Abstract
We aimed comparing two-year clinical outcomes of the Everolimus-Eluting Promus and Paclitaxel-Eluting TAXUS Liberte stents used in routine clinical practice. Patients with objective evidence of ischemia and coronary artery disease eligible for PCI were prospectively randomized to everolimus-eluting stent (EES) or paclitaxel-eluting stent (PES) groups. The primary end-point was ischemia-driven target vessel revascularization (TVR) at 2 yr after intervention, and the secondary end-point was a major adverse cardiac event (MACE), such as death, myocardial infarction (MI), target lesion revascularization (TLR), TVR or stent thrombosis. A total of 850 patients with 1,039 lesions was randomized to the EES (n=425) and PES (n=425) groups. Ischemic-driven TVR at 2 yr was 3.8% in the PES and 1.2% in the EES group (P for non-inferiority=0.021). MACE rates were significantly different; 5.6% in PES and 2.5% in EES (P = 0.027). Rates of MI (0.8% in PES vs 0.2% in EES, P = 0.308), all deaths (1.5% in PES vs 1.2% in EES, P = 0.739) and stent thrombosis (0.3% in PES vs 0.7% in EES, P = 0.325) were similar. The clinical outcomes of EES are superior to PES, mainly due to a reduction in the rate of ischemia-driven TVR.
First generation drug-eluting stent (DES) dramatically reduced in-stent restenosis (ISR) by inhibiting neointimal hyperplasia (1, 2). The principal goal of second generation DES, including the everolimus-eluting stent (EES), was to overcome these concerns regarding issues such as stent thrombosis while maintaining efficacy. A considerable amount of comparative data is available concerning the clinical results of second generation DES and first generation DES, such as, the TAXUS express stent. However, long-term clinical data about the everolimus-eluting stent and the paclitaxel-eluting stent are inadequate. Accordingly, the aim of this study was to evaluate the procedural outcomes and short and long-term clinical outcomes of the PROMUS™ Everolimus-eluting stent and to compare these with those of the TAXUS Liberte™ Paclitaxel-eluting stent.
This study was designed as a prospective, randomized, open label, two arm, multicenter trial to compare the PROMUS™ Everolimus-eluting stent (EES; Abbott Vascular, Abbott Park, IL, USA) and the Taxus Liberte™ Paclitaxel-eluting stent (PES; Boston Scientific, Natick, MA, USA) in patients with coronary arteries of ≥ 2.5 and ≤ 3.75 mm of diameter with a lesion of length ≤ 46 mm (estimated visually) eligible for percutaneous coronary intervention (PCI).
Eight hundred and fifty (850) patients were enrolled at 18 centers in Korea, and randomized on a 1:1 basis to Promus™ EES (n=425) or TAXUS Liberte™ PES (n=425) groups. Patients aged over 18 yr and eligible for PCI were included. The exclusion criteria applied were; any planned treatment of the target vessel other than with a drug-eluting stent, ST-segment elevation myocardial infarction development within 7 days prior to the procedure, a history of Paclitaxel or Everolimus allergy or of allergy to stent polymers or metals, serious hepatic or renal dysfunction, a history of a malignant tumor within the previous 5 yr, a history of PCI treatment within the previous year, chronic total occlusion (CTO), a left main coronary artery lesion (stenosis > 50%), a bifurcation lesion requiring elective stenting of the branch lesion (side branch vessel > 2.5 mm in diameter), in-stent restenosis of a lesion implanted with a bare-metal stent or drug-eluting stent, and a target lesion in saphenous vein graft. The study hypothesis was that the PROMUS stent would be non-inferior to the Taxus Liberte stent in terms of target vessel revascularization (TVR) at 2 yr after intervention. Initial study design and study flow chart for 2 yr were shown in Fig. 1.
PCI was performed using standard techniques. All patients received ≥ 300 mg aspirin orally and a loading dose of 300 mg of clopidogrel before coronary angiography (CAG), or after PCI for emergency cases. After PCI, patients were routinely treated with aspirin 100 mg/day, clopidogrel 75 mg/day, and/or cilostazol 200 mg/day at operator's discretion. Patients were advised to maintain life-long aspirin therapy. Clopidogrel duration was at operator's discretion based on considerations of lesion and procedural complexity.
Primary end-points were ischemia-driven TVR based on the presence of symptoms, positive functional test, or restenosis by angiography at 2 yr after PCI. Secondary endpoints were target lesion revascularization (TLR), myocardial infarction, death, and a composite of major adverse cardiac events (MACE) and stent thrombosis (ST). MACEs included all deaths, myocardial infarction (MI), and ischemia-driven target vessel revascularization (TVR) at 2 yr. MI was defined as typical ischemic chest pain, ST-segment, or T-wave abnormalities with a creatine kinase-MB level ≥ 2 times higher than the reference value, without any new pathologic Q waves. Periprocedural MI was not included as clinical events in this study. TLR was defined as surgical or percutaneous re-intervention driven by significant (> 50%) luminal narrowing within a stent or with 5 mm proximal or distal to a stent in the presence of angina symptoms or objective evidence of ischemia. Ischemia-driven TVR was defined as the need for emergency or elective coronary artery bypass grafting or repeat PCI in a target vessel due to chest pain or a positive test result for ischemia (exercise stress test, stress echocardiogram, 24-hr Holter monitoring, evidence of ST segment depression or increase in > 1 electrocardiogram lead at rest, or a radionuclide study showing a reversible defect). ST was defined as previously described by the Academic Research Consortium (3).
Results are expressed as means ± SDs or numbers (%). The chi-square test was used to compare categorical variables, and the Student's t-test was used to compare continuous variables. P values of < 0.05 were considered statistically significant. Statistical was used to determine if TVR at 2 yr after index PCI with the Promus everolimus-eluting stent was non-inferior to the TAXUS Liberte paclitaxel-eluting stent in all study subjects. Based on the results of TAXUS trials, such as, the ATLAS, SPIRIT I and SPIRIT II trials (4-6), we assumed a TVR rate of 8% in both arms. Calculation to the sample size was based on a margin of non-inferiority for TVR 5%. Using a 1-sided significance level of 5%, we estimated that 365 patients per group were needed to detect this difference with a statistical power of 80%. Thus, in the expectation that approximately 15% of patients would be lost to follow-up, the total sample size was estimated to be 858 (429 patients per group). Data were analyzed using SPSS ver. 12.0 for Windows (SPSS, Chicago, IL, USA).
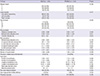
Group baseline characteristics were not statistically different (Table 1). Angiographic and procedural findings are summarized in Table 2. A considerable proportion of patients had a single vessel affected with a left anterior descending artery lesion. Pre- and post-procedural findings were similar in the two groups, as were rates of procedure-related myocardial infarction (6.7% in the PES group vs 6.8% in the EES group, P = 1.000). Stent length in the PES group tended to be longer (25.5 ± 11.0 mm in PES vs 24.1 ± 10.1 mm in EES, P = 0.061). Procedural success was achieved in 100% in the PES group and in 99.8% in the EES group (P = 0.495).
The overall clinical follow-up rate at 1 yr after PCI was 97.1% (826/850). Cumulative clinical outcomes at 1 yr after-PCI are summarized in Table 3. Total MACE rates were 3.9% in the PES group and 1.9% in the EES group (P = 0.090). All death rates were similar (0.7% in PES vs 1.0% in EES, P = 0.719) and MI rates were non-significantly different (0.7% in PES vs 0% in EES, P = 0.080). Rates of TLR (1.5% in PES vs 1.0% in EES, P = 0.510) and of ischemia-driven TVR (2.4% in PES vs 1.0% in EES, P = 0.100) were not significantly different. Stent thrombosis rates were similar in the two groups (0% in PES vs 0.7% in EES, P = 0.666).
The two-year clinical follow-up was completed by 93.7% (797/850); results are summarized in Table 3. Ischemia driven TVR at 2 yr (the primary end-point) was 3.8% in the PES group, and this was non-inferior to the 1.2% found for the EES group (P for non-inferiority=0.021). Moreover, TLR rates were higher in the PES than in the EES group (3.5% vs 1.2%, P = 0.037). The cumulative MACE rate at 2 yr was higher in the PES group (5.6% vs 2.5%, P = 0.027). However, rates of MI (0.8% for PES vs 0.2% for EES, P = 0.308) and all deaths (1.5% for PES vs 1.2% for EES, P = 0.739) were similar. Stent thrombosis rates at 2 yr were also similar in the two groups (0.3% for PES vs 0.7% for EES, P = 0.325). One definite stent thrombosis developed in the PES group, two possible STs in the EES group, and one probable ST in the EES group. Three STs were late and one was very late over 1 yr. Fig. 2 shows that ischemia-driven TVR-free survivals were significantly different in the two groups (P = 0.023). Fig. 3 shows that group MACE-free survivals at 2 yr were also significantly different (P = 0.030).
The PROMISE study shows that the clinical outcomes of Promus™ EES at 2 yr after PCI are non-inferior to those of Taxus Liberte™ PES, and that this was mainly due to a reduction in the ischemia-driven TVR rate. Cumulative MACE at 2 yr was excellent for both stents and death and MI rates were no different in the two groups. Furthermore, group ST rates were similar.
Second generation DES, such as EES, were developed due to safety concerns such as stent thrombosis development. Many trials have compared clinical outcomes between different types of stent, but to date, none of studies has given correct answers. Nevertheless, but TLR, TVR and stent thrombosis rates have decreased significantly as compared with first generation DES, especially in diabetes patients (7-9).
Recently the results of the retrospective REWARD TLX trial were published. It was found that mortality rates were similar for the Xience V EES and Taxus Liberte PES (10). However, in terms of composite efficacy and safety, EES exceeded PES. The present study also showed mortality rates were no different in the two groups, but in terms of ischemia-driven TVR, EES produced better results than PES. The COMPARE study showed that EES produced better MACE associated clinical outcomes, such as, for stent thrmobosis, MI, and TLR, than the TAXUS Liberte PES in non-selected patients (8). Contrary to the 1 yr follow-up in the COMPARE study, we found that the beneficial effects of EES continued for 2 yr, especially with respect to ischemia-driven TVR and TLR. In the COMPARE study, the MI rate was significantly lower in the EES group than in the PES group, and this was attributed due to a significant lower rate of early stent thrombosis. In the present study, 4 cases of ST occurred. One definite ST was observed in the Taxus Liberte PES group and 3 (two possible and one probable) in the Promus EES group. These four cases involving three cases of late ST and one of very late ST, but no case of acute or sub-acute ST was encountered. As was mentioned in the report issued on the REWARDS TLX trial, an early high rate of ST could be associated with technical procedural issues or complex lesions (11).
In the present study, rates of MACE (5.6% in the PES group and 2.5% in the EES group) were lower than those found in previous studies (6, 8, 10, 12). For example, in the REWARD TLX trial, MACE rates were 7.8% in the EES group and 10.8% in the PES Liberte stent group and in the COMPARE study, rates were 6% in the EES group and 9% in the PES Liberte group. We thought that this discrepancy was caused by the exclusion of patients with ST-segment elevation MI in the present study. In the REWARD TLX and the COMPARE study, patients were enrolled with ST-segment elevation MI ranging from 6.2% to 27% (10).
Regarding study limitations, first, we did not perform routine angiographic follow-ups after PCI in the absence of chest pain or a need for urgent revascularization, which could have compromised angiographic findings regarding, for example, late loss. Second, Taxus Liberte stent is not a current trend in the era of second generation DES such as everolimus eluting stent. However, our objective for this study is to compare first generation DES such as Taxus Liberte and second genenration DES such as everolimus-eluting stent. From this comparison, we reconfirm additional evidence of superiority of everolimus eluting stent to Taxus Liberte stent and long-term clinical outcomes for 2 yr. Third, although this was an open label study, revascularization could be influenced by operator's intention. So, we administered Adjudication Committee and they decided whether the clinical events were optimal for our intention or not. Fourth, our follow-up rate was low as 93.7%. This low follow-up rate for 2 yr might have impacted on the overall trial results.
In conclusion, this study shows that second generation DESs, such as, the Taxus Liberte PES and Promus EES, produce excellent clinical outcomes. Furthermore, the clinical outcomes of EES at 2 yr post-PCI are found to be superior to those of PES, mainly because of a reduction in ischemia-driven TVR.
Figures and Tables
Fig. 1
Initial study design and study flow chart. EES, everolimus-eluting stent; PES, paclitaxel-eluting stent; Id-TVR, ischemia-driven target vessel revascularization; MACE, major adverse cardiac events; TLR, target lesion revascularization; MI, myocardial death.

Fig. 2
The primary study end-point was ischemia-driven target vessel revascularization (TVR)-free survival rate at 2 yr post-PCI, and a significant difference was found between the two study groups (99% for the Promus™ Everolimus-eluting stent and 96% for the Taxus Liberbe™ Paclitaxel-eluting stent, P = 0.023).
Notes
References
1. Popma JJ, Leon MB, Moses JW, Holmes DR Jr, Cox N, Fitzpatrick M, Douglas J, Lambert C, Mooney M, Yakubov S, et al. Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Circulation. 2004; 110:3773–3780.
2. Stone GW, Ellis SG, Cox DA, Hermiller J, O'Shaughnessy C, Mann JT, Turco M, Caputo R, Bergin P, Greenberg J, et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004; 350:221–231.
3. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.
4. Turco MA, Ormiston JA, Popma JJ, Mandinov L, O'Shaughnessy CD, Mann T, McGarry TF, Wu CJ, Chan C, Webster MW, et al. Polymer-based, paclitaxel-eluting TAXUS Liberté stent in de novo lesions: the pivotal TAXUS ATLAS trial. J Am Coll Cardiol. 2007; 49:1676–1683.
5. Serruys PW, Ong AT, Piek JJ, Neumann FJ, van der Giessen WJ, Wiemer M, Zeiher A, Grube E, Haase J, Thuesen L, et al. A randomized comparison of a durable polymer Everolimus-eluting stent with a bare metal coronary stent: the SPIRIT first trial. EuroIntervention. 2005; 1:58–65.
6. Serruys PW, Ruygrok P, Neuzner J, Piek JJ, Seth A, Schofer JJ, Richardt G, Wiemer M, Carrié D, Thuesen L, et al. A randomised comparison of an everolimus-eluting coronary stent with a paclitaxel-eluting coronary stent:the SPIRIT II trial. EuroIntervention. 2006; 2:286–294.
7. Kedhi E, Gomes ME, Lagerqvist B, Smith JG, Omerovic E, James S, Harnek J, Olivecrona GK. Clinical impact of second-generation everolimus-eluting stent compared with first-generation drug-eluting stents in diabetes mellitus patients: insights from a nationwide coronary intervention register. JACC Cardiovasc Interv. 2012; 5:1141–1149.
8. Kedhi E, Joesoef KS, McFadden E, Wassing J, van Mieghem C, Goedhart D, Smits PC. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet. 2010; 375:201–209.
9. Stone GW, Rizvi A, Newman W, Mastali K, Wang JC, Caputo R, Doostzadeh J, Cao S, Simonton CA, Sudhir K, et al. Everolimus-eluting versus paclitaxel-eluting stents in coronary artery disease. N Engl J Med. 2010; 362:1663–1674.
10. Waksman R, Ghali M, Goodroe R, Ryan T, Turco M, Ring M, McGarry T, Dobies D, Shammas N, Steinberg DH, et al. Percutaneous coronary intervention with second-generation paclitaxel-eluting stents versus everolimus-eluting stents in United States contemporary practice (REWARDS TLX Trial). Am J Cardiol. 2012; 110:1119–1124.
11. Maluenda G, Mitulescu L, Ben-Dor I, A Gaglia M Jr, Weissman G, Torguson R, F Satler L, Pichard AD, Bernardo NL, Waksman R. Retroperitoneal hemorrhage after percutaneous coronary intervention in the current practice era: clinical outcomes and prognostic value of abdominal/pelvic computed tomography. Catheter Cardiovasc Interv. 2012; 80:29–36.
12. Stone GW, Midei M, Newman W, Sanz M, Hermiller JB, Williams J, Farhat N, Mahaffey KW, Cutlip DE, Fitzgerald PJ, et al. Comparison of an everolimus-eluting stent and a paclitaxel-eluting stent in patients with coronary artery disease: a randomized trial. JAMA. 2008; 299:1903–1913.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download