Abstract
Vascular injuries in lumbar disc surgery are serious complications which may be overlooked due to a broad range of clinical manifestations. It is important to be aware of the perioperative implications of this rare occurrence to lower mortality risk. A 20-yr-old man with a right L4-5 lumbar disc protrusion was operated on routinely under a surgical microscope. A bloody surgical field was noted temporarily during a discectomy along with a decreased blood pressure. After fluid resuscitation with an ephedrine injection, the bleeding soon stopped spontaneously and his vital signs were stabilized. Fifty hours after the operation, the patient showed signs of hypovolemic hypotension with abdominal distension. The right femoral artery pulsation was absent on palpation. An enhanced CT angiography revealed a retroperitoneal hematoma and obstruction of the left common iliac artery. An urgent laparotomy was done to repair the injured vessel by excision and interposition of a graft. The patient had an uneventful recovery.The subacute course of deterioration might have been due to intermittent blood leakage from the lacerated common iliac artery, which was sealed spontaneously. It is very important to pay close attention to post-surgical clinical manifestations to avoid a potentially fatal outcome in lumbar disc surgery.
Lumbar disc surgery is a common and routine procedure. The incidence of vascular injury is 0.01%-0.05% and has not been reduced over the past 50 yr (1). The most common injury during lumbar discectomy is seen in the common iliac artery, which is located immediately anterior to the L4-5 lumbar disc space (2). Types of vascular injury include laceration, arteriovenous fistula (AVF), and pseudoaneurysm (3). Laceration usually becomes symptomatic and fatal intraoperatively or in the early postoperative period, while AVF and pseudoaneurysm are usually diagnosed later. It is very rare that laceration of the common iliac artery takes a subacute course. Here we discuss the vascular injury a subacute course of vascular injuries secondary to lumbar discectomy including pathophysiology, diagnosis, and management.
A 20-yr-old man, 173 cm in height and 58 kg in weight, underwent a microdiscectomy for a symptomatic right-sided disc herniation at the intervertebral space, confirmed by magnetic resonance imaging in 2002. Routine laboratory studies were unremarkable with a hemoglobin (Hb) level of 14.1 g/dL and hematocrit (Hct) of 41.6%. Anesthesia was induced with 250 mg thiopental, 100 mg succinylcholine, 25 mg atracurium and maintained with 1.5% isoflurane in 50% oxygen and 50% nitrous oxide with a fresh gas flow 2 L/min. A routine microdiscectomy was carried out in the prone position on Wilson's frame under general anesthesia. During operation the discectomy the surgeon felt some momentary downward slippage of the pituitary rongeur into the deep intervertebral space. At that moment unexplained profuse bleeding occurred in the disc space. Shortly after this event blood pressure (BP) suddenly decreased from 110/80 mmHg to 80/60 mmHg. It became normalized soon after the injection of ephedrine 10 mg and atropine 0.5 mg and the bleeding stopped spontaneously. In the recovery room, the patient experienced transient hypotension (90/60 mmHg) and tachycardia (95 bpm/min) which again responded well to volume replacement. On the first day after the surgery operation the patient complained of abdominal discomfort and wound pain. BP was 100/70 mmHg, HR 92 bpm/min and body temperature 38.4℃. Hb and Hct was 11 g/dL and 32% respectively. Neurologic examination revealed normal motor tone in his lower extremities. Physically, the abdomen was mildly distended with tenderness in the left lower quadrant of the abdomen on a physical examination. Bowel sounds were decreased. Apparently he was stabilized with volume expansion.
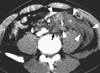
On the second day after the operation he started to complain of increasing abdominal pain in the left quadrant with dizziness and became restless and very pale. At that time BP was 100/60 mmHg, HR 100 b/min and body temperature 38.5℃. Hb was 9.2 g/dL and Hct was 26.9%. Abdominal examination revealed decreased bowel sounds and the left femoral and deep peroneal artery pulsation was absent on palpation. Three hours later, Hb became 6.8 g/dL and Hct was 19.7%. Four units of blood were transfused for stabilization. An urgent Doppler sonogram showed no flow in the common iliac artery suggesting segmental obstruction. Contrast-enhanced CT also revealed a low attenuation perfusion defect in the common iliac artery at the level of L4-5 with a moderate amount of retroperitoneal hematoma (Fig. 1). There was no leakage of contrast but a few small air densities were present around the obstructed artery probably coming out from the perforated anterior spinal ligaments. Angiography of the abdomen demonstrated a complete obstruction of the left common iliac artery, located about 2 cm distal to the aortic bifurcation (Fig. 2). The distal portion of the obstructed artery was filled with contrast material by collateral circulation through the internal and external iliac arteries. Fifty five hours after the L4-5 discectomy, an emergent laparotomy was performed. Anesthesia was induced with 250 mg thiopental, 100 mg succinylcholine, 25 mg atracurium and maintained with 1.5% isoflurane in 50% oxygen and 50% nitrous oxide with a fresh gas flow 2 L/min. During the operation, BP and HR were stable and the surgical field revealed a moderate retroperitoneal hematoma. There was no active bleeding. A small defect was observed in the anterior longitudinal ligament overlying the right side of the L4-5 disc space. The laceration was located at the posterior aspect of the left common iliac artery, made by a partial puncture with a pituitary rongeur. It was packed with thrombus and adhered densely to the punctured anterior longitudinal ligament at the surgical level so that it was spontaneously sealed. The arterial injury was repaired by the excision and interposition of an 8 mm polytetrafluoroethylene graft with the removal of the retroperitoneal hematoma. The postoperative course was uneventful and the patient remains in good condition over 10 yr later.
Major vascular injury during lumbar disc surgery is a rare but life-threatening complication (4-7). While some injuries occur late after surgery, most vascular injuries are seen during or shortly after lumbar disc surgery (6). Anatomically the aortic bifurcation and inferior vena cava confluence occurs at or below the L4 level and is separated from L4-5 disc space only by the anterior spinal ligament (ALL) (8). The left common iliac artery is the most commonly involved because it is located immediately anterior to the L4-5 disc space (8, 9).
Severe arterial injury often causes acute life threatening retroperitoneal hemorrhage. The most common signs and symptoms of arterial lacerations are hypotension, tachycardia, wide pulse pressure and abdominal distention during or shortly after the operation. However, there are rare cases when this type of injury is diagnosed late either in the recovery room or even one day later (10, 11). This case was diagnosed 2 days later after surgery without severe complications.
We couldn't suspect arterial injury during the perioperative period because there was transient hypotension with bleeding in the operation site that recovered quickly by vasopressor and fluid. In general venous bleeding stops spontaneously, does not require surgery and is not life threatening (6). Based on a review of the literature, there are several possible reasons behind the delay in the diagnosis of some of these cases (10, 11). The injury may go undetected by the surgeon, as the blood tends to seep into the retroperitoneal space because of the anatomical position of the injured vessels. At the same time, the anterior spinal ligaments have a self-sealing effect due to its tough and elastic quality, which produces a one-way valve mechanism (4, 6). This leads the blood to flow into the retroperitoneal space rather than the operating space. In a young healthy person a drop in blood pressure may not occur until there is a 30%-40% loss of blood volume. Hemoglobin and hematocrit concentration may not contribute at this early stage of bleeding (7). Abdominal distention and discomfort due to an expanding retroperitoneal hematoma and/or paralytic ileus may not be relied upon, as it was found in less than 20% of cases. However, if they persist, they may indicate a vascular or visceral injury.
The correct diagnosis postoperatively was hindered by misunderstanding the patient's course: episodic mild hypotension and recovery with fluid administration which seemed to be caused by intermittent minor arterial bleedings from a partially ruptured common iliac artery into the retroperitoneum. In retrospect, the sudden drop in blood pressure during the discectomy and postoperatively, should have prompted diagnostic intervention, such as CT and angiography. In addition, physical examination such as palpation of the femoral or deep peroneal artery would also prompt diagnostic procedures. The periphery of the iliac artery distal to segmental obstruction was filled with contrast dye due to collateral circulation through the internal and external iliac artery. That would have explained that why the patient did not complain of any symptoms in his left leg.
Many different suggestions are in the literature concerning the recognition and prevention of this life threatening complication (1). If the surgeon wants to remove only the offending disc material, a pituitary rongeur should not be placed into the disc space any deeper than its jaw. Even if the surgeon wants to remove the disc totally, a pituitary rongeur should not be inserted through the ALL. To prevent this complication, the surgeon should use two hands to manipulate the pituitary rongeur, with one hand fixed on the pituitary rongeur adequately so as not to penetrate the ALL. Additionally the surgeon should keep in mind how far the pituitary rongeur has been inserted into the magnified operation field (3).
We have presented a patient with a left common iliac artery laceration diagnosed two days after an L4-5 microdiscectomy, and treated by the excision and interposition of an 8 mm polytetrafluoroethylene graft on laparotomy. The subacute course of deterioration might be due to intermittent bleeding from a partially ruptured common iliac artery into the retroperitoneum, which thrombosed with and adhered to the ruptured anterior longitudinal ligament. After lumbar disc surgery it is very important to pay close attention to clinical signs such as the absence of femoral and/or deep peroneal artery pulsation on palpation, and to utilize sonography or CT and angiography in the detection of vascular injury in order to avoid a potentially fatal outcome.
Figures and Tables
Fig. 1
Enhanced CT showed non-enhancing thrombotic obstruction of the left common iliac artery iliac artery (arrow) and accompanied large retroperitoneal hematoma (arrowheads). These findings suggested the possibility of iatrogenic arterial laceration with dissecting arterial occlusion and periarterial hematoma formation.
References
1. Inamasu J, Guiot BH. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien). 2006. 148:375–387.
2. Goodkin R, Laska LL. Vascular and visceral injuries associated with lumbar disc surgery: medicolegal implications. Surg Neurol. 1998. 49:358–370. discussion 370-2.
3. Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002. 24:189–195.
4. Yip SL, Woo SB, Kwok TK, Mak KH. Nightmare of lumbar diskectomy: aorta laceration. Spine (Phila Pa 1976). 2011. 36:E1758–E1760.
5. Karwacki Z, Witkowska M, Lasinska-Kowara M, Sloniewski P, Wojciechowski J. iliac artery injury during lumbar microdiscectomy. Anestezjol Intens Ter. 2010. 42:24–26.
6. Dosoglu M, Is M, Pehlivan M, Yildiz KH. Nightmare of lumbar disc surgery: iliac artery injury. Clin Neurol Neurosurg. 2006. 108:174–177.
7. Torun F, Tuna H, Deda H. Abdominal vascular injury during lumbar disc surgery: report of three cases. Ulus Travma Acil Cerrahi Derg. 2007. 13:165–167.
8. Vraney RT, Phillips FM, Wetzel FT, Brustein M. Peridiscal vascular anatomy of the lower lumbar spine: an endoscopic perspective. Spine (Phila Pa 1976). 1999. 24:2183–2187.
9. Bingol H, Cingoz F, Yilmaz AT, Yasar M, Tatar H. Vascular complications related to lumbar disc surgery. J Neurosurg. 2004. 100:249–253.
10. Hui YL, Chung PC, Lau WM, Ng YT, Yu CC. Vascular injury during a lumbar laminectomy. Chang Gung Med J. 2003. 26:189–192.
11. Hanouz JL, Bessodes A, Samba D, Gerard JL, Bricard H. Delayed diagnosis of vascular injuries during lumbar discectomy. J Clin Anesth. 2000. 12:64–66.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download