Abstract
Hepatobiliary complications, such as stone recurrence, recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma may occur after treatment for hepatolithiasis. However, few previous studies have addressed the risk factors and long-term outcomes after initial treatment. Eighty-five patients with newly diagnosed hepatolithiasis, actively treated for hepatolithiasis, constituted the cohort of this retrospective study. Patients were treated by hepatectomy or nonoperative percutaneous transhepatic cholangioscopic lithotomy. Long-term complications, such as recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma, and their relationships with clinical parameters were analyzed. The mean follow-up period was 57.4 months. The overall hepatobiliary complication rate after the treatment was 17.6%. Multivariate analysis of suspected risk factors showed that complications were associated with age (HR, 1.046; CI, 1.006-1.089), bile duct stricture (HR, 4.894; CI, 1.295-18.495), and residual stones (HR, 3.482; CI, 1.214-9.981). In conclusion, several long-term hepatobiliary complications occur after hepatolithiasis treatment, and regular observation is necessary in patients with concomitant biliary stricture or residual stones.
Hepatolithiasis, that is, the formation of stones in the intrahepatic biliary tree, is most prevalent in East Asia, including China, Japan, and Korea (1). The goals of primary treatment are to resolve ongoing infections and to prevent recurrent cholangitis, subsequent hepatic fibrosis, and progression to cholangiocarcinoma (2). However, complications associated with hepatolithiasis, such as recurrent cholangitis, hepatic cirrhosis, and cholangiocarcinoma, frequently occur even after effective treatment. Long-term complications are usually considered to result from inadequate stone retrieval, concurrent biliary stricture, or long standing cholangitis (3, 4). However, few studies have evaluated the risk factors of these complications after hepatolithiasis treatment. Moreover, previous studies have only evaluated the risk factors of recurrent cholangitis after initial surgical and/or endoscopic treatment (5, 6). Furthermore, the results of previous articles are inadequate to identify the risk factors responsible for hepatobiliary complications after treatment. Therefore, we sought to identify the risk factors and long-term hepatobiliary outcomes with respect to recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma, in patients with hepatolithiasis after treatment.
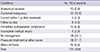
The medical records of 260 patients with hepatolithiasis that were surgically and/or endoscopically managed at our institution between December 1996 and August 2005 were retrospectively reviewed. We excluded 175 patients due to concurrent malignancy, underlying biliary cirrhosis, a congenital anomaly, incomplete medical records, or postoperative mortality (Table 1). Hepatolithiasis was confirmed by abdominal ultrasonography, computed tomography, endoscopic retrograde cholangiopancreatography, magnetic resonance cholangiopancreatography, and/or surgery. Ultrasonograpy was usually used for initial radiologic examinations. Further examinations depended on the ultrasonographic findings, severity of associated symptoms, combined clinical problems, and the intended mode of treatment. When the presence of intrahepatic duct stones, a liver mass, or a liver abscess was suspected based on sonographic findings, further examinations, such as abdominal CT, magnetic resonance cholangiopancreatography, and/or biopsy, were undertaken. Definite indications for hepatectomy were stones localized in a unilateral lobe, bile duct stricture associated with stones, or atrophy of the affected liver segments or lobe. Hepatectomy was performed at the lobe with intrahepatic stones. However, if treatment provided by endoscopic methods was inadequate in patients with stones in both lobes, a surgery strategy was adopted. On the other hand, patients at high operative risk, including the elderly, and those that refused operative treatment were treated endoscopically.
Follow-up was defined as time from date of discharge after initial treatment to the detection of subsequent cholangitis, liver abscess, secondary biliary cirrhosis, or cholangiocarcinoma. Patients were followed every 6 or 12 months. Some patients who dropped out were interviewed over the telephone. A residual stone was defined as a stone detected within 6 months by any diagnostic method. Bile duct stricture was defined as definite narrowing of bile duct documented by cholangiography, cholangioscopy, or surgery. Recurrent cholangitis was defined as a condition accompanied by presence of abdominal pain, fever, and/or jaundice without any other infection focus outside the hepatobiliary system requiring antibiotic administration. Liver abscesses were detected by imaging studies. Cholangiocarcinoma was confirmed by surgical resection or endoscopic or percutaneous biopsy. All specimens were examined by expert pathologists.
Univariate analysis of individual and total hepatobiliary complications was performed using the chi-square test, Fisher's exact test, and the t-test. Cox regression analysis was used to identify factors that influenced long-term survival. P values of < 0.05 were considered statistically significant. The analysis was performed using SPSS ver. 11.5 for Windows (SPSS Inc., Chicago, IL, USA).
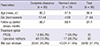
We recruited 85 hepatolithiasis patients, all of whom were actively treated. Baseline clinical characteristics are shown in Table 2. There were 21 men and 64 women, whose ages ranged from 37 to 83 yr (mean, 59.4 yr). Of the patients, 65 were surgically treated and 20 underwent percutaneous transhepatic cholangioscopic lithotripsy (PTCSL). Residual stones were found in 24 patients (28.2%) after initial treatment. Residual stone rates were 35% in patients treated with PTCSL (7/20) and 26.2% in patients treated surgically (17/65). Biliary stricture was found in 35 patients, and 29/35 patients were manipulated by endoscopic dilation or segmental hepatectomy. When complete resection was done, residual stones or biliary strictures resolved spontaneously. However, surgery was performed in patients with stones located in bilateral lobes and liver atrophy in only one lobe, to prevent cholangiocarcinoma. Similarly, partial segmentectomy was performed in patients with segmental atrophy of the liver and inadequate liver function. Resultantly, residual stones and stricture remained in some surgically treated patients.
Mean follow-up was 57.4 months. Complications were counted as individual events. Overall hepatobiliary complications occurred in 15 patients (17.6%). Recurrent cholangitis occurred in 14 (16.5%), liver abscess in 3 (3.5%), secondary biliary cirrhosis in 5 (5.9%), and cholangiocarcinoma in 2 (2.4%). Patients with recurrent cholangitis were treated by peroral transpapillary endoscopic lithotripsy (n=6), PTCSL (n=4), surgery (n=1), or systemic antibiotics only (n=3).
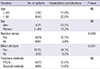
Univariate analysis showed that the presences of bile duct stricture and residual stones were significant predictors of hepatobiliary complications (P = 0.001, P = 0.009, respectively). The rate of hepatobiliary complication was 34.3% in patients with a biliary stricture and 37.5% in patients with a residual stone. Age, sex, and treatment methods were not found to be risk factors of hepatobiliary complications (Table 3).
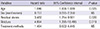
Multivariate analysis included age, sex, the presence of a residual stone, the presence of bile duct stricture, and treatment method. Age (HR, 1.046; CI, 1.006-1.089), bile duct stricture (HR, 4.894; CI, 1.295-18.495), and residual stone (HR, 3.482; CI, 1.214-9.981) were found to be independently correlated with the risk of developing a hepatobiliary complication (Table 4). Fig. 1 demonstrates the cumulative risks of hepatobiliary complications according to the presence of bile duct stricture or a residual stone, respectively.
Although hepatolithiasis is a benign condition, the clinical progression of the disease may lead to liver parenchymal destruction due to recurrent cholangitis (7). Furthermore, hepatolithiasis can subsequently result in biliary cirrhosis and even cholangiocarcinoma (8), which usually result from inadequate stone removal or stricture treatment (2).
Residual stones are the most troublesome problem after treatment (9). In a previous study, the overall recurrence rate of hepatolithiasis and/or cholangitis in patients with a residual stone after initial treatment was 57% (39/69). On the other hand, the recurrence rate of hepatolithiasis and/or cholangitis in patients without a residual stone was only 17% (27/167). In addition, it has been reported that recurrent biliary symptoms were more common in patients with a residual stone than in patients without a residual stone (6). Another retrospective study of 193 patients with hepatolithiasis, who had been newly diagnosed and treated, reported similar results (4). In the study, cholangitis developed more commonly in patients with retained stones after hepatolithiasis treatment and cholangitis also developed more in patients with recurrent calculi in intrahepatic bile ducts than in patients without residual or recurrent stones (60% and 55% vs 29% and 9%, respectively). The results are similar to the present study, in which the complication rate in patients with a residual stone after hepatolithiasis treatment was 37.5% but the rate in patients without a residual stone was only 9.8%. Furthermore, multivariate analysis showed that the presence of a residual stone was independently related to the risk of developing a hepatobiliary complication. In our experience, hepatolithiasis patients who retained residual stones even after aggressive treatment often had a good prognosis without any hepatobiliary events during long-term follow-up. We speculate that the good prognosis in this subset of patients with a residual stone, was due to the tendency of residual stones to locate to the peripheries of intrahepatic ducts and not to migrate into main ducts. Nevertheless, the presence of a residual stone was found to be an independent risk factor of a long-term hepatobiliary complication.
Intrahepatic biliary stricture is a major cause of treatment failure for intrahepatic stones and the main cause of stone recurrence. Biliary stricture often gives rise to bile stasis, cholangitis, and stone formation, and if the diseased ducts are not removed, the possibility of stone recurrence is high (2). One retrospective study reviewed 74 patients treated for hepatolithiasis. At 1- to 23-yr follow-ups, patients with a bile duct stricture were found to have a higher rate of incomplete clearance (30% [11/37] vs 5% [2/37]; P < 0.05). Furthermore, the recurrence rate of hepatolithiasis was higher in patients with a bile duct stricture (69% [18/26] vs 37% [13/35]; P < 0.05) (9). In another series, biliary stricture was found to be associated with a recurrent hepatobiliary complication after treatment, and the rate of stone and/or cholangitis recurrence was greater in patients with an intrahepatic duct stricture than in those without (31% [41/133] vs 47% [16/34]; P = 0.075). Furthermore, multivariate analysis showed that an intrahepatic duct stricture was an independent risk factor of stone recurrence, cholangitis, and residual stones after treatment (4). In the present study, hepatobiliary complication rate was 34.3% in patients with a biliary stricture, and by multivariate analysis, bile duct stricture was independently correlated with the risk of developing a hepatobiliary complication (Table 4). These findings show that complete stone clearance and the elimination of intrahepatic duct strictures, is necessary to prevent recurrent hepatobiliary complications in patients with hepatolithiasis.
Stricture dilation with a balloon catheter has been reported to decrease the risk of recurrent cholangitis in hepatolithiasis concurrent with biliary stricture (10). However, biliary stricture has also been reported to be an independent risk factor of long-term hepatobiliary complications in patients with hepatolithiasis, regardless of stricture dilation (5).
Generally, the prevalence of intrahepatic stones increases with age (11). However, we were unable to find any study that investigated the relations between recurrent hepatolithiasis and age. In the present study, patient age was found to be an independent risk factor for a long-term hepatobiliary complication. An age threshold was used to evaluate its influence on the rate of recurrent hepatobiliary complications. Univariate analysis showed that age was not a significant risk factor of a hepatobiliary complication, but Cox proportional hazards analysis showed that age was significantly associated with a long-term hepatobiliary complication.
A previous study concluded that hepatectomy is more effective than non-hepatectomy surgical treatment for hepatolithiasis (3). Hepatectomy seems to be the most definitive approach because it allows stone and biliary stricture removal simultaneously, and thus, reduces the risk of intrahepatic stone recurrence (12). However, other surgical methods, such as, choledochoenterostomy and T-tube drainage are available (13). Sometimes surgery may not be an option in those at high surgical risk who refuse surgery, or those that have undergone biliary surgery, or when stones are distributed in multiple segments (14). Non-surgical approaches to hepatolithiasis consist of endoscopic and/or radiological procedures. The endoscopic treatment of hepatolithiasis is considered relatively safe (11), but access is limited by strictures, ductal angulation, and the degree of stone impaction (12). The cholangioscopy was introduced to visualize stones, blood clots, air bubbles, and duct strictures and to improve stone clearance success rates (15). The first use of percutaneous transhepatic cholangioscopic lithotripsy for the treatment of hepatolithiasis was described in 1981, and it is now common used to remove intrahepatic duct stones non-surgically. However, almost 40% of cases of hepatolithiasis patients have intrahepatic bile duct strictures, which make stone extraction difficult (2). Furthermore, bile duct strictures prevent the definitive removal of sclerotic damage to intrahepatic biliary ducts, and this predisposes the recurrence of septic complications and the need for repeated treatments (16). In our study, treatment method was not found to be a significant risk factor of hepatobililary complications after initial treatment for hepatolithiasis by statistical analysis. However, this result could have been caused by selective bias, because when decisions were made regarding surgical and endoscopic methods, patient condition and location of stones in the biliary tract were considered. Thus, when stones were deemed not amenable to endoscopy, a surgical method was chosen. Our study also has other limitations. First, it is inherently limited by its retrospective nature and particularly by the absence of clear clinical information. Second, the study involved a relatively small number of patients, and it was performed at a single medical center, and thus, our results may not be representative of the general population. More specifically, the incidence of cholangiocarcinoma and the residual stone rate could have been affected by bias, as is suggested by a lower incidence of cholangiocarcinoma and a higher residual stone rate than have been previously reported.
In conclusion, the present study shows the presence of a bile duct stricture is the strongest predictor of subsequent complications after initial treatment for hepatolithiasis. Furthermore, hepatobiliary complications, such as, recurrent cholangitis, liver abscess, secondary biliary cirrhosis, and cholangiocarcinoma may occur frequently even after multidisciplinary treatment. Therefore, close observation is required especially in hepatolithiasis concomitant with bile duct stricture or residual stones, and in the elderly, even after constructive treatment.
Figures and Tables
Fig. 1
Cumulative rate of hepatobiliary complications by risk factors. (A) Biliary stricture as a risk factor (P < 0.05). (B) Residual stone as a risk factor (P < 0.05). These graphs show that complications are more common in patients with a biliary stricture or residual stones after treatment for hepatolithiasis.

References
1. Lee JY, Kim JS, Moon JM, Lim SA, Chung W, Lim EH, Lee BJ, Park JJ, Bak YT. Incidence of cholangiocarcinoma with or without previous resection of liver for hepatolithiasis. Gut Liver. 2013; 7:475–479.
2. Uchiyama K, Kawai M, Ueno M, Ozawa S, Tani M, Yamaue H. Reducing residual and recurrent stones by hepatectomy for hepatolithiasis. J Gastrointest Surg. 2007; 11:626–630.
3. Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, Kim MH. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007; 39:731–736.
4. Hwang JH, Yoon YB, Kim YT, Cheon JH, Jeong JB. Risk factors for recurrent cholangitis after initial hepatolithiasis treatment. J Clin Gastroenterol. 2004; 38:364–367.
5. Sakpal SV, Babel N, Chamberlain RS. Surgical management of hepatolithiasis. HPB (Oxford). 2009; 11:194–202.
6. Kim EH, Kim HJ, Oh HC, Lee KH, Jung JY, Kim S, Lee SS, Seo DW, Kim MH, Lee SK. The usefulness of percutaneous transhepatic cholangioscopy for identifying malignancies in distal common bile duct strictures. J Korean Med Sci. 2008; 23:579–585.
7. Yang SH, Lee SE, Jang JY, Ryu JK, Kim YT, Yun YB, Kim SW. Clinical and epidemiological analysis of gallstone patients: focused on 25-year experience of surgically treated patients. Korean J Gastroenterol. 2007; 50:42–50.
8. Tian J, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG. Laparoscopic hepatectomy with bile duct exploration for the treatment of hepatolithiasis: an experience of 116 cases. Dig Liver Dis. 2013; 45:493–498.
9. Kim MH, Lee SS. Current status of intrahepatic stones in Korea. Korean J Gastroenterol. 2003; 42:89–95.
10. Kim BW, Wang HJ, Kim WH, Kim MW. Favorable outcomes of hilar duct oriented hepatic resection for high grade Tsunoda type hepatolithiasis. World J Gastroenterol. 2006; 12:431–436.
11. Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009; 146:843–853.
12. Lee SE, Jang JY, Lee JM, Kim SW. Selection of appropriate liver resection in left hepatolithiasis based on anatomic and clinical study. World J Surg. 2008; 32:413–418.
13. Eun JR, Jang BI, Lee JY, Kim KO, Lee SH, Kim TN, Lee HJ. Clinical characteristics of intrahepatic cholangiocarcinoma and prognostic factors in patients who received non-surgical treatment. Korean J Gastroenterol. 2009; 54:227–234.
14. Lai EC, Ngai TC, Yang GP, Li MK. Laparoscopic approach of surgical treatment for primary hepatolithiasis: a cohort study. Am J Surg. 2010; 199:716–721.
15. Chen C, Huang M, Yang J, Yang C, Yeh Y, Wu H, Chou D, Yueh S, Nien C. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005; 19:505–509.
16. Catena M, Aldrighetti L, Finazzi R, Arzu G, Arru M, Pulitanò C, Ferla G. Treatment of non-endemic hepatolithiasis in a Western country: the role of hepatic resection. Ann R Coll Surg Engl. 2006; 88:383–389.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download