Abstract
Osteopontin (OPN) is an acidic, noncollagenous matrix protein produced by the bone and kidneys. It is reportedly involved in bone resorption and formation. We examined the association between serum OPN levels and bone mineral density in postmenopausal women. Premenopausal women (n=32) and postmenopausal women (n=409) participated in the study. We measured serum osteopontin levels and their relationships with bone mineral density and previous total fragility fractures. The postmenopausal women had higher mean serum OPN levels compared to the premenopausal women (43.6±25.9 vs 26.3±18.6 ng/mL; P<0.001). In the postmenopausal women, high serum OPN levels were negatively correlated with mean lumbar bone mineral density (BMD) (r=-0.113, P=0.023). In a stepwise multiple linear regression model, serum OPN levels were associated with BMD of the spine, femoral neck, and total hip after adjustment for age, body mass index, smoking, and physical activity in postmenopausal women. However, serum OPN levels did not differ between postmenopausal women with and without fractures. Postmenopausal women exhibit higher serum OPN levels than premenopausal women and higher serum OPN levels were associated with low BMD in postmenopausal women.
Osteopontin (OPN) is an acidic, noncollagenous matrix protein produced by the bone and kidneys. Plasma osteopontin levels are elevated in many pathologic conditions, including cancer (1, 2), autoimmune disease, obesity (3, 4), and cardiovascular disease (5). OPN is reportedly involved in bone resorption and bone formation (6, 7). OPN -/- mice show resistance to ovariectomy-induced bone resorption compared to wild-type mice (-60% vs -10% reduction in bone volume, respectively), suggesting the pivotal role of OPN in postmenopausal osteoporosis (8). We examined the association between serum OPN levels and bone mineral density in postmenopausal Korean women.
This study was performed from June 2009 to October 2010 in Kangwon National University Hospital. A total of 441 healthy female volunteers over the age of 50 yr satisfied the inclusion criteria. Menopause was defined as the absence of menstruation for at least 1 yr. Excluded from this study were women taking glucocorticoids and estrogen for more than 3 months prior or women with diseases that could affect bone metabolism, such as Graves' disease or Cushing's syndrome. Hysterectomized women and premenopausal bilaterally ovariectomized women were also excluded.
A self-administered questionnaire, interviews, and anthropometric measurements were used to collect data on lifestyle, physical activity, and previous medical and fracture histories. Previous fragility fractures were low-trauma fractures involving femur, spine, and other sites such as wrist, ankle, foot, ribs and others. Smoking status was categorized as non-smoker, ex-smoker, and smoker. Daily physical activity (walking or cycling) was measured using the responses to the questionnaire ("How much time do you usually spend walking or on a bicycle outdoors each day?") Possible response included none, less than 30 min, 30 min to 1 hr, or more than 1 hr.
Areal bone mineral density (BMD) (g/cm2) values were determined in the spine, femoral neck, and total hip in all subjects using a Lunar Prodigy Vision dual-emission X-ray absorptiometry system (Lunar Corp., Madison, WI, USA). According to the World Health Organization definition, osteoporosis was determined as a T-score of ≤ -2.5 standard deviations (SD) at any site. One investigator performed all densitometry tests and analyses in all subjects. The precision of the equipment, presented as coefficients of variation (CV), was 0.90 and 1.14% at Kangwon National University for the lumbar spine and the femoral neck, respectively in 20 volunteers at Kangwon National University who were not enrolled in the study.
Serum OPN levels were measured using the Quantikine Human OPN immunoassay kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer's instructions. Intraassay coefficient of variation (CV) was 4% and inter-assay CV was 6.6%.
Pearson correlation coefficients were calculated to analyze the relationship between serum OPN levels and clinical parameters, including BMD. Student's t-tests or the chi-square test was used to compare baseline characteristics between premenopausal and postmenopausal women. Linear regression was used to investigate the association between serum OPN levels and BMD, adjusting for age, body mass index (BMI), smoking, and physical activity. A multiple logistic regression analysis with the stepwise forward method was used to evaluate independent variables. The history of fragility fractures was set as the dependent variable. A P value of < 0.05 was considered to be statistically significant.
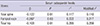
This study included 409 postmenopausal women with a mean age of 61.4 ± 7.8 yr and 32 premenopausal women with a mean age of 51.4 ± 1.9 yr. In postmenopausal women, the mean number of years after menopause was 11.4 ± 8.7. The postmenopausal group was about 10 yr older and had a higher systolic blood pressure compared to the premenopausal group. The postmenopausal women had higher mean serum OPN levels compared to the premenopausal women (43.6 ± 25.9 vs 26.3 ± 18.6 ng/mL; P < 0.001, Table 1). The BMD of the spine, femoral neck, and total hip was significantly lower and the total fracture history was significantly more frequent in postmenopausal women compared to premenopausal women.
We studied the correlation between serum OPN levels and age, BMI, systolic blood pressure, BMD of the spine, femoral neck, and total hip and other clinical parameters in pre- and postmenopausal women. However, Pearson correlations failed to show any correlation between serum OPN levels and clinical parameters with the exception of some BMD values in postmenopausal women. In the postmenopausal women, high serum OPN levels were negatively correlated with mean lumbar BMD (r = -0.113, P = 0.023).
In the multiple linear regression model with stepwise forward method, serum OPN levels were associated with BMD of the spine, femoral neck, and total hip (Table 2) after adjustment for age, BMI, smoking, and physical activity in postmenopausal women. However, in the premenopausal group, there was no association between serum OPN levels and BMD of the spine, femoral neck, and total hip in the multiple linear regression model with stepwise forward method.
Postmenopausal women with previous fragility fractures were older, had a lower BMI, had a longer number of years after menopause, and had a lower BMD of the spine, femoral neck, and total hip, compared to postmenopausal women without previous fragility fractures. However, serum OPN levels were not different between postmenopausal women with and without fractures.
Our study demonstrates that postmenopausal women have significantly higher levels of serum OPN compared to premenopausal women, and that in postmenopausal women, serum OPN levels are inversely associated with BMD of the spine, femoral neck, and total hip, implicating the physiologic role for OPN in postmenopausal bone loss.
OPN is a multifunctional protein that involves the regulation of inflammation, bone remodeling, and cell survival (9). OPN stimulates CD44 expression, thereby upregulating osteoclast motility and bone resorption (10). It plays a critical role in sympathetic control of bone mass through β2 adrenergic receptors/c AMP signaling (11). OPN -/- mice show resistance to ovariectomy-induced bone resorption compared to wild-type mice (-60% vs -10% reduction in bone volume, respectively)(8), suggesting the pivotal role of OPN in postmenopausal osteoporosis.
A previous study involving 124 postmenopausal women has shown that the serum OPN levels were a risk factor for menopausal osteoporosis and serum OPN levels were positively correlated with bone resorption marker such as carboxy-terminal collagen crosslinks (12). Our study reinforces the previous study with a larger sample size (n = 409 vs 124, respectively) in that high serum OPN levels were shown to be an independent risk factor for low BMD in postmenopausal women. Our study investigated the relationship between serum OPN levels and total fragility fractures, although there was no association between them in postmenopausal women. In the previous study, there was a correlation between serum OPN levels and age or body weight, but our data failed to show a correlation between serum OPN levels and age or BMI. In another study showed that the high serum levels of OPN were associated with low BMD and increased levels of bone turnover markers and that postmenopausal women with osteoporotic vertebral fractures had significantly higher levels of OPN than those without vertebral fractures (13). Our study differs from two previous studies (12, 13) in that we studied the association between the serum OPN levels and total fragility fractures. One of possible reason of lack of relationship in our study was that there were very low prevalence of spine or hip fractures (0.7%-1.0%) in total fragility fractures. Therefore, the potential of serum OPN levels to predict major osteoporotic fractures remains open to debate.
In the previous study (12), the mean serum OPN levels (15.4 ± 6.2 ng/mL) were relatively low compared to our data and other previous data (14). Commercial ELISA kits are available to determine plasma or serum OPN levels. The reason of serum mean OPN differences between human studies were not clear. The results of circulating OPN levels may be variable depending on the type of sample (plasma vs serum), ages, races, detection method, and choice of ELISA kit (12, 15).
The baseline rise in circulating OPN levels was associated with coronary artery disease with rapid plaque progression (16), asthma (14, 17), and cancer aggressiveness and poor survival (2) in humans. Our data demonstrate that high serum OPN levels were associated with osteoporosis, especially in postmenopausal women, suggesting the role of OPN in bone remodeling.
Our study has some limitations. This was a cross-sectional study, not a prospective study. The postmenopausal status was self-reported. In addition, our study did not involve measurement of bone turnover markers or bone quality.
Further investigation is definitely warranted to unravel the potential role of OPN in large-scale and long-term prospective cohort studies to arrive at a conclusion about the causal relationship between serum OPN and bone mineral density or fracture in postmenopausal women.
In conclusion, our study shows that postmenopausal women have higher serum OPN levels than premenopausal women and that higher serum OPN levels are associated with low BMD in postmenopausal women.
ACKNOWLEDGEMENTS
The biospecimens for this study were provided by the Kangwon National University Hospital Biobank, a member of the National Biobank of Korea, which is supported by the Ministry of Health, Welfare and Family Affairs. All samples derived from the National Biobank of Korea were obtained with informed consent under institutional review board-approved protocols.
References
1. Chang YS, Kim HJ, Chang J, Ahn CM, Kim SK, Kim SK. Elevated circulating level of osteopontin is associated with advanced disease state of non-small cell lung cancer. Lung Cancer. 2007; 57:373–380.
2. Weber GF, Lett GS, Haubein NC. Osteopontin is a marker for cancer aggressiveness and patient survival. Br J Cancer. 2010; 103:861–869.
3. Gómez-Ambrosi J, Catalán V, Ramírez B, Rodríguez A, Colina I, Silva C, Rotellar F, Mugueta C, Gil MJ, Cienfuegos JA, et al. Plasma osteopontin levels and expression in adipose tissue are increased in obesity. J Clin Endocrinol Metab. 2007; 92:3719–3727.
4. Nomiyama T, Perez-Tilve D, Ogawa D, Gizard F, Zhao Y, Heywood EB, Jones KL, Kawamori R, Cassis LA, Tschöp MH, et al. Osteopontin mediates obesity-induced adipose tissue macrophage infiltration and insulin resistance in mice. J Clin Invest. 2007; 117:2877–2888.
5. Scatena M, Liaw L, Giachelli CM. Osteopontin: a multifunctional molecule regulating chronic inflammation and vascular disease. Arterioscler Thromb Vasc Biol. 2007; 27:2302–2309.
6. Ishijima M, Ezura Y, Tsuji K, Rittling SR, Kurosawa H, Denhardt DT, Emi M, Nifuji A, Noda M. Osteopontin is associated with nuclear factor kappaB gene expression during tail-suspension-induced bone loss. Exp Cell Res. 2006; 312:3075–3083.
7. Ishijima M, Rittling SR, Yamashita T, Tsuji K, Kurosawa H, Nifuji A, Denhardt DT, Noda M. Enhancement of osteoclastic bone resorption and suppression of osteoblastic bone formation in response to reduced mechanical stress do not occur in the absence of osteopontin. J Exp Med. 2001; 193:399–404.
8. Yoshitake H, Rittling SR, Denhardt DT, Noda M. Osteopontin-deficient mice are resistant to ovariectomy-induced bone resorption. Proc Natl Acad Sci U S A. 1999; 96:8156–8160.
9. Denhardt DT, Noda M, O'Regan AW, Pavlin D, Berman JS. Osteopontin as a means to cope with environmental insults: regulation of inflammation, tissue remodeling, and cell survival. J Clin Invest. 2001; 107:1055–1061.
10. Chellaiah MA, Kizer N, Biswas R, Alvarez U, Strauss-Schoenberger J, Rifas L, Rittling SR, Denhardt DT, Hruska KA. Osteopontin deficiency produces osteoclast dysfunction due to reduced CD44 surface expression. Mol Biol Cell. 2003; 14:173–189.
11. Nagao M, Feinstein TN, Ezura Y, Hayata T, Notomi T, Saita Y, Hanyu R, Hemmi H, Izu Y, Takeda S, et al. Sympathetic control of bone mass regulated by osteopontin. Proc Natl Acad Sci U S A. 2011; 108:17767–17772.
12. Chang IC, Chiang TI, Yeh KT, Lee H, Cheng YW. Increased serum osteopontin is a risk factor for osteoporosis in menopausal women. Osteoporos Int. 2010; 21:1401–1409.
13. Fodor D, Bondor C, Albu A, Simon SP, Craciun A, Muntean L. The value of osteopontin in the assessment of bone mineral density status in postmenopausal women. J Investig Med. 2013; 61:15–21.
14. Zhao JJ, Yang L, Zhao FQ, Shi SM, Tan P. Osteopontin levels are elevated in patients with asthma. J Int Med Res. 2011; 39:1402–1407.
15. Constantinescu D, Vornicu M, Grigoriu C, Cozmei C, Grigoriu BD. Assaying for circulating osteopontin in practice: a technical note. Eur Respir J. 2010; 35:1187–1188.
16. Mazzone A, Parri MS, Giannessi D, Ravani M, Vaghetti M, Altieri P, Casalino L, Maltinti M, Balbi M, Barsotti A, et al. Osteopontin plasma levels and accelerated atherosclerosis in patients with CAD undergoing PCI: a prospective clinical study. Coron Artery Dis. 2011; 22:179–187.
17. Samitas K, Zervas E, Vittorakis S, Semitekolou M, Alissafi T, Bossios A, Gogos H, Economidou E, Lötvall J, Xanthou G, et al. Osteopontin expression and relation to disease severity in human asthma. Eur Respir J. 2011; 37:331–341.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download