Abstract
Currently, infliximab is given for disease control for active rheumatoid arthritis (RA) patients despite methotrexate treatment. However, the efficacy and safety of infliximab in Korean patients has not been assessed appropriately. Therefore, we performed placebo-controlled, double-blind, randomized study and extension study. One-hundred forty-three patients with active RA were randomized to receive placebo or infliximab 3 mg/kg intravenously at week 0, 2, 6, 14, and 22 with methotrexate maintenance. Primary endpoint was American College of Rheumatology 20% improvement criteria (ACR20) at 30 week. After the clinical trial, patients on placebo (Group 1) and patients on infliximab who showed ACR20 response (Group 2) were treated with infliximab through another 84 week for evaluation of safety. During clinical trial, patients in infliximab group showed higher ACR20 at week 30 than patients in placebo group (50.1% vs 30.6%, P=0.014). A total of 92 patients participated in the extension study. The maintenance rate of infliximab was 62.0% at 84 weeks of extension study. The overall rate of adverse events was not different between Group 1 and Group 2. In Korean patients with active RA despite methotrexate treatment, infliximab in combination with methotrexate is effective and the long-term treatment with infliximab is well tolerated. (ClinicalTrials.gov No. NCT00202852, NCT00732875)
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by synovitis and other system involvement. Currently, disease modifying antirheumatic drugs (DMARDs) are given for disease control. However, DMARDs are not satisfactory because they can take several months to produce the effects and have dose limiting toxicity. Among DMARDs, methotrexate (MTX) showed faster action and excellent efficacy in long-term treatment, and consequently has been widely used by many rheumatologists. However, despite high-dose methotrrexate, many patients do not reach remission in spite of partial symptomatic relief (1).
Tumor necrosis factor-α (TNFα) is the main cytokine of regulating other pro-inflammatory cytokines related to RA (2, 3). Infliximab, chimeric TNFα monoclonal antibody, has high affinity and specificity to TNFα and neutralized its biologic activity, thus, it had good therapeutic effect based on many clinical trials (4, 5). The anti-tumor necrosis factor trial in rheumatoid arthritis with concomitant therapy (ATTRACT) study showed that the repeated administration of infliximab was more effective in decreasing RA signs and symptoms, improving physical function, and preventing structural damage and the worsening of quality of life than MTX monotherapy in established RA patients (6, 7). However, well-designed clinical trial of infliximab in RA patients was not performed in Asia although there are retrospective study and study on small number of patients (8-10).
This clinical trial and subsequent extension study was conducted to investigate whether this drug decreased the symptoms and signs of RA at 30 weeks in Korean patients with active RA compared to placebo and whether the safety and efficacy results of the drug were consistent with the results of previous trials.
Patients were eligible if they had been diagnosed with RA according to the 1987 American College of Rheumatology (ACR) criteria (11) and had evidence of active disease despite treatment with methotrexate (six or more swollen and tender joints plus two of: morning stiffness greater than or equal to 45 min, erythrocyte sedimentation rate (ESR) greater than 28 mm/h, C-reactive protein (CRP) greater than 2 mg/dL. The patients were classified into a functional class using ACR criteria (12). Patients must also have been receiving oral or parenteral methotrexate for at least 3 months. The methotrexate dose must have been stable at 12.5 mg/week or more for at least 4 weeks before screening. Patients using oral corticosteroids (10 mg/kg or less prednisone equivalent) or non-steroidal anti-inflammatory drugs (NSAIDs) must have been on a stable dose for at least 4 weeks before screening. Patients using leflunomide at least 6 months before drug administration had to have wash-out period (cholestyramine 8 g three times a day for 11 days). Other DMARDs was stopped 4 weeks before administration of study drugs. Patients continued their baseline dose of methotrexate or corticosteroids during the trial. All patients were checked for latent tuberculosis (tuberculin skin test and chest radiograph) and if the test was positive, then the patients were treated with isoniazid for at least 3 weeks before enrollment.
Patients were screened for inclusion criteria within 14 days before randomization. Before the first infusion, patients were assessed for all criteria to provide baseline measurements. Patients were randomly assigned to placebo or treatment regimens of infliximab (3 mg/kg, Remicade, Schering-Plough, Kenilworth, New Jersey, USA). All patients were given intravenous infusions at weeks 0, 2, and 6 and every 8 weeks thereafter through 22 weeks. The investigators, independent joint assessors and patients were blinded to the treatment assignments.
After the completion of 30-week visits and unblinding in all the patients who participated in the clinical trial, infliximab was additionally given to patients in the placebo group (placebo → infliximab, Group 1) and patients in the infliximab group who showed clinical responses at 30 weeks (infliximab → infliximab, Group 2). For the patients Group 1, infliximab 3 mg/kg was given in an open-label manner at 0, 2, and 6 weeks and every 8 weeks. In addition, infliximab treatment continued in patients who showed at least ACR20 clinical response at 30 weeks among patients of Group 2 who received infliximab. The patients received infliximab concomitantly with methotrexate maintenance therapy during extension study for 84 weeks.
Clinical efficacy was assessed at baseline, at every visit for infusion (before infusion of study drugs) and at 30 week. All the patients were assessed at 30 weeks regardless of study drug response or drop-out for safety evaluation. The primary endpoint was prospectively defined as 20% improvement, according to the ACR20 (13) at the week 30 visit. Secondary measurements of response to therapy included documentation of ACR50, ACR70 and ACR90 response, reduction in individual measurements of disease activity (swollen or tender joint count, ESR, CRP, morning stiffness, Korean Health Assessment Questionnaire [KHAQ]), and Short Form-36 (SF-36).
Adverse events (AEs) were assessed for the safety and tolerance evaluation during clinical trial. Complete blood count and chemistry were performed at baseline and week 2, 6 and every 8 weeks thereafter. Urinalysis was performed at screening and at week 30. Anti-nuclear antibody (ANA) and anti-dsDNA antibody was measured at 0 week and 30 week. In extension period, AEs were evaluated. Adverse event (AE) is defined as any untoward or undesirable medical incident or symptom experienced by patients given the investigational drugs regardless of the causal relationship with the use of the drug. All the AEs were summarized according to World Health Organization Adverse Reaction Terminology (WHOART) system organ class and preferred terms (14).
The number of subjects for this study is calculated with the significance level of 0.05 and statistical power of >80%, in order to verify the hypothesis that the ACR20 difference between the infliximab group and the placebo group would stand at 25%. Consequently, the hypothesis is anticipated to be proven if each group can have approximately 61 patients allocated. However, this clinical study was proceeded with 70 patients in each group (a total of 140 patients), in consideration of uncertainties in subject calculation and drop-out.
The primary outcome variable (ACR20) analysis was performed on an intention-to-treat basis. Secondary outcome variables such as ACR50, ACR70, and ACR90, the number of swollen or tender joint, KHAQ, ESR, CRP and improvement in the quality of life (SF-36) at 30 weeks were analyzed.
The safety analysis was conducted on the number of AEs that occurred per time unit in the phase III clinical study and the extension clinical study. The timeframe was divided into the phase III clinical study, up to 30 weeks (extension clinical study) and 30-60 weeks (extension clinical study) periods, and the numbers of AEs in each period were compared with one another.
Chi-square test was used to compare the response rate of each treatment group. Serious AEs (SAEs) were compared using the Fisher's exact test. The t-test or weighted t-test was used to analyze continuous variables. All statistical analyses are two-tailed.
This study protocol was reviewed and approved by institutional review boards or ethics committees at all sites (IRB No. 0504-147-022), and performed according to the Declaration of Helsinki. All patients were enrolled after obtaining informed consent at 6 centers in Korea. This trial was registered at www.clinicaltrial.gov as NCT00202852 (phase 3 clinical trial) and NCT00732875 (extension study).
From June 2005 through May 2006, a total of 143 patients was enrolled in the clinical trial in the 6 medical centers. Seventy-one patients were randomized to infliximab group and 72 patients to placebo group. Among them, 136 patients completed clinical trials through 30 weeks. A total of 143 patients were included in the efficacy assessment and 138 patients were in the safety assessment (Fig. 1).
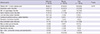
Gender ratio and age were comparable in both groups, while disease duration was longer in the placebo group than in the infliximab group (P=0.033). There were no differences in baseline clinical characteristics between two treatment groups (Table 1). During extension period, 86 (93.5%) of the patients enrolled in this trial were females and mean age was 49.0±11.1 yr (Table 2). Thirty-five (38.0%) of 92 subjects discontinued the treatment in the middle of the extension study due to the withdrawal of consent in 6 subjects (6.5%), lack of efficacy in 13 subjects (14.1%) and AEs in 16 patients (17.4%). Among subjects who discontinued the treatment due to the lack of efficacy, 2 subjects terminated the trial due to serious adverse events (SAEs) caused by the worsening of RA symptoms, judged as a lack of efficacy by investigators.
At 30 week visit, the proportion of ACR20 response rate was significantly higher in infliximab group than placebo group (infliximab group 50.7% vs placebo group 30.6%, P=0.014). According to efficacy assessment at each time point, significant response appeared first in infliximab group from 2 week visit (ACR20 response rate, infliximab group, 25.4% vs placebo group, 5.6%) and this difference was persistent throughout the study period.
The proportion of ACR50, ACR70, and ACR90 was increased from 2 week visit in infliximab group compared with placebo group, which was increased gradually afterwards. ACR50 was 4.2% in infliximab treatment group at 2 week, 22.5% at 14 week visit, and reached 33.8% at 30 week visit. The number of swollen joint or tender joint at 30 weeks was decreased from the baseline value significantly in infliximab group compared with placebo group (swollen joint: -51.9% in infliximab group vs -25.7% in placebo group, P=0.002; tender joint: -44.2% in infliximab group vs -15.7 in placebo group, P=0.005). The difference in KHAQ score between infliximab group and placebo group was also significant at 30 week (-35.5 vs -10.8, P=0.009). The life quality measured by SF-36 showed improvement in physical component (mean physical component score, infliximab group, 6.1 vs in placebo group, 1.2, P<0.001). CRP decreased 77.6% in infliximab group and 11.5% in placebo group at 30 week. ESR was decreased significantly in infliximab group at 30 week visit compared to baseline value (34.0% in infliximab group and 20.5% in placebo group).
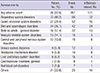
A total of 143 patients participated in this clinical trial and among them, 138 patients who received study medication at least once became the group for safety analysis. The number of patients who experienced AE was 46 (66.7%) in infliximab group and 42 (60.9%) in placebo group (Table 3).
The commonly involved systems were respiratory, skin and appendage, hepatobiliary, resistance mechanism, and body as whole-general disorder in order. AE which could be attributed to by study medication by investigator occurred in 27 (39.1%) in infliximab group and 10 (14.5%) in placebo group (P=0.001). SAEs were reported from 6 patients (8.7%) in infliximab group and 10 (14.5%) in placebo group. The relationship with study medication was not excluded in 5 (7.3%) in infliximab group and 3 (4.4%) in placebo group. Among them, 2 anaphylaxes and 1 (1.4%) fever in infliximab group and 2 (2.9%) fever in placebo group were included.
Infection was reported in 25 (36.2%) in infliximab group and 19 (27.5%) in placebo group (P=0.273), but there was no tuberculosis case. Infusion reaction occurred more frequently in infliximab group than placebo group (7 [10.1%] vs 2 [2.9%]). The incidence of infusion reaction was not increased by increasing number of infusion. Significantly increased lymphocyte count was found in infliximab group compared to placebo group (infliximab group 16 [23.2%] vs placebo group 1 [1.4%]) and significantly increased AST/ALT was found in infliximab group (infliximab group 7 [10.1%] vs placebo group 0 [0%]). Among ANA-negative (<1:320) patients (infliximab group 64, placebo group 63) before treatment, 8 (12.5%) in infliximab group and 3 (4.8%) in placebo group became ANA-positive (≥1:320) at 30 week (P=0.121). Anti-dsDNA antibody became positive (>25 IU/mL FARR assay) in 3 (4.4%) patients treated with infliximab and none with placebo at 30 week. Stomach cancer was reported in 1 patient of placebo group.
Safety evaluation was made in subjects given infliximab additionally at least once or more after the completion of 30-week visits. Patients received drugs for 61±28.9 weeks on average during the extension period. Eighty-six patients (93.5%) continued the treatment until 12 weeks, 74 (80.4%) until 24 weeks, 64 (69.6%) until 48 weeks and 57 (62.0%) until 84 weeks.
During the extension study periods, 287 adverse events were reported in 76 subjects (82.6%) and 24 SAEs in 12 subjects (13.0%). Eighteen subjects (19.6%) discontinued the treatment due to AEs; and 70 infection-related diseases were reported in 41 subjects (44.6%). Among all the reported AEs, AEs that occurred at ≥5% were summarized according to WHOART systemic organ class and preferred term (Table 4). In total, 24 SAEs were reported over 13 cases and 4 of them were related with infection. The causal relationship with infliximab was not likely in 17 events.
The treatment was discontinued in 18 subjects (19.6%) due to AE. Two of them discontinued the treatment due to the lack of efficacy. The most common reason of the discontinuation was respiratory AEs observed in 6 subjects, followed by skin and appendage AEs in 5, systemic reactions in 4, gastrointestinal AEs in 4, neurologic AEs in 3, injection-site disorder and musculoskeletal disorders, vascular (non-cardiac) disorders in 2 each and metabolism and nutrition disorders, red blood cell disorder (anemia), resistance mechanism disorders (fever) and urinary AEs (pyelonephritis) in one each.
A total of 70 infection cases were reported in a total of 41 subjects (44.6%). Tuberculosis was not reported during this extension study. System organ class which was most frequently classified into infection was respiratory AEs in 27 subjects (29.4%), followed by urinary AEs (n=7, 7.6%), resistance mechanism AEs (n=7, 7.6%), skin and appendage AEs (n=4, 4.4%), systemic reactions (n=2, 2.2%), gastrointestinal AEs (n=2, 2.2%), musculoskeletal AE, reproductive AE and vision-related AE (n=1, 1.1%, each). No cancer was reported in this study period.
Person time incidence rate of all patients was calculated for safety analysis. Among the patient who received placebo in the clinical trial, person time incidence rate was 0.033 (42 patients/1,262.4 weeks) and the number of AEs per week was 0.078 (98 AEs/1,262.4 weeks). Among the patients who received infliximab in the clinical trial or extension study, person time incidence rate was 0.016 (105 patients/6,685.9 weeks) and the number of AE per week was 0.061 (409 AEs/6,685.9 weeks).
The average number of AEs in the infliximab group (Group 2) was 1.6 during the phase III clinical trial, 1.2 during the extension study up to 30 weeks, and 1.5 during the extension study from 30 weeks to 60 weeks. The numbers of AEs during each period did not post a statistically significant difference (P=0.531, by repeated measures ANOVA). The average number of AEs in placebo group (Group 1) amounted to 1.5 during the phase III clinical study, 1.6 during the extension study up to 30 weeks, and 0.9 during the extension study from 30 weeks to 60 weeks, which also did not post a statistically significant difference (P=0.220, by repeated measures ANOVA). The results are summarized in Table 5.
In this placebo-controlled, double-blind, randomized phase III clinical trial and subsequent extention study on patients with active rheumatoid arthritis despite methotrexate treatment, primary outcome (ACR20) at 30 week was significantly improved compared with placebo group (P=0.014). This efficacy was consistent regardless of demographic characteristics, baseline disease characteristics or combined drugs, showing higher efficacy in the infliximab group, appearing at week 2 visit and persistent through week 30. Moreover, the safety was shown in clinical trial and extension study, which was similar to other trials.
Accordingly, patients with active RA despite methotrexate treatment could be beneficial by infusion of infliximab 3 mg/kg at 0, 2, 6 week and every 8 weeks thereafter. First, only 2 weeks after the infusion of study medication, the sign and symptom of active disease was reduced and this effect was persistent through 30-week-trial period. Second, through 30-week follow-up period, patients who tolerated infliximab treatment were generally safe. Therefore, these results showed that patients with active RA despite methotrexate treatment could be effectively managed by infliximab to improve disease symptom and signs.
The results of this trial were very similar to the findings in the ATTRACT trial (6, 7). Infliximab therapy was associated with a greater number of patients achieving ACR20, ACR50 and ACR70 responses. Improvements in joint swelling/tenderness, HAQ, physical component score. The safety profile of infliximab group was similar to placebo group; no difference in incidence of AE/SAE or infection rates.
The efficacy of infliximab was rarely studied prospectively in Asian population. Japaneses retrospective study showed the efficacy of infliximab, which showed good or moderate overall response using EULAR criteria in 84.5% of patients after 22 weeks and 78.7% at 54 week (8, 9). Small-scale, short-term Chinese study showed 83.3% ACR20 rate after 14 week treatment in 18 patients (10).
During the extension period, infliximab was generally well tolerated and the previous treatment of infliximab did not affect the incidence of AE in the extension period. There was no statistically significant difference in the comparison of the number of AEs among phase III vs. extension trial ≤30 weeks vs. 30-60 weeks. The long-term treatment with infliximab in active RA patients in spite of MTX treatment was well tolerated. In addition, the profiles of AEs were not very different from the previous reports (15).
In one report, the retention on infliximab was 61.6% after 4 yr treatment and the main reason for discontinuation were lack of efficacy (13.6%) and safety issue (16.9%) (16). Retrospective Japanese study demonstrated 75.6% retention rate on infliximab at 54 week, and the 9.3% and 8.1% discontinued the therapy due to adverse events and inefficiency, respectively (8, 9). Comparing with these data, the retention rate in this extension study was similar, which was 67.4% at 60 week and 62.0% at 84 week, although each data can have the different enrollment criteria. Moreover, the number of AEs in infliximab-treated period in this study showed apparent low incidence rate compared with placebo-treated period. With 12 yr of clinical experience and the large scale data of national disease registries, the safety profile of TNF inhibitors was well characterized (16). SAEs with infliximab included infection, infusion reaction/allergy, malignancy, and autoantibody formation (15). Among them, there was no malignancy in this trial and the generation of antibodies to infliximab was not correlated to AE in the current study. There were 3 infusion reactions including 2 anaphylaxes.
Whether infection rate during the treatment with infliximab is increasing or not is not clear. Some registry data demonstrated similar rate of infection between the patients treated with anti-TNF agents and the patients treated with conventional DMARD (17) while other did not (18). In a prospective, observational study from the British Society for Rheumatology Biologics Register, the incidence rate ratio of serious infection rates, adjusted for baseline risk, for the TNF-inhibitor cohort compared with the DMARD cohort was 1.03 (95% confidence interval, 0.68 to 1.57), suggesting similar risk levels between the two treatment groups (17). However, a prospective cohort study of the German RA registry RABBIT showed that 21% of patients who were treated with biologic agent experienced a serious infection compared with 6% of patients who were treated with conventional DMARDs (18). There is few registry data comparing infection rate between infliximab and conventional DMARDs. In the situation of clinical trial, infection rate was similar between infliximab group and placebo group (19). This study also showed infection rate in infliximab group was comparable with placebo, and the extension study did not show any increase of infection during study period. Therefore, infliximab treatment was safe in Korean RA patient like other population.
The long-term treatment with infliximab in Korean patients with active RA in spite of MTX treatment is well tolerated. In addition, adverse events are similar to the previously reported studies.
Figures and Tables
Table 3
Number of patients with any adverse event by WHOART preferred term in clinical trial (if an adverse event occurred in at least 5% of all infliximab-treated patients)
References
1. Firestein GS. Evolving concepts of rheumatoid arthritis. Nature. 2003; 423:356–361.
2. Feldmann M, Brennan FM, Chantry D, Haworth C, Turner M, Abney E, Buchan G, Barrett K, Barkley D, Chu A. Cytokine production in the rheumatoid joint: implications for treatment. Ann Rheum Dis. 1990; 49:480–486.
3. Cope AP, Aderka D, Doherty M, Engelmann H, Gibbons D, Jones AC, Brennan FM, Maini RN, Wallach D, Feldmann M. Increased levels of soluble tumor necrosis factor receptors in the sera and synovial fluid of patients with rheumatic diseases. Arthritis Rheum. 1992; 35:1160–1169.
4. Knight DM, Trinh H, Le J, Siegel S, Shealy D, McDonough M, Scallon B, Moore MA, Vilcek J, Daddona P, et al. Construction and initial characterization of a mouse-human chimeric anti-TNF antibody. Mol Immunol. 1993; 30:1443–1453.
5. Elliott MJ, Maini RN, Feldmann M, Kalden JR, Antoni C, Smolen JS, Leeb B, Breedveld FC, Macfarlane JD, Bijl H, et al. Randomised double-blind comparison of chimeric monoclonal antibody to tumour necrosis factor alpha (cA2) versus placebo in rheumatoid arthritis. Lancet. 1994; 344:1105–1110.
6. Maini R, St Clair EW, Breedveld F, Furst D, Kalden J, Weisman M, Smolen J, Emery P, Harriman G, Feldmann M, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial: ATTRACT Study Group. Lancet. 1999; 354:1932–1939.
7. Lipsky PE, van der Heijde DM, St Clair EW, Furst DE, Breedveld FC, Kalden JR, Smolen JS, Weisman M, Emery P, Feldmann M, et al. Infliximab and methotrexate in the treatment of rheumatoid arthritis: Anti-Tumor Necrosis Factor Trial in Rheumatoid Arthritis with Concomitant Therapy Study Group. N Engl J Med. 2000; 343:1594–1602.
8. Yamanaka H, Tanaka Y, Sekiguchi N, Inoue E, Saito K, Kameda H, Iikuni N, Nawata M, Amano K, Shinozaki M, et al. Retrospective clinical study on the notable efficacy and related factors of infliximab therapy in a rheumatoid arthritis management group in Japan (RECONFIRM). Mod Rheumatol. 2007; 17:28–32.
9. Tanaka Y, Takeuchi T, Inoue E, Saito K, Sekiguchi N, Sato E, Nawata M, Kameda H, Iwata S, Amano K, et al. Retrospective clinical study on the notable efficacy and related factors of infliximab therapy in a rheumatoid arthritis management group in Japan: one-year clinical outcomes (RECONFIRM-2). Mod Rheumatol. 2008; 18:146–152.
10. Gao GH, Li J, Xie HW, Lü Z. Therapeutic effect of infliximab on moderate and severe active rheumatoid arthritis. Nan Fang Yi Ke Da Xue Xue Bao. 2010; 30:724–726.
11. Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988; 31:315–324.
12. Hochberg MC, Chang RW, Dwosh I, Lindsey S, Pincus T, Wolfe F. The American College of Rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum. 1992; 35:498–502.
13. Paulus HE, Egger MJ, Ward JR, Williams HJ. Analysis of improvement in individual rheumatoid arthritis patients treated with disease-modifying antirheumatic drugs, based on the findings in patients treated with placebo: the Cooperative Systematic Studies of Rheumatic Diseases Group. Arthritis Rheum. 1990; 33:477–484.
14. Uppsala Monitoring Centre. The WHO adverse reaction terminology - WHO-ART. accessed on 3 January 2012. Available at http://www.umc-products.com/graphics/3149.pdf.
15. Smolen JS, Emery P. Infliximab: 12 years of experience. Arthritis Res Ther. 2011; 13:S2.
16. Voulgari PV, Alamanos Y, Nikas SN, Bougias DV, Temekonidis TI, Drosos AA. Infliximab therapy in established rheumatoid arthritis: an observational study. Am J Med. 2005; 118:515–520.
17. Dixon WG, Watson K, Lunt M, Hyrich KL, Silman AJ, Symmons DP. British Society for Rheumatology Biologics Register. Rates of serious infection, including site-specific and bacterial intracellular infection, in rheumatoid arthritis patients receiving anti-tumor necrosis factor therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2006; 54:2368–2376.
18. Listing J, Strangfeld A, Kary S, Rau R, von Hinueber U, Stoyanova-Scholz M, Gromnica-Ihle E, Antoni C, Herzer P, Kekow J, et al. Infections in patients with rheumatoid arthritis treated with biologic agents. Arthritis Rheum. 2005; 52:3403–3412.
19. Westhovens R, Yocum D, Han J, Berman A, Strusberg I, Geusens P, Rahman MU. START Study Group. The safety of infliximab, combined with background treatments, among patients with rheumatoid arthritis and various comorbidities: a large, randomized, placebo-controlled trial. Arthritis Rheum. 2006; 54:1075–1086.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download