Abstract
Few literatures have elaborated on the clinical characteristics of children with thalassemia from low-prevalence areas. A retrospective analysis was conducted on children genetically confirmed with thalassemia at Seoul National University Children's Hospital in Korea. Nine children (1α thalassemia trait, 6β thalassemia minor, 2β thalassemia intermedia) were diagnosed with thalassemia at median age of 4.3 yr old with median hemoglobin of 9.7 g/dL. Seven (78%) children were incidentally found to be anemic and only 2 with β thalassemia intermedia had presenting symptoms. Five children (56%) were initially misdiagnosed with iron deficiency anemia. Despite the comorbidities due to α thalassemia mental retardation syndrome, the child with α thalassemia trait had mild hematologic profile. Children with β thalassemia intermedia had the worst phenotypes due to dominantly inherited mutations. None of the children was transfusion dependent and most of them had no complications associated with thalassemia. Only 1 child (11%) with codon 60 (T→A) mutation of the HBB gene needed red blood cell transfusions. He also had splenomegaly, cholelithiasis, and calvarial vault thickening. Pediatricians in Korea must acknowledge thalassemia as a possible diagnosis in children with microcytic hypochromic hemolytic anemia. High level of suspicion will allow timely diagnosis and managements.
Normal human hemoglobin (Hb) is a tetramer of two α-like and two β-like globin chains. Adult Hb is constituted by hemoglobin A (Hb A) (α2β2), hemoglobin F (Hb F) (α2γ2) and small amounts of hemoglobin A2 (Hb A2) (α2δ2) (1). The production ratio of α and β globin chains is tightly controlled in a normal individual. HBA1 gene and HBA2 gene are the α globin genes located on chromosome 16p13.3, and HBB gene is the β globin gene located on chromosome 11p15.5. In α or β thalassemia, mutation of α or β globin gene results in decreased production of that globin chain. Consequently, the other globin chain, produced in normal amounts from a normal gene, is in relative excess. It is the excessive globin chains that fail to form soluble tetramers on their own and cause a variety of manifestations in patients with thalassemia. In general, excessive β globin chains are less toxic than excessive α globin chains, and this explains the less severe clinical manifestations of α thalassemia (1).
In α thalassemia, it is the number of allelic mutations or deletions of α globin genes that determines the phenotype from silent carrier, α thalassemia trait, Hb H disease to hydrops fetalis. In β thalassemia, it is the degree of expression of the β globin gene that determines the phenotype from β thalassemia minor, intermedia to major (1, 2).
The classical form of β thalassemia is inherited in Mendelian recessive manner, and 2 mutant alleles are required for clinical manifestation. In such form, quantitative deficiency of the β globin chains contributes to β thalassemia. In comparison, the rare form of β thalassemia is inherited in autosomal dominant manner, and 1 mutant allele can result in clinical manifestation. In this form, ineffective erythropoiesis due to the extremely unstable β globin variants results in further deficiency of the β globin chains and contributes to β thalassemia with relatively severe manifestation. The β globin variants in the dominant β thalassemia are so unstable and easily degradable that they are detected only when newly synthesized (3).
Thalassemia is one of the most common disorders worldwide and is becoming a growing global public health problem (2, 4). However, it is uncommon in Korea. The carrier frequency of β thalassemia was reported to be around 0.1% in Korea, compared to 14% in Cyprus, the highest in the world (1, 5, 6). There is no recent report on the carrier frequency of α thalassemia in Korea, but it is generally thought to be lower. Nonetheless, new cases of thalassemia are continuously being diagnosed in Korea with a growing awareness of this disease.
Despite the relative low incidence of thalassemia in Korea, it must be considered in the differential diagnosis of microcytic hypochromic hemolytic anemia. Few reports have thus far focused on the clinical characteristics of thalassemia subjects in low-prevalence areas. Even fewer have elaborated on that of children from these areas (6). In this study, we analyzed the clinical, hematological and genetic characteristics of children diagnosed with α or β thalassemia in a pediatric institute in Korea.
A retrospective medical record review was done on children genetically confirmed with α or β thalassemia between January 2000 and December 2011 at Seoul National University Children's Hospital, Seoul, Korea.
Hb A, Hb F and Hb A2 were quantified with Hb electrophoresis. Mutational analysis was performed with direct sequencings of genomic deoxyribonucleic acid amplified through polymerase chain reaction (PCR) to determine the presence of mutations of α globin gene (HBA1 gene and HBA2 gene on chromosome 16p13.3) or β globin gene (HBB gene on chromosome 11p15.5).
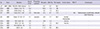
Nine children (6 boys and 3 girls) were newly diagnosed with thalassemia at median age of 4.3 yr old (range: 2.8-12.1 yr old), within 12 yr of study period in a single pediatric institute in Korea. Only 1 child (11%) had α thalassemia trait and 8 children had β thalassemia; 6 (67%) had β thalassemia minor and 2 (22%) had β thalassemia intermedia (Table 1).
Most of the children were asymptomatic. Seven children (78%) were incidentally found to be anemic on blood tests done for other reasons. Only 2 children, both of whom had β thalassemia intermedia, had presenting symptoms that led to the diagnosis of anemia, either jaundice or red urine. It took median 2 yr from initial diagnosis of anemia to diagnosis of thalassemia, during which 5 (56%) of the children (1 with α thalassemia trait and 4 with β thalassemia minor) were refractory to oral iron, supplemented under the suspicion of iron deficiency anemia (Table 1).
On initial blood tests, their median Hb was 9.7 g/dL (range: 8.5-11.0 g/dL), their median corrected reticulocyte (cReti) was 1.2% (range: 0.7%-6.7%) and their median total bilirubin (Tbil) was 0.8 mg/dL (range: 0.2-3.9 mg/dL). On Hb electrophoresis, their median Hb A2 was 2.9% (range: 1.6%-4.2%). Hemolytic anemia was evident on peripheral blood smears and none of them had iron deficient anemia (Table 1).
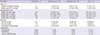
Only 1 mutant allele of either α or β globin gene was found in each of the children. The presence of dominantly inherited mutation distinguished β thalassemia intermedia from β thalassemia minor; children with the classical recessively inherited mutations were diagnosed with β thalassemia minor and children with the rare dominantly inherited mutations were diagnosed with β thalassemia intermedia (Table 2).
The child with α thalassemia trait had α thalassemia mental retardation syndrome, also known as ATR-16 syndrome. He had a large deletion of the chromosome 16 telomeric region, which extended from POLR3K to HBA1 on multiple ligation-dependent probe amplification. The resultant haplosufficient SOX8 gene led to intellectual disabilities as well as hemoglobinopathy (7, 8). In fact, he was found to be anemic on routine blood test done during a routine follow-up for localization related epilepsy and mental retardation. Despite his concomitant neurologic morbidities, his hemoglobinopathy was mild. He was diagnosed at oldest age, at 12.1 yr of age, and his hemolytic anemia was mild amongst current study population (Table 2).
Children with β thalassemia intermedia had the worst phenotype amongst the study population. They were diagnosed youngest, at median age of 3.8 yr old (3.6-4.1 yr old), after presenting with symptoms of jaundice or red urine; they were the only ones with presenting symptoms (Table 1). Their hemolytic anemia and hyperbilirubinemia were worst, both at initial presentation and at last follow-up. At initial presentation, their median Hb was 8.7 g/dL (range: 8.5-8.8 g/dL), their median cReti was 4.2% (range: 1.7%-6.7%) and their median Tbil was 2.8 mg/dL (range: 1.7-3.9 mg/dL) (Table 1). At last follow-up, their median Hb was 8.7 g/dL (range: 7.3-10.1 g/dL), their median cReti was 3.3% (range: 0.6%-6.1%) and their median Tbil was 4.8 mg/dL (range: 2.0-7.6 mg/dL) (Table 3).
Codon 60 (T→A) mutation and codon 121 (G→T) mutation of the HBB gene were the dominantly inherited mutations found in current study population. The child with codon 60 (T→A) mutation of the HBB gene was diagnosed at 3.6 yr old with initial Hb of 8.5 g/dL. He was the only child with evident splenomegaly at initial presentation (3, 9). The child with codon 121 (G→T) mutation of the HBB gene was born to a father who had splenectomy done for an undetermined hemolytic anemia; his father died soon after splenectomy due to sepsis (3, 6, 10). His younger sister and two cousins were subsequently found to have the same mutation (Table 2). These 4 children had median Hb of 9.1g/dL (range: 8.4-9.3 g/dL), median cReti of 1.2% (range: 0.9%-1.7%) and median Hb A2 of 3.2% (range: 2.7%-3.6%), at median age of 2.4 yr old (range: 1.8-3.9 yr old).
Most of the children did not need transfusions or other managements on regular follow-ups. Only 1 child (11%) with codon 60 (T→A) mutation of the HBB gene needed red blood cell (RBC) transfusions (Table 2). He had his first transfusion at 6 yr old and had 2 more at 9 yr old. At 10.9 yr of age, he is on folic acid and ursodeoxycholic acid. He has not required chelation therapy yet. The development of transfusion dependency will determine the need for hematopoietic stem cell transplantation during follow-up.
Most of the children did not have evident physical abnormalities or complications due to thalassemia. Only 1 child (11%) with codon 60 (T→A) mutation of the HBB gene had splenomegaly since diagnosis. Cholelithiasis was evident on abdominal ultrasonography done at 8.1 yr of age. Thickening of the calvarial vault with multiple vertical striations was found on a simple x-ray of the skull done at 9.6 yr of age (Table 2, 3). Up until his latest follow-up at 10.9 yr of age, he has neither developed symptoms due to cholelithiasis nor has required splenectomy. On regular follow-up at the outpatient clinic, symptomatic cholelithiasis or uncontrolled hemolysis and transfusion dependency will determine the need for cholecystectomy or splenectomy.
Follow-up measurements of body weights and heights were available in 8 children and 7 children, respectively. Only 1 child (11%) with α thalassemia trait had body weight and height under the 3rd percentile of national standard for age. Two children had body weights between the 3rd and 10th percentiles, and another 2 had body weights between the 10th and 50th percentiles. Three children had body weights above the 50th percentile. Five children had heights between the 10th and 50th percentiles and 1 child had height above the 50th percentile.
Regardless and because of the low incidence, characterization of thalassemia in Korea is important. This paper is the first to provide detailed descriptions of the clinical, hematological and genetic characteristics of pediatric thalassemia in Korea.
Most (78%) of the children were asymptomatic and were incidentally found to be anemic on blood tests done for other reasons. This suggests the possibility of underdiagnosis in Korea, especially for α thalassemia trait and β thalassemia minor. Due to the microcytic hypochromic nature of this anemia, many (56%) were treated with needless iron supplementations under the suspicion of iron deficiency anemia. This reiterates the need for appropriate confirmation of iron deficiency anemia with the necessary evaluations. Pediatricians in Korea must acknowledge thalassemia as a possible diagnosis in children with microcytic hypochromic hemolytic anemia even in Korea. High level of suspicion will allow timely diagnosis and managements and will allow the avoidance of needless examinations, iron supplementations or RBC transfusions.
β thalassemia was more frequent (89%) and α thalassemia was rarely found (11%). Although α thalassemia was rare, current study showed the possibility of α thalassemia with comorbidities due to large deletion mutation. Amongst β thalassemia children, none of them had β thalassemia major but a substantial portion of them had β thalassemia intermedia (25%). In a population where thalassemia is uncommon, this prevalence of β thalassemia intermedia was possibly due to the presence of dominantly inherited mutations in this population. These mutations are not only dominantly inherited but also produce extremely unstable β globin variants and thus result in β thalassemia intermedia even with 1 mutant allele (3).
During a median follow-up of 3.1 yr (range: 0.3-7.2 yr), only 1 child (11%) underwent RBC transfusions (Table 3). Fortunately, none of the children was transfusion dependent to date. The development of transfusion dependency during follow-up will necessitate hematopoietic stem cell transplantations. Only 1 child had physical abnormalities or complications associated with thalassemia and most of the children showed good physical growth.
The current study is limited by the small number of the study population within a single pediatric institute in Korea. Conclusion can be made neither on the overall picture of pediatric thalassemia in Korea nor on the genotype-phenotype correlation. This warrants a prospective, multicenter collaboration study with larger number of subjects. Furthermore, long-term follow-up data will aid further comprehensive understandings of thalassemia in Korea.
Figures and Tables
Table 1
Characteristics of the study population at initial evaluation

Thal, thalassemia; interm, intermedia; px, presentation; dx, diagnosis; Hb, hemoglobin; MCV, mean corpuscular volume; MCH, mean corpuscular hemoglobin; cReti, corrected reticulocyte; Hb A, hemoglobin A; Hb F, hemoglobin F; Hb A2, hemoglobin A2; AST, aspartate transaminase; ALT, alanine transaminase.
Notes
References
1. Cunningham MJ. Update on thalassemia: clinical care and complications. Hematol Oncol Clin North Am. 2010; 24:215–227.
2. Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010; 12:61–76.
3. Thein SL. Is it dominantly inherited beta thalassaemia or just a beta-chain variant that is highly unstable? Br J Haematol. 1999; 107:12–21.
4. Vichinsky EP. Changing patterns of thalassemia worldwide. Ann N Y Acad Sci. 2005; 1054:18–24.
5. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010; 5:11.
6. Park SS, Cho HI. Beta-thalassemia in the Korean population. Int J Hematol. 2002; 76:93–95.
7. Galanello R, Cao A. Gene test review: alpha-thalassemia. Genet Med. 2011; 13:83–88.
8. Gibson WT, Harvard C, Qiao Y, Somerville MJ, Lewis ME, Rajcan-Separovic E. Phenotype-genotype characterization of alpha-thalassemia mental retardation syndrome due to isolated monosomy of 16p13.3. Am J Med Genet A. 2008; 146A:225–232.
9. Podda A, Galanello R, Maccioni L, Melis MA, Rosatelli C, Perseu L, Cao A. Hemoglobin Cagliari (beta 60 [E4] Val----Glu): a novel unstable thalassemic hemoglobinopathy. Blood. 1991; 77:371–375.
10. Thein SL, Hesketh C, Taylor P, Temperley IJ, Hutchinson RM, Old JM, Wood WG, Clegg JB, Weatherall DJ. Molecular basis for dominantly inherited inclusion body beta-thalassemia. Proc Natl Acad Sci U S A. 1990; 87:3924–3928.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download