renal disease (CARTER) study investigators. Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin-angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int. 2007. 72:1543–1549.
13. Kidney Disease Outcomes Quality Initiative (K/DOQI) Group. K/DOQI clinical practice guidelines for managing dyslipidemias in chronic kidney disease. Am J Kidney Dis. 2003. 41:I–IV. S1–S91.
14. Yuan J, Fang W, Zhang W, Ni Z, Qian J. Effective and well tolerated treatment of nephrotic idiopathic membranous nephropathy with monthly i.v. pulse cyclophosphamide and oral steroids: a single centre's retrospective study. Nephrology. 2011. 16:440–445.
15. Menon S, Valentini RP. Membranous nephropathy in children: clinical presentation and therapeutic approach. Pediatr Nephrol. 2010. 25:1419–1428.
16. Cucer F, Miron I, Müller R, Iliescu H, Codruta M. Treatment with cyclophosphamide for steroid-resistant nephrotic syndrome in children. Maedica (Buchar). 2010. 5:167–170.
17. van Husen M, Kemper MJ. New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol. 2011. 26:881–892.
18. Naseri M, Madani A, Ataei N. Correlation between prognosis and response to treatment in children with FSGS. Acta Med Iran. 2009. 47:93–96.
19. Oshima S, Kawamura O. Long-term follow-up of patients with IgA nephropathy treated with prednisolone and cyclophosphamide therapy. Clin Exp Nephrol. 2008. 12:264–269.
20. Yagi K, Yanagida H, Sugimoto K, Kuwajima H, Tabata N, Morita K, Okada M, Takemura T. Clinicopathologic features, outcome, and therapeutic interventions in four children with isolated C3 mesangial proliferative glomerulonephritis. Pediatr Nephrol. 2005. 20:1273–1278.
21. McQuarrie EP, Shakerdi L, Jardine AG, Fox JG, Mackinnon B. Fractional excretions of albumin and IgG are the best predictors of progression in primary glomerulonephritis. Nephrol Dial Transplant. 2011. 26:1563–1569.
22. Tesar V, Jirsa M Jr, Zima T, Kalousová M, Bartunková J, Stejskalová A, Dostál C, Zabka J. Soluble cytokine receptors in renal vasculitis and lupus nephritis. Med Sci Monit. 2002. 8:BR24–BR29.
23. Kacprzyk F. Serum levels and urinary excretion of soluble receptors for tumor necrosis factor (sTNFR R) in patients with primary glomerulonephritis. Pol Arch Med Wewn. 2002. 107:215–221.
24. Chen A, Sheu LF, Chou WY, Tsai SC, Chang DM, Liang SC, Lin FG, Lee WH. Interleukin-1 receptor antagonist modulates the progression of a spontaneously occurring IgA nephropathy in mice. Am J Kidney Dis. 1997. 30:693–702.
25. Wardle EN. Cytokine growth factors and glomerulonephritis. Nephron. 1991. 57:257–261.
26. Haberstroh U, Pocock J, Gómez-Guerrero C, Helmchen U, Hamann A, Gutierrez-Ramos JC, Stahl RA, Thaiss F. Expression of chemokines MCP-1/CCL2 and RANTES/CCL5 is differentially regulated by infiltrating inflammatory cells. Kidney Int. 2002. 62:1264–1276.
27. Lan HY. Therapeutic effects of cytokine blockade in glomerulonephritis. Nephrol Dial Transplant. 1998. 13:7–9.
28. Wolf G, Aberle S, Thaiss F, Nelson PJ, Krensky AM, Neilson EG, Stahl RA. TNFα induces expression of the chemotractant cytokine RANTES in cultured mouse mesangial cell. Kidney Int. 1993. 44:795–804.
29. Howie AJ, Ferreira MA, Adu D. Prognostic value of simple measurement of chronic damage in renal biopsy specimens. Nephrol Dial Transplant. 2001. 16:1163–1169.
30. Coppo R, Ponticelli C. Ponticelli C, Glassock RJ, editors. Minimal change nephropathy. Treatment of primary glomerulonephritis. 2009. Oxford: Oxford University Press;179–210.
31. Scolari F, Ponticelli C. Ponticelli C, Glassock RJ, editors. Focal and segmental glomerulosclerosis. Treatment of primary glomerulonephritis. 2009. Oxford: Oxford University Press;215–256.
32. Passerini P, Ponticelli C. Ponticelli C, Glassock RJ, editors. Membranous nephropathy. Treatment of primary glomerulonephritis. 2009. Oxford: Oxford University Press;261–308.
33. Glassock RJ, Lee G. Ponticelli C, Glassock RJ, editors. Immunoglobulin A nephropathy. Treatment of primary glomerulonephritis. 2009. Oxford: Oxford University Press;313–361.
34. Glassock RJ. Ponticelli C, Glassock RJ, editors. Membranoprolipherative glomerulonephritis. Treatment of primary glomerulonephritis. 2009. Oxford: Oxford University Press;375–393.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download