Abstract
Many cases of RET proto-oncogene mutations of hereditary medullary thyroid carcinoma (MTC) have been reported in Korea. However, MTC with V804M RET proto-oncogene germline mutations have not been reported in Korea. A 33-yr-old man was diagnosed with a 0.7-cm sized thyroid nodule. Laboratory testing revealed serum calcitonin was elevated. The patient underwent total thyroidectomy with central compartment neck dissection for the thyroid tumor. RET gene analysis was performed in both the index patient and his family. There were no V804M RET mutation and abnormal laboratory findings within his family except the index patient. Therefore, this patient was a de novo V804M RET germline mutation.
Medullary thyroid carcinoma (MTC) is an uncommon malignant tumor derived from calcitonin-producing C cells of the thyroid. Seventy five percent of all MTCs are sporadic, while the remaining 25% of MTCs occur in three well-defined familial syndromes; multiple endocrine neoplasia (MEN) 2A, MEN 2B, and familial medullary thyroid carcinoma (FMTC) (1). The inherited forms of MTC are autosomal dominant traits associated with point mutations of the RET proto-oncogene, which encodes a receptor tyrosine kinase that plays roles in the regulation of cell proliferation, migration, and differentiation (2).
In the literature, RET proto-oncogene mutations of MEN 2A and FMTC in Koreans have been observed most commonly in codons 634 and 618, and rarely in codons 630, 631, and 768 (3-5). However, MTC with codon V804M RET mutations has not reported in Korea. In the present study, we screened a Korean family in which one member had a rare V804M RET germline mutation that was detected by genetic analysis.
A 33-yr-old man (index patient) was incidentally diagnosed with a 0.7 cm sized nodule in the right thyroid at a general check-up on 30 January 2012 (Fig. 1). He had no personal or family history of hypertension or thyroid cancer. Physical exam was normal. Ultrasound (US) guided fine needle aspiration (FNA) was performed and was suspicious for MTC. Laboratory testing revealed serum calcitonin 23.9 pg/mL (normal range < 10 pg/mL), CEA 5.77 ng/mL (normal range < 5 ng/mL) Ca 9.4 mg/dL, P 3.9 mg/dL, and intact parathyroid hormone (iPTH) 27 pg/mL (normal range 15.0-65.0 ng/mL). The patient underwent total thyroidectomy with central compartment neck dissection for the thyroid tumor. Histological examination revealed MTC without metastasis. Genomic DNA was extracted from the peripheral blood leukocytes of both index patient and at-risk family members. Full sequencing of the RET gene and analyses of exons 10, 11, 13, 14, 15, and 16 were subsequently performed. Genetic analysis of the index case revealed a missense GTG → ATG mutation at codon 804 in exon 14 of the RET proto-oncogene by single-strand conformation polymorphism analysis and direct sequencing using an automated DNA sequencer (3130 Genetic Analyzer, Applied Biosystems, Foster City, CA, USA). This transversion leads to the substitution of valine with methionine (Fig. 2). At-risk family members were tested for exon 14. No other family members carried the V804M RET mutation (Fig. 3). Biochemical tests and thyroid US examinations were performed on family members. On thyroid US, the index patient's mother had multiple small nodules on her left thyroid gland (Fig. 1), but US-guided FNA cytology revealed benign. Laboratory findings including serum Ca, P, iPTH, and calcitonin were within normal limits in all family members.
Prior to obtaining samples, all individuals included in the study were fully informed about the genetic study and consent was obtained.
Clear associations between RET mutation genotype and phenotype have been reported in hereditary MTCs. MEN 2A is caused by mutations affecting cysteine residues in codons 609, 611, 618, and 620 within exon 10 and codon 634 in exon 11 of RET (6). In MEN 2B, the mutation in codon 918 in exon 16 is present in over 95% of patients, while codon 883 in exon 15 of RET is present in 2%-3% of patients (6). Rarely, patients with MEN 2B have double RET mutations including V804M and V805K, V804M, and Y806C (7, 8). FMTC is most commonly associated with mutations in codons 609, 611, 618, and 620 in exon 10, codon 768 in exon 13, and codon 804 in exon 14 (6).
Thus far, mutations at the 804 codon have been reported in less than 2% of cases (6, 9). Two types of codon 804 RET mutations have been reported, V804L and V804M. Phenotypes associated with the V804M RET mutation have been reported almost exclusively in FMTC. Only several cases of V804M mutations associated with MEN 2A (MTC plus hyperparathyroidism) have been reported in the literature (10-12).
FMTC is now viewed as a phenotypic variant of MEN 2A, with decreased penetrance for pheochromocytoma and primary hyperparathyroidism, rather than as a distinct entity (13). The most rigid definition of FMTC is multigenerational transmission of MTC in which no family member has either pheochromocytoma or primary hyperparathyroidism (14). A less rigid definition is the presence of MTC in four affected family members without other manifestations of MEN 2A (7). Therefore, a family with a small number of MTC-affected individuals who appear to have FMTC could mask the eventual identification of pheochromocytoma (15). We initially suspected our case to be FMTC because he had MTC with a germline mutation but without manifestations of MEN 2A. However, there were no germline mutations in other members of his family. Therefore, our case was a de novo V804M RET mutation carrier.
The American Thyroid Association (ATA) guidelines stratify all known RET mutations into one of four risk levels (ATA risk levels A-D) (13). ATA level D mutations carry the highest risk for MTC and ATA level A mutations carry the "least high" risk. ATA-A mutations include RET gene mutations at codons 768, 790, 791, 804, and 891 (13). Despite the ATA categorization into four levels (A-D), differences in the development and behavior of MTC and the development of MEN 2A features are present between RET mutations even within the same ATA level (16). Some researchers have reported that V804L or V804M mutations have more aggressive potential (17, 18). Our patient was already 33 yr of age and had developed microcarcinoma without lymph node metastasis; therefore, this case does not appear to have aggressive potential.
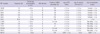
ATA recommends that all patients with personal medical histories of primary C cell hyperplasia, MTC, or MEN 2 should be offered germline RET testing (13). Once a germline RET mutation has been identified in a family, RET mutation analysis should be offered to all first-degree relatives of known mutation carriers before the age of recommended prophylactic thyroidectomy whenever possible (13). Clinical implications, ATA risk level and prophylactic thyroidectomy testing and therapy according to the genotype of RET mutations are summarized in Table 1.
Most laboratories evaluate patients for mutations in the five most commonly mutated codons in exons 10 and 11 (C634R, C609, C611, C618, and C620) (6) and additionally sequence exons 13, 14, 15, and/or 16. Some laboratories use a two-tiered approach to the analysis, starting with sequence analysis of the most commonly mutated "hotspot" exons and, at the request of the ordering physician, sequence the remaining exons of RET if the initial analysis is negative (19). Tiered approaches risk failure to detect rare double mutations. For example, there are a few reports suggesting that codon 804 mutations in conjunction with a second variant in RET are associated with FMTC (20) and MEN 2B (7, 8). We performed a full sequencing analysis of RET proto-oncogene mutations for exon 10, 11, 13, 14, 15, and 16 on the index patient. No double RET mutation was noticed in index patient.
The prevalence of V804M is very high among the residents of Sardinia, an Italian island. Pinna et al. (10) reported the prevalence of V804M in up to 48% of index cases (3/7 families) and 59% of overall family members (17/19 relatives) in Sardinia, possibly as a consequence of founder effect in this population. Shifrin et al. (12) also reported 107 members of an Italian family (origin from Florence/Calabria) with RET V804M proto-oncogene mutations. With exception of Italian, RET V804M protooncogene mutations are very rare in other races. In Asia, only one case of V804M and Y806C in the same allele in patient with MEN 2B was reported (8). However, V804M RET mutations have not been previously reported in Korea. Our case is the first in Korea, and represents a de novo V804M RET mutation.
Figures and Tables
Fig. 1
Transverse ultrasound image of thyroid nodules. (A) Ultrasound showing 0.6 cm nodule in index patient and (B) multiple 0.5 cm sized nodules in the index patient's mother.

Fig. 2
Direct sequence analysis of exon 14 of the RET gene. Genetic analysis of the index case revealed a missense GTG→ATG mutation at codon 804 in exon 14 of the RET proto-oncogene.

Fig. 3
Pedigree of the family showing the affected member (index patient). Circles and squares denote female and male family members, respectively.

References
1. Marsh DJ, Learoyd DL, Robinson BG. Medullary thyroid carcinoma: recent advances and management update. Thyroid. 1995. 5:407–424.
2. Pazaitou-Panayiotou K, Giatzakis C, Koutsodontis G, Vratimos A, Chrisoulidou A, Konstantinidis T, Kamakari S. Identification of two novel mutations in the RET proto-oncogene in the same family. Thyroid. 2010. 20:401–406.
3. Jung J, Uchino S, Lee Y, Park H. A Korean family of familial medullary thyroid cancer with Cys618Ser RET germline mutation. J Korean Med Sci. 2010. 25:226–229.
4. Chung YJ, Kim HH, Kim HJ, Min YK, Lee MS, Lee MK, Kim KW, Ki CS, Kim JW, Chung JH. RET proto-oncogene mutations are restricted to codon 634 and 618 in Korean families with multiple endocrine neoplasia 2A. Thyroid. 2004. 14:813–818.
5. Kim YK, Kim JW, Ahn SM, Song KE, Jung SH, Kim DJ, Chung YS, Lee KW, Kim CH, Hong JH, et al. A case of familial medullary thyroid carcinoma with a E768D mutation in RET proto-oncogene. J Korean Soc Endocrinol. 2005. 20:375–380.
6. Eng C, Clayton D, Schuffenecker I, Lenoir G, Cote G, Gagel RF, van Amstel HK, Lips CJ, Nishisho I, Takai SI, et al. The relationship between specific RET proto-oncogene mutations and disease phenotype in multiple endocrine neoplasia type 2. International RET mutation consortium analysis. JAMA. 1996. 276:1575–1579.
7. Cranston AN, Carniti C, Oakhill K, Radzio-Andzelm E, Stone EA, Mc-Callion AS, Hodgson S, Clarke S, Mondellini P, Leyland J, et al. RET is constitutively activated by novel tandem mutations that alter the active site resulting in multiple endocrine neoplasia type 2B. Cancer Res. 2006. 66:10179–10187.
8. Miyauchi A, Futami H, Hai N, Yokozawa T, Kuma K, Aoki N, Kosugi S, Sugano K, Yamaguchi K. Two germline missense mutations at codons 804 and 806 of the RET proto-oncogene in the same allele in a patient with multiple endocrine neoplasia type 2B without codon 918 mutation. Jpn J Cancer Res. 1999. 90:1–5.
9. Machens A, Niccoli-Sire P, Hoegel J, Frank-Raue K, van Vroonhoven TJ, Roeher HD, Wahl RA, Lamesch P, Raue F, Conte-Devolx B, et al. Early malignant progression of hereditary medullary thyroid cancer. N Engl J Med. 2003. 349:1517–1525.
10. Pinna G, Orgiana G, Riola A, Ghiani M, Lai ML, Carcassi C, Mariotti S. RET proto-oncogene in Sardinia: V804M is the most frequent mutation and may be associated with FMTC/MEN-2A phenotype. Thyroid. 2007. 17:101–104.
11. Gibelin H, Bezieau S, Misso C, Bouin-Pineau MH, Marechaud R, Kraimps JL. Germline RET V804M mutation associated with multiple endocrine neoplasia type 2A. Br J Surg. 2004. 91:1458–1459.
12. Shifrin AL, Xenachis C, Fay A, Matulewicz TJ, Kuo YH, Vernick JJ. One hundred and seven family members with the rearranged during transfection V804M proto-oncogene mutation presenting with simultaneous medullary and papillary thyroid carcinomas, rare primary hyperparathyroidism, and no pheochromocytomas: is this a new syndrome-MEN 2C? Surgery. 2009. 146:998–1005.
13. Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, Gharib H, Moley JF, Pacini F, Ringel MD, Schlumberger M, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid. 2009. 19:565–612.
14. Iihara M, Yamashita T, Okamoto T, Kanbe M, Yamazaki K, Egawa S, Yamaguchi K, Obara T. A nationwide clinical survey of patients with multiple endocrine neoplasia type 2 and familial medullary thyroid carcinoma in Japan. Jpn J Clin Oncol. 1997. 27:128–134.
15. Moers AM, Landsvater RM, Schaap C, Jansen-Schillhorn van Veen JM, de Valk IA, Blijham GH, Hoppener JW, Vroom TM, van Amstel HK, Lips CJ. Familial medullary thyroid carcinoma: not a distinct entity? Genotype-phenotype correlation in a large family. Am J Med. 1996. 101:635–641.
16. Frank-Raue K, Machens A, Scheuba C, Niederle B, Dralle H, Raue F. Difference in development of medullary thyroid carcinoma among carriers of RET mutations in codons 790 and 791. Clin Endocrinol (Oxf). 2008. 69:259–263.
17. Fattoruso O, Quadro L, Libroia A, Verga U, Lupoli G, Cascone E, Colantuoni V. A GTG to ATG novel point mutation at codon 804 in exon 14 of the RET proto-oncogene in two families affected by familial medullary thyroid carcinoma. Hum Mutat. 1998. Suppl 1. S167–S171.
18. Feldman GL, Edmonds MW, Ainsworth PJ, Schuffenecker I, Lenoir GM, Saxe AW, Talpos GB, Roberson J, Petrucelli N, Jackson CE. Variable expressivity of familial medullary thyroid carcinoma (FMTC) due to a RET V804M (GTG-->ATG) mutation. Surgery. 2000. 128:93–98.
19. Kaldrymides P, Mytakidis N, Anagnostopoulos T, Vassiliou M, Tertipi A, Zahariou M, Rampias T, Koutsodontis G, Konstantopoulou I, Ladopoulou A, et al. A rare RET gene exon 8 mutation is found in two Greek kindreds with familial medullary thyroid carcinoma: implications for screening. Clin Endocrinol (Oxf). 2006. 64:561–566.
20. Jhiang SM. The RET proto-oncogene in human cancers. Oncogene. 2000. 19:5590–5597.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download