Abstract
The necessity of routine prostate biopsy prior to transurethral resection of the prostate (TURP) in elderly comorbid patients with a high prostate specific antigen (PSA) level remains controversial. We assessed the role of TURP in prostate cancer diagnosis in these individuals. A total of 197 patients underwent TURP in conjunction with prostatic needle biopsy. Pathologic reviews of specimens of TUR chips and biopsy cores were analyzed. Overall, prostate cancer (CaP) was detected in 114 patients (57.6%). Ninety-eight cancers (86%) were detected with TURP and biopsy, and seven cancers (6.1%) with only TURP. The Gleason score of a TUR-specimen was identical to that of the biopsy-core in 43.9% of cases. Variables associated with diagnostic accuracy in the TUR-specimens included the prebiopsy PSA level, prostate specific antigen density (PSAD), and the Gleason score in biopsy cores. In patients with a PSA level and a PSAD that was greater than 15.4 ng/mL and 0.69 ng/mL/g, respectively, 100% of the cancers were detected in the TUR-specimens. Our results suggest that a prostatic biopsy might be omitted prior to TURP in elderly patients with significant co-morbidity and levels for PSA of >15.4 ng/mL.
Prostate biopsy is the recommended diagnostic method for clinical suspicion of prostate cancer (CaP), eg high prostate specific antigen (PSA), abnormal digital rectal examination (DRE), suspicious lesion on transrectal ultrasound (TRUS) (1). However, there is no consensus on routine prostate biopsy prior to transurethral resection of the prostate (TURP) in patients who are elderly and have significant co-morbidity. There are three diagnostic options. First, the TURP is carried out on the second day after a prostate biopsy. These procedures are associated with considerable cost, discomfort and the risk of infection or hematuria (2, 3). Prostate biopsies are known to increase the incidence of side effects in patients of an advanced age (4). In the second option, a prostatic needle biopsy and TURP are carried out in one session, intraoperatively. Though this strategy is an efficient treatment and could minimize patient discomfort, it requires more under-anesthesia time and increased hospitalization costs. For the third option, if the diagnostic accuracy of a transurethral resection (TUR)-derived specimen is confirmed, some patients could possibly omit the prostatic biopsy. Local curative treatments (such as radical prostatectomy) are not suitable for patients who are elderly, even with significant co-morbidity and androgen deprivation therapy or other types of palliative therapy are more proper for patients with life expectancies of less than 10 yr for CaP (5, 6). Moreover, TURP is now ranked as a palliative therapy used mainly to relieve obstruction caused by CaP (7). Thus, TURP may be useful in such a clinical scenario. However, there is concern that this approach may result in a missed diagnosis of CaP. Reports of the diagnostic accuracy of TUR-derived tissue often differ according to the study design (8-11). To the best of our knowledge, reports of the diagnostic accuracy of TUR-derived tissue in patients with biopsy-proven CaP are rare.
In the present study, the pathological results of a specimen obtained from TURP and from a biopsy core were compared to assess the diagnostic accuracy relative to cancer detection and histologic grading of a TUR-derived specimen. Moreover, we assessed the cut-off values that would confer the optimal sensitivity and specificity for cancer detection in TUR-derived specimens.
We retrospectively reviewed the medical records of 197 patients who underwent TURP in conjunction with a 12-core prostatic needle biopsy. All patients were judged unsuitable for local definitive treatment because of a decreased life expectancy and/or severe comorbidities. Transrectal biopsies were performed with a spring-lodged autonomic biopsy gun equipped with an 18-gauge biopsy needle (Magnum, 15 mm, Bard, Covington, GA, USA) under the TRUS. The 12-core TRUS biopsy (including a 2-core transition zone biopsy) protocol was performed, and additional cores were sampled as hypoechoic lesions were observed on the TRUS. All patients' charts were evaluated retrospectively, including PSA, prostate size based on TRUS, TURP results (including resection weight and pathology report), and TRUS biopsy results (including positive core number and location). PSA was measured using a Tandem-R assay. The prostate volume was calculated using the following formula: width×length×height×0.52. Prostate specific antigen density (PSAD) was calculated by dividing the PSA by the prostate volume. The pathologic review of prostate specimens obtained from TURP and biopsy were deciphered by a pathologist at our institute applying the 2005 International Society of Urological Pathology (ISUP) consensus (12). The TURP procedure was comprised of removing the adenoma from the transitional zone and the resection plane advanced to the surgical capsule by two experienced surgeons.
Statistical analysis was performed by use of a Student's t-test and the Mann-Whitney U test for continuous variables. Receiver operating characteristic (ROC) curves were constructed to obtain the cut-off values that would confer optimal sensitivity and specificity for cancer detection in TUR-derived specimens. The software used for the statistical analyses was SPSS 20.0 software (SPSS Inc., Chicago, IL, USA), and a P value<0.05 was considered statistically significant.
The collection and analyses of all samples was approved by the institutional review board of Chungbuk National University, and informed consent was obtained from each subject (IRB approval number 2006-01-001).
The biospecimens for this study were provided by the Chungbuk National University Hospital, a member of the National Biobank of Korea, which is supported by the Ministry of Health, Welfare and Family Affairs. All samples derived from the National Biobank of Korea were obtained with informed consent under institutional review board-approved protocols.
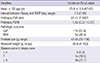
Table 1 lists the baseline characteristics of the 197 patients. The mean interval between biopsy and TURP was 7.3 days. Twenty-six patients received biopsy and TURP in one session. The mean prostate volume was 49.45 cm3 and the mean resected prostate volume was 25.8 cm3. The mean prebiopsy PSA and PSAD were 51.77 ng/mL and 1.82 ng/mL/g, respectively.
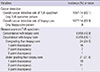
Overall, CaP was detected in 114 patients (57.6%). Seven cancers (6.1%) were detected only with TURP, ninety-eight (86%) with TURP and biopsy, and nine (7.9%) with biopsy alone. The positive predictive value for the TUR specimens and biopsy cores were 92.1% (105/114) and 93.9% (107/114), respectively. The Gleason score of the TUR specimen was concordant with the biopsy core in 43 (43.9%) patients, and 56.1% were discordant with the biopsy core. The Gleason score of the TUR specimen differed by 1 digit in 35 cases, 2 digits in 18 cases, and 3 digits in 2 cases compared with that of the biopsy core (Table 2).
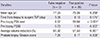
The diagnostic accuracy of the TUR specimens was significantly higher in patients with a higher prebiopsy PSA, PSAD and Gleason scores from the biopsy core (each P<0.05). However, there were no significant differences in the cancer detection rates according to resected weight percentages, ages and time intervals from biopsy to TURP (Table 3).
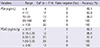
There were five false-negative results from TUR-derived tissue in patients with PSA values between 4.0 and 10.0 ng/mL (the diagnostic gray zone). In patients with a PSA level and a PSAD greater than 15.4 ng/mL and 0.69 ng/mL/g, 100% of the cancers were detected in the TUR specimen (Table 4). The area under the receiver operating characteristic curve for cancer detection in the TUR specimen was 0.951 for PSA (95% confidence interval 0.893 to 1.000, P<0.001) and 0.906 for PSAD (95% confidence interval 0.814 to 0.998, P=0.001). The cut-off value which gave optimal sensitivity and specificity for cancer detection in TUR-derived specimens was 9.5 ng/mL (sensitivity and specificity, 90.8% and 83.3%, respectively) and 0.373 ng/mL/g (sensitivity 81.5% and specificity 93.3%, respectively) (Fig. 1).
In the current study, histologic analysis of the resected specimens after TURP showed a diagnostic accuracy of 92.1% in terms of cancer detection and a 57.1% concordance with the Gleason score. The diagnostic accuracy of the TUR-derived specimens was associated with the prebiopsy PSA, the PSAD, and the Gleason scores of the biopsy cores.
The diagnostic role of TUR-derived tissue in cancer detection remains controversial. Bach et al. (13) reported that only 54% of the CaP cases were detected by TURP and there were no statistical differences in the cancer detection rates according to PSA and biopsy Gleason scores. They concluded that the worth of the obtained tissue sample during TURP seems questionable. The diagnostic accuracy in terms of cancer detection of the TUR-derived tissue in our study was much higher than that shown in the previous study. This result might be due to the fact that a large percentage of the participants in our study population had a very high PSA level and an advanced disease status. In the study of Bach et al., the median PSA level was 8.64 ng/mL and most of the patients (77/84, 92%) had an organ-confined disease (below pT2c), but our study population showed very high PSA levels (mean 51.77 ng/mL). The other possibility is that the study design and inclusion criteria could explain the discrepant results. While the Bach et al. enrolled patients with biopsy-proven CaP who underwent TURP before primary high-intensity focused ultrasound (HIFU) therapy, our study population consisted of patients with CaP who were not suitable for local treatment with a curative intent.
However, there is favorable evidence of the diagnostic role of TURP. In the study by Niesel et al. (14), 132 patients with suspected cancer underwent additional systematic biopsies of the peripheral zone prior to TURP. Biopsy was unable to detect cancer in 11 (40.8%) of 27 prostate cancer cases. In addition, several investigators have reported that TURP was valuable in diagnosing prostate carcinoma in the case of multiple negative biopsies and with a persistently elevated PSA. Kitamura et al. (15) reported that 28% of patients who underwent TURP after negative peripheral zone and transition zone biopsies had cancer in TURP specimens. Zigeuner et al. (8) proposed TURP as a diagnostic tool after a negative biopsy in a patient with voiding symptoms and suspicious DRE results. Though the systemic needle biopsy in the diagnosis of prostate cancer is undoubtedly the choice for diagnosis, the false-negative rate of systemic prostate biopsy is reportedly as high as 35% (16-19). Although 75 to 80% of all CaP originates from the peripheral zone, tumor tissue is also frequently found in the transition zone that is beyond the reach of a biopsy needle in the case of large-volume prostate needle biopsies (20). Whereas TURP procedures do not reach the lateral prostatic tissue, biopsies of the far lateral zone could be combined with TURP to obtain a complete sampling and improve the cancer detection rate (21, 22). Cho et al. (23) reported the safety and efficacy of combined transrectal ultrasound-guided prostate needle biopsy and transurethral resection of the prostate. Puppo et al. (22) also concluded that TURP combined with a set of transrectal needle biopsies of the lateral portion of the gland is a safe procedure with high diagnostic capabilities after repeated negative biopsies in patients with persistently increasing PSA levels. Although the combination of TURP and biopsy is an efficient treatment that can provide reliable cancer detection rates, these continue to require more time under anesthesia and increased hospital costs. Therefore, a combined strategy might be preferred in patients who are susceptible to curative treatment.
Histological grading of prostate cancer is well recognized as an important prognostic factor (24). The Gleason score of the TUR-specimen was discrepant with the biopsy core in 56.1% of the cases and displayed a tendency to under-grade. Therefore, clinicians should consider these discrepancies when discussing treatment options, particularly among patients who are eligible for active surveillance or watchful waiting.
A possible limitation of the present study is that we did not evaluate the surgical outcomes and procedure-related complications. Second, as mentioned above, this study was not a population-based study. Our study population showed very high PSA values, which resulted in a high cancer-detection rate for the TUR-derived tissue.
Our results suggest the omission of prostatic biopsy in obstructive-voiding symptomatic patients with PSA and PSAD levels >15.4 and 0.69 ng/mL/gm, respectively. TUR-derived specimens can yield sufficiently reliable diagnostic accuracy. Further prospective trials are important in establishing reliable cut-off values for PSA levels and/or PSAD, which can negate the need for prostatic biopsy. To apply our results in a clinical setting, the false negative risk should be considered at the time of informed consent and long-term clinicobiological surveillance seems mandatory with a careful observation of PSA levels.
In conclusion, the clinical relevance of the TURP is marked by the fact that it can result in a clear symptomatic benefit and yield high diagnostic accuracy relative to cancer detection and the prediction of histologic grading. Nonetheless, the 7.9% false-negative risk should be considered at the time of informed consent.
Figures and Tables
Fig. 1
Receiver operating characteristic (ROC) curve generated for calculated the cancer detection in TUR specimen in related to PSA and PSAD. AUC, area under the curve; PSA, Prostate specific antigen; PSAD, Prostate specific antigen density.

ACKNOWLEDGMENT
The authors wish to thank Ms. Eun-Ju Shim from the National Biobank of Korea at Chungbuk National University Hospital for the sample preparations and her excellent technical assistance.
References
1. Aus G, Abbou CC, Bolla M, Heidenreich A, Schmid HP, van Poppel H, Wolff J, Zattoni F. European Association of Urology. EAU guidelines on prostate cancer. Eur Urol. 2005; 48:546–551.
2. Berger AP, Gozzi C, Steiner H, Frauscher F, Varkarakis J, Rogatsch H, Bartsch G, Horninger W. Complication rate of transrectal ultrasound guided prostate biopsy: a comparison among 3 protocols with 6, 10 and 15 cores. J Urol. 2004; 171:1478–1480.
3. Nam RK, Saskin R, Lee Y, Liu Y, Law C, Klotz LH, Loblaw DA, Trachtenberg J, Stanimirovic A, Simor AE, et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol. 2010; 183:963–968.
4. Raaijmakers R, Kirkels WJ, Roobol MJ, Wildhagen MF, Schrder FH. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002; 60:826–830.
5. Wong YN, Mitra N, Hudes G, Localio R, Schwartz JS, Wan F, Montagnet C, Armstrong K. Survival associated with treatment vs observation of localized prostate cancer in elderly men. JAMA. 2006; 296:2683–2693.
6. Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid HP, van der Kwast T, Wiegel T, et al. EAU guidelines on prostate cancer: part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol. 2011; 59:61–71.
7. Crain DS, Amling CL, Kane CJ. Palliative transurethral prostate resection for bladder outlet obstruction in patients with locally advanced prostate cancer. J Urol. 2004; 171:668–671.
8. Zigeuner R, Schips L, Lipsky K, Auprich M, Salfellner M, Rehak P, Pummer K, Hubmer G. Detection of prostate cancer by TURP or open surgery in patients with previously negative transrectal prostate biopsies. Urology. 2003; 62:883–887.
9. Lin CC, Huang WJ, Wu LJ, Chang YH, Lin AT, Chen KK. Diagnosis of prostate cancer: repeated transrectal prostate biopsy or transurethral resection. J Chin Med Assoc. 2008; 71:448–454.
10. Merrill RM, Wiggins CL. Incidental detection of population-based prostate cancer incidence rates through transurethral resection of the prostate. Urol Oncol. 2002; 7:213–219.
11. Philip J, Dutta Roy S, Scally J, Foster CS, Javlé P. Importance of TURP in diagnosing prostate cancer in men with multiple negative biopsies. Prostate. 2005; 64:200–202.
12. Epstein JI, Allsbrook WC Jr, Amin MB, Egevad LL. ISUP Grading Committee. The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol. 2005; 29:1228–1242.
13. Bach T, Geavlete B, Pfeiffer D, Wendt-Nordahl G, Michel MS, Gross AJ. TURP in patients with biopsy-proven prostate cancer: sensitivity for cancer detection. Urology. 2009; 73:100–104.
14. Niesel T, Breul J, Hartung R. Diagnostic value of additional systematic prostate biopsies in patients undergoing transurethral resection of the prostate. Urology. 1997; 49:869–873.
15. Kitamura H, Masumori N, Tanuma Y, Yanase M, Itoh N, Takahashi A, Tsukamoto T, Adachi H, Hotta H. Does transurethral resection of the prostate facilitate detection of clinically significant prostate cancer that is missed with systematic sextant and transition zone biopsies? Int J Urol. 2002; 9:95–99.
16. Wolters T, van der Kwast TH, Vissers CJ, Bangma CH, Roobol M, Schröder FH, van Leenders GJ. False-negative prostate needle biopsies: frequency, histopathologic features, and follow-up. Am J Surg Pathol. 2010; 34:35–43.
17. Ploussard G, Nicolaiew N, Marchand C, Terry S, Allory Y, Vacherot F, Abbou CC, Salomon L, de la Taille A. Risk of repeat biopsy and prostate cancer detection after an initial extended negative biopsy: longitudinal follow-up from a prospective trial. BJU Int. 2013; 111:988–996.
18. Durkan GC, Sheikh N, Johnson P, Hildreth AJ, Greene DR. Improving prostate cancer detection with an extended-core transrectal ultrasonography-guided prostate biopsy protocol. BJU Int. 2002; 89:33–39.
19. Lee SJ, Hwang I, Hwang EC, Jung SI, Kang TW, Kwon DD, Park K. Are more low-risk prostate cancers detected by repeated biopsy? a retrospective pilot study. Korean J Urol. 2013; 54:364–368.
20. O'dowd GJ, Miller MC, Orozco R, Veltri RW. Analysis of repeated biopsy results within 1 year after a noncancer diagnosis. Urology. 2000; 55:553–559.
21. Ploussard G, Dubosq F, Boublil V, Allory Y, de la Taille A, Vordos D, Hoznek A, Abbou CC, Salomon L. Extensive biopsies and transurethral prostate resection in men with previous negative biopsies and high or increasing prostate specific antigen. J Urol. 2009; 182:1342–1349.
22. Puppo P, Introini C, Calvi P, Naselli A. Role of transurethral resection of the prostate and biopsy of the peripheral zone in the same session after repeated negative biopsies in the diagnosis of prostate cancer. Eur Urol. 2006; 49:873–878.
23. Cho JM, Lee SW, Kang JY, Yoo TK. Safety and efficacy of combined transrectal ultrasound-guided prostate needle biopsy and transurethral resection of the prostate. Korean J Urol. 2010; 51:101–105.
24. Cookson MS, Fleshner NE, Soloway SM, Fair WR. Correlation between Gleason score of needle biopsy and radical prostatectomy specimen: accuracy and clinical implications. J Urol. 1997; 157:559–562.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download