Abstract
The cardiovascular system may be one of the target organs of both immunoglobulin G4 related and non-related systemic multifocal fibrosclerosis. We present a case of IgG4 non-related systemic multifocal fibrosclerosis mimicking mitral stenosis on echocardiography. For a more detailed differential diagnosis, we used multimodal imaging techniques. After surgical biopsy around the abdominal aortic area in the retroperitoneum, histological examination revealed IgG4 non-related systemic multifocal fibrosclerosis. We describe the multimodal imaging used to diagnose IgG4 non-related systemic multifocal fibrosclerosis and a positive response to steroid treatment. There have been no previous case reports of IgG4 non-related systemic multifocal fibrosclerosis with intracardiac involvement. Here, we report a case of IgG4 non-related systemic multifocal fibrosclerosis mimicking mitral stenosis.
Immunoglobulin G4-related sclerosing disease (IgG4-RSD) is a new clinical disease entity characterized by elevated serum IgG4 concentration and tumorous lesions or tissue infiltration by IgG4-positive plasma cells (1-3). This disease may present with simultaneous or metachronous lesions in multiple organs such as pancreatitis, biliary sclerosis, retroperitoneal and mediastinal fibrosis, inflammatory pseudotumor of the lung and liver, and interstitial nephritis (4-6). Immunoglobulin G4 non-related sclerosing disease (IgG4 non-RSD) is the contrary concept in immunohistochemical pathology findings.
The diagnosis of IgG4-RSD and IgG4 non-RSD are both based on histological appearance. The three classical morphological features are 1) dense lymphoplasmacytic infiltration, 2) fibrosis arranged at least focally in a storiform pattern, and 3) obliterative phlebitis (6). For diagnosis of these diseases, biopsy and tissue confirmation about histopathologic finding is the important (7). Comprehensive diagnostic criteria for IgG4-RSD consisting of three items has been established, 1) organ enlargement, mass or nodular lesions, or organ dysfunction, 2) a serum IgG4 concentration > 135 mg/dL, and 3) histopathological findings of > 10 IgG4+cells/HPF and an IgG4+/IgG+cell ratio > 40% (8, 9).
While our case had similar systemic clinical manifestations like IgG4-related sclerosing disease, it had the inconsistent laboratory and histopathologic findings. Furthermore, the disease was localized at the intracardiac space, which is an uncommon site. Ultimately, this case was diagnosed as IgG4 non-RSD.
We herein report a case of IgG4 non-related periaortitis with retroperitoneal fibrosis and an intracardiac mass.
A 70-yr-old woman came to an emergency department with aggravation of dyspnea of three months duration at 7th July in 2012. Her vital signs were stable, and physical examination did not reveal any significant findings. Initially, electrocardiogram showed the ordinary finding as normal sinus rhythm and left ventricular hypertrophy. The transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) showed a left atrial (LA) mass-like lesion attached to the anterior leaflet of the mitral valve (MV), which could be suggestive of thrombus, tumor, or severe mitral stenosis (MS) (Fig. 1A, B). This mass-like lesion occurred functional MS that the mean pressure gradient (mean PG) of MV was measured as 15.2 mmHg. In addition, the patient had moderate pulmonary hypertension with a measured right ventricular systolic pressure (RVSP) of 69 mmHg. The patient's past medical history was significant, with an operation for an intradural extramedullary spinal cord tumor at thoracic vertebrae 3-5 in 2007.
Laboratory tests showed elevated erythrocyte sedimentation rate (ESR, 120 mm/hr) and C-reactive protein (CRP, 7.42 mg/dL). Abdominal computed tomography (CT) demonstrated localized aortitis involving the proximal abdominal aorta with a periaortic cuff of soft tissue and mild calcifications (Fig. 1C). Abdominal CT was performed to identify and decide an available biopsy site around the periaortic area.
We also conducted other image modalities. It was the reason that we wanted to obtain more evidences, because we could not confirm the definite diagnosis or characterization about this mass inside the heart by echocardiography. Coronary CT angiography showed diffuse soft-tissue infiltration (Fig. 1E). Cardiac magnetic resonance imaging (MRI) findings, which were discerning for thrombus and tumor, were indicative of a mass diffusely involving the LA wall, MV, interatrial septum (IAS), and aortomitral continuity, resulting in severe MS that was likely a mass such as lymphoma rather than a thrombus and wall thickening involving the LA with extension to the MV leaflet (Fig. 1D).
Additionally, it was necessary to be excluded that this mass might have the potency of malignancy and the lesion of other metastatic site. Positron emission tomography (PET) is the ideal imaging modality recognizing the inflammatory or malignancy lesion as the degree of standardized uptake value (SUV) and detecting the metastatic lesion. In this patient, the result of PET indicated highly active metabolic inflammation in the ascending aorta, abdominal aorta and right proximal common iliac artery. The increased fludeoxyglucose (FDG) uptake in the LA and septum of the heart suggested that an active inflammatory lesion was more likely (Fig. 1F).
Excisional biopsy of the aorta wall mass revealed lymphoplasmacytic infiltration and fibrosis (Fig. 2A). The infiltrate was granulomatous with central microabscess. The abundant plasma cells stained for CD38 and IgG (Fig. 2C, D). Additionally, Masson's trichrome stain showed adventitial fibrosis (Fig. 2B). However, only 5% of the plasma cells stained for IgG4 (Fig. 2E, F), which was suggestive of IgG4 non-related sclerosing periaortitis.
The finding of IgG4-positive plasma cells within the aortic wall led us to perform additional serologic investigations. Serum IgG levels were found to be substantially increased (1969 mg/dL). Serum IgG4 level was normal at 53 mg/dL. Serum and urine protein electrophoresis demonstrated normal patterns aside from a peak in the gamma region.
The patient was prescribed prednisolone (1 mg/kg/day for 4 weeks). She continued taking 60 mg/day of prednisolone for four weeks, after which the dosage was tapered. By the time she completed 12 weeks of treatment, her ESR level had dramatically decreased to 6 mm/hr and CRP had decreased to 0.1 mg/dL. Dyspnea was completely relieved by steroid administration. TTE showed that the size of the LA mass had decreased (Fig. 3A). In hemodynamic parameters, mean PG was improved as 4.42 mmHg and RVSP as 45 mmHg was also better than previous results. Coronary CT angiography, cardiac MRI demonstrated the decreased extent of soft tissue lesion arounding the LA and MV after steroid treatment (Fig. 3B, C). We could not find the inflammatory mass-like lesion of periabdominal aortic area in PET (Fig. 3D).
We describe here what we believe to be the first reported case of IgG4 non-related sclerosing disease associated with the diffuse intracardiac involvement of IAS and MS. These dense lymphoplasmacytic infiltrative and fibrotic multiorgan lesions may occur synchronously or metachronously (2, 10-12), and the patient's history of an intradural extralmedullary spinal cord tumor was related to the intracardiac mass and abdominal aorta wall thickness in this event. Thus, these manifestations were considered to be part of the same disease entity. And the initial symptom dyspnea was supposed to be associated with valvular heart disease induced heart failure sign.
There are no significant differences between IgG4-related and IgG4 non-related inflammatory disease in terms of macroscopic findings (11). In this case, we experienced a patient with abdominal aorta wall fibrosis and an intracardiac mass who had normal serum IgG4 levels, and ultimately found that the clinical features and the good response to steroid treatment in the IgG4-related and IgG4 non-related sclerosing diseases were similar.
Sclerosing periaortitis or aortitis explained the mediastinal or retroperitoneal fibrosis, and IgG4-related sclerosing periaortitis involving multiple organs progressing to include the cardiovascular system has been found recently (13, 14). Sclerosing periaortitis is classified as IgG4-related or IgG4 non-related based on immunohistochemical staining. IgG4 non-RSD is a newly recognized disorder that may manifest as thoracic aortitis, inflammatory abdominal aortic aneurysm, retroperitoneal fibrosis, or intracardiac mass.
A more comprehensive understanding of this disease may provide insight into its diagnosis and management. Unlike IgG4-related sclerosing disease, we cannot infer a steroid therapy response based on serum IgG4 levels in IgG4 non-related sclerosing disease. Therefore, further investigation of appropriate therapy response parameters in IgG4 non-related sclerosing disease is necessary.
Figures and Tables
 | Fig. 1The main remarks of several imaging modalities before steroid treatment. (A) Parasternal long axis view of TTE demonstrated limited motion of mitral leaflet by attached mass like lesion (white circle). (B) The mid-esophageal 4-chamber view of TEE demonstrated LA mass-like lesion (two white arrows). Color Doppler imaging showed flow acceleration as MS. (C) Transverse view of abdominal CT demonstrated increased wall thickness of the abdominal aorta (white arrow). (D) Cardiac MRI demonstrated wall thickening (white arrow) involving LA and IAS with extension to MV leaflet. (E) Coronary CT angiography showed diffuse soft-tissue infiltration involving LA, IAS, and MV. (F) PET showed LA mass (white arrow) and periabdominal aortic area thickness (white arrow in little figure) increased FDG uptake. |
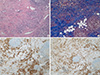 | Fig. 2The histopathologic results by the biopsy of periabdominal aortic mass. (A) Hematoxylin and eosin stained section of the biopsied periabdominal aortic mass demonstrated dense lymphoplasmacytic infiltration and fibrosis. (B) Masson's trichrome stain showed adventitial fibrosis. (Original magnification A, B, ×100). (C) Immunohistochemical staining for IgG. (D) Immunohistochemical staining for CD38. Immunohistochemical staining for IgG4. Below 5% of the plasma cells exhibit this stain. (Original magnification C, ×100; D, ×200). IgG, immunoglobulin G. |
 | Fig. 3The improved findings of a few images after steroid treatment for four weeks. (A) Follow-up at the four weeks of steroid treatment showed that the thickness of LA mass decreased (white circle) in TTE. (B) Coronary CT angiography showed interval decreased extent of soft tissue lesion (black arrow) arounding LA after steroid treatment. (C) Cardiac MRI showed the decreased lesion of MV after four weeks from the point of starting steroid treatment. (D) PET did not show any lesion in LA and periabdominal aortic area after six months from the point of starting steroid treatment. |
References
1. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–551.
2. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Sumida T, Mimori T, Tanaka Y, et al. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol. 2012; 22:1–14.
3. Masaki Y, Kurose N, Umehara H. IgG4-related disease: a novel lymphoproliferative disorder discovered and established in Japan in the 21st century. J Clin Exp Hematop. 2011; 51:13–20.
4. Kamisawa T, Okamoto A. IgG4-related sclerosing disease. World J Gastroenterol. 2008; 14:3948–3955.
5. Stone JH, Khosroshahi A, Deshpande V, Chan JK, Heathcote JG, Aalberse R, Azumi A, Bloch DB, Brugge WR, Carruthers MN, et al. Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum. 2012; 64:3061–3067.
6. Zen Y, Nakanuma Y. IgG4-related disease: a cross-sectional study of 114 cases. Am J Surg Pathol. 2010; 34:1812–1819.
7. Masaki Y, Dong L, Kurose N, Kitagawa K, Morikawa Y, Yamamoto M, Takahashi H, Shinomura Y, Imai K, Saeki T, et al. Proposal for a new clinical entity, IgG4-positive multiorgan lymphoproliferative syndrome: analysis of 64 cases of IgG4-related disorders. Ann Rheum Dis. 2009; 68:1310–1315.
8. Umehara H. A new clinical entity: IgG4-related disease (IgG4-RD) discovered in the 21st century. Intern Med. 2012; 51:821–822.
9. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, Matsui S, Yoshino T, Nakamura S, Kawa S, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012; 22:21–30.
10. Okazaki K, Umehara H. Are classification criteria for IgG4-RD now possible? the concept of IgG4-related disease and proposal of comprehensive diagnostic criteria in Japan. Int J Rheumatol. 2012; 2012:357071.
11. Kasashima S, Zen Y, Kawashima A, Endo M, Matsumoto Y, Kasashima F. A new clinicopathological entity of IgG4-related inflammatory abdominal aortic aneurysm. J Vasc Surg. 2009; 49:1264–1271.
12. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, Okamoto A, Egawa N, Nakajima H. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–984.
13. Stone JR. Aortitis, periaortitis, and retroperitoneal fibrosis, as manifestations of IgG4-related systemic disease. Curr Opin Rheumatol. 2011; 23:88–94.
14. Ishizaka N, Sakamoto A, Imai Y, Terasaki F, Nagai R. Multifocal fibrosclerosis and IgG4-related disease involving the cardiovascular system. J Cardiol. 2012; 59:132–138.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download