Abstract
This study attempted to calculate and investigate the incidence of hospitalized acute myocardial infarction (AMI) and stroke in Korea. Using the National Health Insurance claim data, we investigated patients whose main diagnostic codes included AMI or stroke during 2006 to 2010. As a result, we found out that the number of AMI hospitalized patients had decreased since 2006 and amounted to 15,893 in 2010; and that the number of those with stroke had decreased since 2006 and amounted to 73,501 in 2010. The age-standardized incidence rate of hospitalized AMI, after adjustment for readmission, was 41.6 cases per 100,000-population in 2006, and had decreased to 29.4 cases in 2010 (for trend P < 0.001). In the case of stroke was estimated at 172.8 cases per 100,000-population in 2006, and had decreased to 135.1 cases in 2010 (for trend P < 0.001). In conclusion, the age-standardized incidence rates of both hospitalized AMI and stroke in Korea had decreased continuously during 2006 to 2010. We consider this decreasing trend due to the active use of pharmaceuticals, early vascular intervention, and the national cardio-cerebrovascular disease care project as the primary and secondary prevention efforts.
In Korea, the proportion of circulatory system diseases accounted for 22.0% of the all deaths in 2010 (1). In particular, the severity of cerebrovascular and cardiovascular diseases, among other diseases of the circulatory system, are such that they rank first and second, respectively, among mortality by single diseases in Korea (1). The Korea Statistical Information Service calculates and announces such mortality data annually, and mortality by cardio-cerebrovascular diseases effectively maintains a high rank every year.
Unlike mortality data, data of the incidence of cardio-cerebrovascular diseases available since 2007 are few. Regarding data of the entire incidence of cardio-cerebrovascular diseases in Korea known so far, there is the Center for Disease Control and Prevention report on the incidence rates of acute myocardial infarction (AMI) and stroke from 1995 to 2003 (2), and a study on trends in AMI incidence in Koreans from 1997 to 2007 (3). However, we cannot determine the current trends in cardio-cerebrovascular diseases because the available research data here are extremely insufficient compared to that of developed countries, and because a national level surveillance system that periodically yields incidence data does not exist.
A number of studies have analyzed the trends in the incidence of cardio-cerebrovascular diseases in many countries, and reported that incidence tends to decrease in most developed countries (4, 5). In the case of AMI, research based on the Framingham Heart Study (6) determined that incidence in the United States of America (USA) has decreased from the 1960s to the 1990s, and has decreased further in the late 1990s or towards 2000, according to research using hospitalization data (7, 8). In the United Kingdom (UK), research using national-level hospitalization data has determined that the incidence of AMI had decreased towards the 2000s (9). Research using data from the Danish National Health Service shows that the same has held true since 1984 (10). In Japan, hospital registration data have indicated that the incidence trends increased until the 1990s but leveled off in the 2000s (11). In the case of stroke, the Framingham Heart Study in USA found that incidence has decreased for the past 50 yr (12), and analyses using national-level data indicate that incidence has decreased since 1980 in the UK (13, 14). Furthermore, research involving the stroke registration system in Finland reveals that incidence has decreased since the 1980s (15), and the same tendency toward reduction has been observed in Japan and Hong Kong (16, 17).
As such, a number of countries have carried out a considerable amount of work on the incidence of cardio-cerebrovascular diseases, and current trends in incidence indicate a reduction. However, we have not attempted to study the recent incident rates of cardio-cerebrovascular diseases in Korea. Thus, this study attempted to calculate and investigate the incidence of hospitalized AMI and stroke in Korea from 2006 to 2010 using the National Health Insurance (NHI) claim data of the entire nation.
The source data used for this analysis were those of the National Health Insurance Corporation's (NHIC) claims. These data, for the purpose of public research, were provided upon request by the Korea Centers for Disease Control and Prevention and 9 Regional Cardiocerebrovascular Centers.
The NHIC claim data consist of requests made by medical institutions in Korea to the NHIC in order to receive fees after providing medical services. For 2010, these data include approximately 800 million annual claims and the use of medical services by 48,906,795 medical insurance holders, and account for 96.7% of the entire national population, with 3.3% being the exception as medical aid recipients (18). In this study, we used a 5-yr data set from 2006 to 2010 and investigated hospitalized AMI or stroke patients at each year.
The NHI claim data contain principal and additional diagnoses, hospitalization/outpatient treatment, dates of examinations, medical fees, contents of medical services, prescribed medications, hospital codes, patients' genders, ages, etc., and are arrayed according to the claims made by medical institutions on the basis of the contents of their examinations. Specifically, a number of multiple, not single, claim data are generated if a patient is examined at several different hospitals, or at a single hospital but for several different conditions. In order to resolve this issue, we arranged the medical records based on individual patients, and extracted the years of hospitalization from the data of the hospitalized AMI and stroke cased for analysis. We used a structured identification code provided by the NHI to identify individual patients. The NHI erased all private information such as name, social security number, address and phone number from the original patient claim data.
The diagnoses in the NHI claim data were made in accordance with the Korean Standard Classification of Diseases (KSCD), which is based on the ICD-10 code, an International Classification of Diseases, and ischemic heart diseases fall within the I20-I25 codes (19). While different studies define and select different AMI diagnostic codes for different purposes or in different circumstances, the present analysis defined only the I21 code for patients with AMI onset because it focused on patients with newly occurring AMI. While cerebrovascular diseases fall within the I60-I69 codes in the KSCD, the present analysis included the I60-I63 codes in the diagnostic codes for stroke (19).
The subjects of this study were those patients who were hospitalized for AMI or stroke from January 1, 2006, to December 31, 2010. Though the NHI claim data contain principal and additional diagnoses, we selected patients hospitalized for principal diagnoses at each year. Given the characteristics of AMI and stroke, we excluded those who only received outpatient treatment but not hospital treatment because they were expected not to be newly diagnosed. As there were cases where some hospitalized patients were readmitted due to relapses or complications, we regarded such patients as having disease onset in the year of their first hospitalization, and excluded them if they were subsequently hospitalized. We also ruled out patients who were admitted into medical institutions as such as sanatoria or mental hospitals because such institutionalization was very likely not essential for acute treatment.
As disease incident means that a new disease occurs without previous conditions, patients who were hospitalized several times from 2006 to 2010 were regarded as subjects only in the year of their first hospitalization when we calculated the incidence rates. However, even with this approach, those who were readmitted during 2006-2010 but had had the condition before 2006 could not be considered patients with new disease onset. For example, a patient who developed a disease in 2005 and who was readmitted in 2006, though an affected, could be classified as one with disease onset in 2006 because we could not check the data before 2006. Mistaking affected patients for emerging patients in the year of observation in a study without previous information of incidence as such is known as the 'prevalent pool effect' (20). In order to adjust for prevalent pool effect, long-term data should be used to establish a clearance period for the years before the starting year of research deemed sufficient (2). Thus, being regarded as affected patients, patients who were hospitalized for the clearance period were ruled out, and only patients who were never admitted for the period were considered newly affected patients.
However, the current study did not establish a clearance period to exclude patients hospitalized for the period because it only analyzed the data from a 5-yr period (2006-2010). Instead, in order to resolve the prevalent pool effect issue, we assumed a readmission proportion derived from the analyzable 2006-2010 data for adjustment based on the hypothesis that the readmission proportion during the 4 yr before 2006 would be the same as that calculated from our data. To create formulae for these processes, let R1-R4 be the calculated readmission proportions for 1-4 yr afterwards, then the 2006 adjusted incident cases (AIC) = the 2006 total incident case (TIC) × (1 - [R1 + R2 + R3 + R4]), the 2007 AIC = the 2007 TIC × (1 - [R2 + R3 + R4]), the 2008 AIC = the 2008 TIC × (1 - [R3 + R4]), and the 2009 AIC = the 2009 TIC × (1 - R4).
The results are presented as the calculation of the incident cases of AMI and stroke, respectively, the proportion of male patients, mean ages, and the proportions among age groups (0-29, 30-44, 45-54, 55-64, 65-74, and over 75 yr). Moreover, we calculated the crude incidence rates for every 100,000 population, age-standardized incidence rates, and age-standardized incidence rates adjusted by readmission. In the calculation of crude incidence rates, the denominators were the numbers of registered residents in each year, and age-standardization is in 5 yr intervals. In the calculation of age-standardized incidence rates, the standard population was the mid-year population of registered residents in 2008. We subsequently calculated readmission proportions for 1-4 yr by checking whether the patients hospitalized in each year of observation were readmitted 1-4 yr after their first hospitalization, and the age-standardized incidence rates were adjusted with the calculated readmission proportions.
We carried out logistic regression using years as continuous variables to test yearly differences in the sex-based proportions of patients in each age group, and linear regression to test linear changes in the mean ages of yearly emerging patients. Tendencies of changes in yearly in-patient incidence rates were analyzed with Poisson regression. The analysis was carried out with SAS PROC GENMODE. The years with reference to 2006 were used as predictor variables, and the analysis was performed by separating response variables, including the numbers of the entire patient population, patients according to sex, and patients in each age group. The denominator, offset, was the population of registered residents in each group. We used SAS version 9.1 (SAS Institute, Cary, NC, USA) for all analyses, and the significance level is P < 0.05.
This study relied on secondary data from NHI. The data set did not include private information such as patient name, social security number, address, or phone number. Only non-identifiable aggregate results were released and they were openly available for public research purposes. For this reason, we did not seek institutional review board approval.
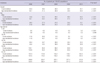
The subjects who were diagnosed with AMI and hospitalized for treatment for the first time in 2006 in Korea amounted to 20,730, since then, the number continuously decreased and arrived at 15,893 in 2010, a 23.3% reduction from that in 2006. Males accounted for 65.7% of all in-patients (13,619) in 2006, while females made up 34.3% (7,111) of all in-patients. Since then, the proportion of male patients gradually increased while that of females decreased, and hence the former accounted for 69.9% of all patients (11,105) and the latter for 30.1% (4,788) in 2010 (P < 0.001). The mean age of newly hospitalized subjects was 64.4 yr in 2006, and 64.8 yr in 2010. Though slight, the increase in onset age was significant (P < 0.001). The proportion of the 65-74 yr age group was highest from 2006 to 2010, but gradually decreased (P < 0.001). The proportion of in the over 75 yr age group significantly increased (P < 0.001) (Table 1).
The number of subjects who were diagnosed with stroke and hospitalized for the first time was 102,210 in 2006, and since then, it continuously decreased to 73,501 in 2010, a 28.1% reduction from that in 2006. Males accounted for 50.6% of the all in-patients in 2006, while females accounted for 49.4%. Since then, the proportion of male patients gradually increased to 53.6%, and that of female patients gradually decreased to 46.4% in 2010 (P < 0.001). The mean age of newly hospitalized subjects was 66.7 yr in 2006 and 67.2 yr in 2010, a significant 0.5 yr increase (P < 0.001). The proportion of the 65-74 yr age group was highest at 31.8% in 2006, but subsequently decreased. Since 2008, the proportion of the group aged over 75 yr was the highest, and subsequently increased (P < 0.001) (Table 1).
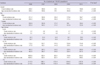
The AMI readmission proportion for 1 yr after the year of observation was 5.50%, that for 2 yr was 1.52%, that for 3 yr was 1.06%, and that for 4 yr was 0.91%. The readmission proportion was higher in male patients than in female patients and in the 30-44 yr age group than in other age groups (Table 2).
The stroke, the readmission proportion for 1 yr after the year of observation was 10.14%, that for 2 yr was 5.85%, that for 3 yr was 4.28%, and that for 4 yr was 3.44%. The readmission proportion was higher in female patients than in male patients and in the over 65 yr age group than in other age groups (Table 2).
The yearly crude incidence rates and age-standardized incidence rates of patients who were hospitalized for treatment of AMI for the first time from 2006 to 2010 are presented in Table 3, and the tendencies of the age-standardized incidence rates adjusted by readmission are illustrated in Fig. 1. The 2006 crude incidence rate was 42.4 cases per 100,000 population, and subsequently decreased in a statistically significant manner to 31.7 cases per 100,000 population in 2010 (P < 0.001). The 2006 age-standardized rate was 45.7 cases per 100,000 population, and subsequently decreased in a statistically significant manner to 29.4 cases per 100,000 population in 2010, 35.7% lower than that in 2006 (P < 0.001) (Table 3). The age-standardized incidence rate after adjusting for readmission also decreased continuously and significantly after 2006, and amounted to 29.4 cases per 100,000 population in 2010, 29.3% lower than that in 2006 (P < 0.001) (Fig. 1A).
In both sexes, the crude incidence rates of newly hospitalized patients, age-standardized incidence rates, and age-standardized incidence rates adjusted by readmission decreased continuously and significantly from 2006 to 2010 (P < 0.001). Moreover, all but the 0-29 yr age group, which had only a few affected patients, exhibited a significant decrease (P < 0.001) (Table 3, Fig. 1).
The 2006-2010 crude incidence rates of newly hospitalized patients with stroke, age-standardized incidence rates, and age-standardized incidence rates adjusted by readmission are presented in Table 4, and illustrated in Fig. 2. The 2006 crude incidence rate of stroke was 209.1 cases per 100,000 population, and it continuously decreased in a statistically significant manner to 146.6 cases per 100,000 population in 2010 (P < 0.001). The 2006 age-standardized incidence rate was 226.5 cases per 100,000 population, and decreased continuously and significantly to 135.1 cases per 100,000 population in 2010, 40.4% lower than that in 2006 (P < 0.001). The age-standardized incidence rate adjusted by readmission also decreased continuously and significantly from 2006, standing at 135.1 cases per 100,000 population in 2010, 21.8% lower than the 172.8 cases per 100,000 population in 2006 (P < 0.001) (Table 4, Fig. 2A).
In both sexes, the crude incidence rates of newly hospitalized patients, age-standardized incidence rates, and age-standardized incidence rates, after adjusting for readmission, continuously decreased significantly from 2006 to 2010 (P < 0.001). Moreover, all but the 0-29 yr age group, which had only a few affected patients, exhibited a significant reduction (P < 0.001) (Table 4, Fig. 2).
In order to examine recent trends in the incidence of AMI and stroke, we analyzed the NHI claim data, which contain the data of medical services used by 96.7% of the national population. Our analysis determined that the rates for crude incidence, age-standardized incidence, and age-standardized incidence after adjusting for readmission of patients hospitalized for treatment of AMI and stroke gradually decreased after 2006. Though this analysis has different output values compared with other studies carried out in Korea, the results suggest a similar tendency toward a reduction in incidence. The Health Insurance Review and Assessment Service analysis of the hospitalized AMI cased up to 2010 also determined that the number of hospitalized cases gradually increased from 20,322 in 2003 to peak at 23,080 in 2007, and then decreased to 21,636 in 2010 (21). Analyses of the incidence rate of patients hospitalized for AMI from 1997 to 2007 also reported that the age-standardized incidence rate was the highest at 82.1 cases per 100,000 population but decreased slightly to 78.3 cases per 100,000 population in 2007 (3). The report by the Korea Center for Disease Control (KCDC) that has analyzed the incidence rates of AMI and stroke from 1995 to 2003 from the NHI data, also demonstrated that the rates increased up to the early 2000s, but the tendency of increase slowed or became congested since 2002 or 2003 (2). To summarize these results, the incidence rates of hospitalized patients with cardio-cerebrovascular diseases in Korea may be considered to have become congested in the mid- 2000s, and then decreased since 2006 or 2007.
Until recently, much of the research on trends in the incidence and mortality of cardio-cerebrovascular diseases has been carried out in other countries. Though concerning different periods, the present results show that the decreasing trends in the incidence rates of cardio-cerebrovascular diseases in Korea are similar to those in other developed countries. Specifically, the USA has investigated trends in the incidence of cardio-cerebrovascular diseases since the 1950s through cohort data such as the Framingham study, and the Atherosclerosis Risk in Communities study, and currently monitors cardio-cerebrovascular disease incidence using large scale hospitalization data (6-8, 12, 22-24). Such studies in the USA reported that the incidence rates of cardio-cerebrovascular diseases have generally been decreasing since the 1960s or toward the late 1990s. Likewise, studies in the UK (9, 13, 14, 25) that examined trends in the incidence of cardio-cerebrovascular diseases using hospital registration data reported that the rates have decreased since the late 1990s or the early 2000s. As is the case in Korea, Denmark manages the medical service data for the entire national population via the health insurance system. Studies using such data report that the hospitalization rate of initial AMI has decreased since 1985 (10, 26). In addition, a study that analyzed research on stroke incidence in 56 countries via a systematic review of the literature reported that the rate has decreased in high-income countries since the 1970s (5), and some studies in Japan, a country geographically close to Korea and that possesses similar ethnic characteristics, also indicate that the rate has decreased since the 1970s (16). Additionally, Hong Kong studies have reported that the incidence rate of ischemic stroke has decreased until 2008 (17).
The reason cardio-cerebrovascular diseases began to decrease after the mid-2000s in Korea, as in other developed countries, is that preventive actions for the management and improvement of major risk factors of cardio-cerebrovascular diseases such as chronic illnesses and unhealthy lifestyles have paid off. This is because cardio-cerebrovascular diseases can be prevented by managing and improving risk factors such as chronic illnesses and unhealthy lifestyles, which are major contributors to the risk of cardio-cerebrovascular diseases (27). Most of the above mentioned studies also deem the preventive activities for managing and improving the risk factors as causes of the reduction in the incidence of cardio-cerebrovascular diseases (6, 8, 12-14, 22, 25). In fact, recognizing the importance of the prevention of chronic and cardio-cerebrovascular diseases, the Korean government established and carried out measures for the management of chronic diseases and cardio-cerebrovascular diseases in the 2000s (28). Accordingly, there has been no greater increase in the prevalence of hypertension, diabetes, and high cholesterol in Korea now than in the past, whereas the rates of awareness, treatment rate, and control rate have greatly improved in the 2000s. On the basis of such results, it is believed that the preventive care programs and projects for chronic illnesses and cardio-cerebrovascular diseases towards the 2000s in Korea are major contributors to the reduction in the incidence of cardio-cerebrovascular diseases.
We may consider the increase in the prescription of aspirin or statin medications as primary prevention to be another contributor to the reduced incidence of cardio-cerebrovascular diseases. Though there is no Korean research regarding the prescription rates or changes in the usage of such medications, we may conjecture that prescription or use has increased in comparison with that in the past. Drug prescription data in the USA and the UK have recorded a rapid rise in the use of anti-platelet drugs, such as aspirin, and lipid-lowering drugs since 1990 (8, 29), and the United States' Preventive Service Task Force recommended the prescription of aspirin for primary prevention of cardio-cerebrovascular diseases in 2002. Thus, it is believed that the incidence of cardio-cerebrovascular diseases has decreased due to the increased use of medications as primary prevention.
The incidence of AMI appears to have decreased as coronary angiography has been performed preventively on patients diagnosed with angina pectoris, a pre-stage of the disease. In fact, according to the analysis made by the Health Insurance Review and Assessment Service, while patients hospitalized for AMI decreased from the mid-2000s to 2010, patients hospitalized for ischemic heart diseases increased continuously from 2003, and there were 65.5% more patients in 2010 than in 2003. Coronary angiography cases also constantly increased, hence there were 30.1% more cases in 2009 than in 2006 (21, 30).
This study investigated trends in the incidence of cardio-cerebrovascular diseases using state level data. As the data used in this study were collected to claim medical service costs, this study has limitations in the sense that it could not examine actual clinic information including patients' symptoms and severities. In addition, the estimated incidence rates could have been lower than the actual rates derived from local society based investigations, because claims are not made for dead persons without hospital treatment after disease onset. Moreover, there could have been problems with the precision of diagnoses even if patients had received hospital treatment. In fact, a 2002 report analyzing the consistency between NHI data and hospitals' clinical data determined that approximately 69.7% diagnostic precision (31). However, we believe that the diagnostic consistence in AMI or stroke may be higher than 69.7% because diagnostic consistency is higher in out-patients than in-patients, in main diagnostic codes than additional diagnostic codes, in severe diseases than frequent diseases, and in specialized general hospitals than other hospitals. Furthermore, this study might have more or less underestimated the incidence rates, as it ruled out patients diagnosed with AMI or stroke in additional diagnostic codes because it analyzed the data only in the main diagnostic codes. However, issues arising from such underestimation would be trivial, given the characteristics of AMI and stroke. This study analyzed only the 5-yr data from 2006 to 2010. Due to the prevalence pool effects, we might have overestimated the crude incidence rates of in-patients. However, we calculated and adjusted the readmission proportions with the provided data in order to address this issue.
Despite such limitations, the greatest strength of this study is that we have calculated the incidence rates using data accounting for 96.7% of the entire national population. As only a few countries, have compiled the medical service data of the entire national population, estimation of incidence rates should be carried out only using cohort data in partial regions or the patient data registered in some hospitals. While such results may have limitations due to the lack of representativeness of the population in general, this study has the advantage of using data from the entire national population to overcome such limitations. Moreover, at a time when research that has estimated the recent incidence rates of cardio-cerebrovascular diseases in Korea is insufficient, this study has merit in that it presents the analysis of recent data. Such results can be used as materials for management and preventive programs for cardio-cerebrovascular diseases and for future research.
In conclusion, the age-standardized incidence rates of both hospitalized AMI and stroke in Korea decreased continuously during 2006 to 2010. We consider this decreasing trend due to the active use of pharmaceuticals, early vascular intervention, and the national cardio-cerebrovascular disease care project as the primary and secondary prevention efforts. And then, further study on the determinants of the decline in these trends for public health purposes would be necessary.
Figures and Tables
Fig. 1
Age-standardized incidence rate of hospitalized AMI after adjustment for readmission, 2006-2010. (A) Incidence overall and by sex. (B) Incidence by age groups (year).

Fig. 2
Age-standardized incidence rate of stroke after adjustment for readmission, 2006-2010. (A) Incidence overall and by sex. (B) Incidence by age groups (year).

References
1. Korea National Statistical Office. 2010 Annual report on the cause of death statistics. 2011. Daejeon, Korea: Korea National Statistical Office.
2. Korea Centers for Disease Control and Prevention. Development of strategy and action plans for major chronic diseases prevention and control. 2004. Seoul: Korea Centers for Disease and Prevention.
3. Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of AMI in Korea: 1997-2007. Korean Circ J. 2009. 39:467–476.
4. Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999. 353:1547–1557.
5. Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009. 8:355–369.
6. Parikh NI, Gona P, Larson MG, Fox CS, Benjamin EJ, Murabito JM, O'Donnell CJ, Vasan RS, Levy D. Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute's Framingham Heart study. Circulation. 2009. 119:1203–1210.
7. Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987-2008. Circulation. 2012. 125:1848–1857.
8. Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of AMI. N Engl J Med. 2010. 362:2155–2165.
9. Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from AMI in England between 2002 and 2010: linked national database study. BMJ. 2012. 344:d8059.
10. Schmidt M, Jacobsen JB, Lash TL, Bøtker HE, Sørensen HT. 25 year trends in first time hospitalisation for AMI, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ. 2012. 344:e356.
11. Takii T, Yasuda S, Takahashi J, Ito K, Shiba N, Shirato K, Shimokawa H. MIYAGI-AMI Study Investigators. Trends in acute myocardial infarction incidence and mortality over 30 years in Japan: report from the MIYAGI-AMI Registry Study. Circ J. 2010. 74:93–100.
12. Carandang R, Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Kannel WB, Wolf PA. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA. 2006. 296:2939–2946.
13. Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, Gutnikov SA, Edwards P, Mant D, Sackley CM, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet. 2004. 363:1925–1933.
14. Lee S, Shafe AC, Cowie MR. UK stroke incidence, mortality and cardiovascular risk management 1999-2008: time-trend analysis from the General Practice Research Database. BMJ Open. 2011. 1:e000269.
15. Sivenius J, Tuomilehto J, Immonen-Räihä P, Kaarisalo M, Sarti C, Torppa J, Kuulasmaa K, Mähönen M, Lehtonen A, Salomaa V. FINSTROKE study. Continuous 15-year decrease in incidence and mortality of stroke in Finland: the FINSTROKE study. Stroke. 2004. 35:420–425.
16. Kubo M, Kiyohara Y, Kato I, Tanizaki Y, Arima H, Tanaka K, Nakamura H, Okubo K, Iida M. Trends in the incidence, mortality, and survival rate of cardiovascular disease in a Japanese community: the Hisayama study. Stroke. 2003. 34:2349–2354.
17. Chau PH, Woo J, Goggins WB, Tse YK, Chan KC, Lo SV, Ho SC. Trends in stroke incidence in Hong Kong differ by stroke subtype. Cerebrovasc Dis. 2011. 31:138–146.
18. National Health Insurance Corporation, Health Insurance Review & Assessment Service. 2010 National Health Insurance statistical yearbook. 2011. Seoul, Korea: National Health Insurance Corporation, Health Insurance Review & Assessment Service.
19. Korea National Statistical Office. Korean standard classification of diseases. 2010. Daejeon, Korea: Korea National Statistical Office.
20. Brameld KJ, Holman CD, Lawrence DM, Hobbs MS. Improved methods for estimating incidence from linked hospital morbidity data. Int J Epidemiol. 2003. 32:617–624.
21. Health Insurance Review & Assessment Service. 2011 Result of AMI evaluation. 2011. Seoul, Korea: Health Insurance Review & Assessment Service.
22. Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, Wang CH, Heiss G. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998. 339:861–867.
23. Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010. 121:863–869.
24. Kleindorfer DO, Khoury J, Moomaw CJ, Alwell K, Woo D, Flaherty ML, Khatri P, Adeoye O, Ferioli S, Broderick JP, et al. Stroke incidence is decreasing in whites but not in blacks: a population-based estimate of temporal trends in stroke incidence from the Greater Cincinnati/Northern Kentucky Stroke Study. Stroke. 2010. 41:1326–1331.
25. Heuschmann PU, Grieve AP, Toschke AM, Rudd AG, Wolfe CD. Ethnic group disparities in 10-year trends in stroke incidence and vascular risk factors: the South London Stroke Register (SLSR). Stroke. 2008. 39:2204–2210.
26. Abildstrom SZ, Rasmussen S, Rosén M, Madsen M. Trends in incidence and case fatality rates of AMI in Denmark and Sweden. Heart. 2003. 89:507–511.
27. World Health Organization. 2008-2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases. 2008. accessed on 10 May 2012. Geneva: World Health Organization;Available at http://www.who.int/nmh/publications/9789241597418/en/index.html.
28. Ministry of Health, Welfare and Family Affairs. Guidebook of 2010 Major chronic disease management project. 2010. Seoul, Korea: Ministry of Health, Welfare and Family Affairs.
29. Scarborough P, Peto V, Bhatnagar P, Kaur A, Leal J, Luengo-Fernandez R, Gray A, Rayner M, Allender S. Stroke statistics 2009. 2011. accessed on 10 May 2012. Oxford, UK: British Heart Foundation;Available at http://www.bhf.org.uk/research/statistics/heart-statistics-publications.aspx.
30. Health Insurance Review & Assessment Service. Results of the first Coronary Artery Bypass Graft (CABG) evaluation. 2011. Seoul, Korea: Health Insurance Review & Assessment Service.
31. Park BJ, Sung JH, Park KD, Seo SW, Kim SW. Report of the evaluation for validity of discharged diagnosis in Korean Health Insurance database. 2003. Seoul, Korea: Seoul National University.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download