Abstract
This study aimed to investigate the status of primary liver cancers found through a routine health check-up. The data of subjects who were diagnosed with primary liver cancer for the first time through a routine health check-up during a period of 8-yr were analyzed. Primary liver cancers were detected for the first time in 34 subjects among 91,219 routine health check-up subjects. Only 11.8% of primary liver cancer subjects had been under previous surveillance. Of them, 55.8% were positive for HBsAg, 17.7% were positive for anti-HCV, and 8.8% were heavy alcohol comsumers. However, 17.7% of the subjects were neither heavy alcohol consumers nor positive for both HBsAg and anti-HCV. Of the subjects, 50.0% had a single nodular tumor, 23.5% had multi-nodular tumors, and 26.5% had an infiltrative tumor. A routine health check-up may provide beneficial opportunities to detect a liver cancer in a very early stage. It is beneficial to start surveillance in high-risk subjects for liver cancer or to detect any liver cancer in subjects without risk factors of chronic viral hepatitis or heavy alcohol consumption.
According to many guidelines, surveillance for liver cancer is strongly recommended in high risk subjects to improve prognosis by early diagnosis (1-4). Hepatitis B virus (HBV) infection, hepatitis C virus (HCV) infection and heavy alcohol consumption are representative risk factors for liver cancer (3). As Korea has been an endemic area of HBV, liver cancer also has been a major public health problem in Korea (5). Actually in 2011, liver cancer was ranked as the second most common cause of cancer mortality in Korea (6). Therefore, surveillance for liver cancer in high-risk subjects for liver cancer may be important in view of improving not only personal health but also public health in Korea (5, 7). Since 2001, in order to reduce the clinical burden of liver cancer through early diagnosis and treatment, the Ministry of Health and Welfare, Republic of Korea Government has recommended the regular surveillance of subjects older than 40 yr who are at a high risk for liver cancer (8).
Routine health check-ups are performed on people in Korea for the purpose of primary prevention or secondary prevention of major public health problems such as cancers or cardiovascular disease. Therefore, a routine health check-up may be a good chance not only to perform essential surveillance activities but also to detect liver cancer in the early stage. The purpose of this study was to study the characteristics of liver cancers found during routine health check-ups and their previous surveillance status in one health check-up specialized center which exists as a part of a major tertiary hospital in Korea.
A total of 91,219 subjects (48,122 males and 43,097 females) received a routine health check-up which included abdominal ultrasonography (USG) or computed tomography (CT) at the Seoul National University Hospital Healthcare System Gangnam Center (Seoul, Korea) between October, 2003 and August, 2011. Among these 91,219 subjects, those who were diagnosed with liver cancer were extracted for this study. After excluding the 17 subjects with a previous history of liver cancer, the subjects who were diagnosed with liver cancer for the first time during a routine health check-up or during a surveillance which had started after a routine health check-up were the final subjects for this study.
Each subject answered a questionnaire, underwent anthropometric assessment, and had laboratory tests and a radiologic study of abdominal USG or CT done on the same health check-up day. Data about age, gender, cigarette smoking, amount of alcohol intake, family history of cancer, and general symptoms about weakness, weight loss or dyspepsia were collected from the questionnaire. Body mass index (BMI) was calculated by dividing the weight in kilograms by square of the height in meters. Laboratory tests included serum hepatitis B surface antigen (HBsAg), an antibody to hepatitis C virus (anti-HCV) and alpha-fetoprotein (αFP). Blood samples were collected from each subject before 10 a.m. after an overnight fast. All biochemical analyses of blood samples were performed in the same quality-controlled laboratory and done according to standard laboratory methods. Abdominal magnetic resonance imaging (MRI) or USG guided liver biopsy were performed on a separate day if needed diagnostically. A heavy alcohol consumer was defined as a person who consumed more than 80 g of alcohol per drinking session and drank more than 5 times a week for more than 10 yr (9). All USG, CT and MRI were assessed by radiologists. Liver cirrhosis was assessed by surface nodularities of a liver, regenerating nodules in a liver and/or an accompained hypersplenism. Liver cancer was diagnosed according to the Practice Guidelines for Management of Hepatocellular Carcinoma (2009) (10). Nodular tumor was divided into single nodular or multinodular type by the number of tumor nodules. Infiltrative tumor was diagnosed if more than 50% of a tumor margin showed infiltrative and irregular invasion into adjacent liver tissues. Primary liver cancer found during a routine health check-up was treated by surgery, percutaneous ethanol injection, radiofrequency ablation or transarterial chemoembolization at the main tertiary Seoul National University Hospital (11-13).
The data were expressed as the mean ± standard deviation. However, for data which did not follow standard normal distribution, data were expressed as median and range. Intergroup differences in continuous variables were explored by using Kruskal-Wallis test or Student's t-test. Intergroup differences in frequency variables were explored by chi-square test or Fisher's exact test. SAS 9.2 version (SAS Institute, Cary, NC, USA) was used for the statistical analysis. A two-tailed P value that was less than 0.05 was regarded to be statistically significant.
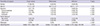
A total of 34 subjects were diagnosed with primary liver cancer for the first time through a routine health check-up during a period of 8 yr. Only 11.8% of liver cancer subjects had been under previous surveillance (Table 1). Of the liver cancers, 82.4% were detected at a health check-up, and 17.6% were detected by surveillance which had been started after the initial health check-up. Liver cirrhosis was found in 76.5% of the liver cancer subjects. HBsAg was the most commonly found underlying risk factor for liver cancer in our study (55.8%), followed by anti-HCV (17.7%) and heavy alcohol consumption (8.8%). However, 17.7% of the liver cancer subjects did not have any evidence of HBsAg, anti-HCV or heavy alcohol consumption. Mean age was significantly younger in subjects with HBsAg than in those without HBsAg (P = 0.028). Male was about 6 times more common than female. Of the liver cancer subjects, 47.1% had diabetes, and 64.7% were current smokers. Family history of liver cancer was positive in 21.1% of subjects with HBsAg and 16.7% of subjects with anti-HCV. Among 34 liver cancers, 1 intrahepatic cholangiocarcinoma was confirmed by biopsy in a subject with HBV.
Gross tumor type was significantly different between subjects with HBsAg and those with anti-HCV (Fig. 1). Nodular tumor was more common than infiltrative tumor in subjects with HBsAg, but infiltrative tumor was more common in subjects with anti-HCV. General weakness, weight loss or dyspepsia was significantly more common in subjects with infiltrative tumor than in those with nodular tumor (Table 2). Serum αFP level was significantly higher in subjects with infiltrative tumor than in those with nodular tumor. Metastasis was observed only in 5 subjects with infiltrative tumor, 4 lung metastasis and 1 lymph node metastasis. Surgery was the most common method of treatment for single nodular liver cancer, but transarterial chemoembolization was used for multinodular or infiltrative liver cancer (Fig. 2).
Our study showed that a low proportion of the liver cancer subjects had been under previous surveillance for primary liver cancer. Moreover, even though HBV is the most common risk factor in Korea, only 5.3% of HBV positive liver cancer subjects were under surveillance. This result may suggest that the actual surveillance rate may be low in spite of the recommendations by the Korean government since 2001 that regular surveillance of high risk subjects for liver cancer who are older than 40 yr be performed (8). As regular surveillance can improve the morbidity and prognosis of liver cancer, more efforts to enroll subjects at high risk for liver cancer into regular surveillance programs may be needed (14).
A routine health check-up may provide a good chance to detect liver cancer and start surveillance for liver cancer. In our study, 82.4% of the liver cancers were found during a health check-up and 17.6% of the liver cancers were found by surveillance which had been started after a health check-up because the HBsAg or anti-HCV was found to be positive.
In regards to the major risk factor for liver cancer found in our study, HBsAg was the most common factor, followed by anti-HCV and heavy alcohol consumption. The proportion of HbsAg-positive subjects was similar to the previously reported worldwide proportion of 50%-55%, but the proportion of anti-HCV positive subjects was less than the previously reported worldwide proportion of 25%-30% (15). The proportion of anti-HCV in liver cancer subjects in Korea may not have changed for 20 yr when comparing the present data to that (17.0%) published 20 yr ago (16). Considering the previous report that HCV-related hepatocellular carcinoma represents 70% of all primary liver cancers in Japan, the underlying cause of primary liver cancer can vary quite considerably among geographically near countries such as Japan and Korea (16, 17). The liver cancer was accompanied by liver cirrhosis in 76.5% of the subjects with liver cancer, which was a rate similar to the 73.3% figure quoted in a previous report in Korea (18). Of the liver cancer subjects, 64.7% were current smokers in our study. As smoking is known to increase the risk of liver cancer, smoking might contribute to the development of liver cancers (19). In our study, 47.1% of the subjects had diabetes. As diabetes is also recognized as a predisposing factor for liver cancer, diabetes might also have contributed to the development of liver cancer in our subjects (20-22). Our subjects' mean BMI was 24.9 ± 3.5, which was near 25, the cutoff value for being overweight (23). Adequate weight control may be needed in subjects with risk factors for liver cancer because obesity has been shown to have an association with liver cancer (24, 25).
The proportion of subjects without HBsAg, anti-HCV, and heavy alcohol consumption was 17.7%, which is comparable to the figure of 17.6% published 20 yr ago in Korea but is slightly higher than that of 8%-15% in Japan (16, 17). These results suggest that any liver mass found by chance at USG or CT should be thoroughly evaluated even in a subject without positive test results for HBV or HCV, or who does not have heavy alcohol consumption. Among subjects without HBsAg, anti-HCV, and heavy alcohol consumption, 83.3% were smokers and 16.7% were obese in our study. Nonalcoholic steatohepatitis was found in 10% of liver cancer subjects without HBV and HCV in Japan (17). Smoking, nonalcoholic steatohepatitis, aflatoxin or other carcinogenic causes may also be an associated underlying risk factor in these subjects without HBsAg, anti-HCV, or heavy alcohol consumption (26).
Male sex was 5.8 times more common than female in our study. This male predominance coincides with the finding in previous reports (3). Mean age was 59.0 ± 10.1 yr. Mean ages were significantly different according to associated risk factors for liver cancer. Mean age of subjects with HBsAg was 54.5 ± 8.5 yr but that of subjects with anti-HCV was 64.3 ± 10.9 yr, which also coincides with the findings in a previous report (16). Proportion of intrahepatic cholangiocarcinoma may be comparable to a previous study in Japan that reported 95% of primary liver cancers were hepatocellular carcinoma (17).
The general symptoms of weakness, fatigue or dyspepsia were more frequently found in subjects with infiltrative tumor than in those with nodular tumor in our study. Newly occurring general symptoms of weakness, fatigue or dyspepsia in a high-risk subject for liver cancer may need attention because these symptoms may come from a newly developed liver cancer (18).
αFP level was higher in subjects with infiltrative liver cancer than in those with nodular liver cancer. This finding is in concordance with the previous report that αFP reflects tumor activity in hepatocellular carcinoma (27).
A routine health check-up may be a good opportunity to detect liver cancer in an early stage. Single nodular liver cancer was found in 50% of the subjects in our study. On the other hand, the proportion of single nodular cancer among all liver cancers detected was previously reported to be 32.0% and 37.3% in each of two different tertiary hospitals in Korea (18, 28). The reason for this difference in the proportion of single nodular cancer may have two possibilities. First, liver cancers detected at tertiary hospitals were found in subjects with already known high-risk factors for liver cancer by surveillance. Second, liver cancers detected in a routine health check-up are found at a very early stage and this phenomenon may reflect the real effect of screening for liver cancer in a primary care setting. This may be important because detecting a liver cancer in an early or at a single nodule stage can lead to curative treatment. Surgical resection or local ablative therapy has been regarded as a curative therapy (29). A total of 44.0% of our liver cancer subjects received curative therapy: 26.5% of subjects received surgical resection and 17.6% of subjects received local ablative therapy. This may be higher than the 12.4% of subjects who were reported to be curatively treated in a previous report (18). Moreover, considering that transarterial chemoembolization can be a curative treatment if the embolization is compact, the actual proportion of subjects who received curative therapy may be higher than 44.0% in our study (30). Actually, 8.8% of our subjects who had single nodular liver cancer were completely treated by transarterial chemoembolization only or consecutive surgery.
Our study has the limitation of not representing the whole Korean population because the subjects in our study visited the center voluntarily for a routine health check-up. There may be some selection bias in our study because a person with high risks for liver cancer may get their liver evaluated in a liver-specific clinic than in a routine heath check-up center. Our study may also have the limitation of being a retrospective study.
In summary, a routine health check-up may provide 3 important opportunities for detection of liver cancer. The first is the opportunity to detect a liver cancer at a very early stage. The second is the opportunity to start surveillance in high-risk subjects for liver cancer. The third is the opportunity to detect a liver cancer in subjects without the representative risk factors of chronic viral hepatitis or heavy alcohol consumption.
Figures and Tables
Fig. 1
Differences in gross tumor type according to associated risk factors for primary liver cancer.

Notes
References
1. Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, et al. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010; 4:439–474.
2. European Association for the Study of the Liver. European Organisation for Research and treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943.
3. De Lope CR, Tremosini S, Forner A, Reig M, Bruix J. Management of HCC. J Hepatol. 2012; 56:S75–S87.
4. Bruix J, Sherman M. American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011; 53:1020–1022.
5. Bae SY, Choi MS, Gwak GY, Paik YH, Lee JH, Koh KC, Paik SW, Yoo BC. Comparison of usefulness of clinical diagnostic criteria for hepatocellular carcinoma in a hepatitis B endemic area. Clin Mol Hepatol. 2012; 18:185–194.
6. Statistics Korea. Korean Statistical Information Service by Statistics Korea. accessed on 10 April 2013. Available at http://kosis.kr/abroad/abroad_01List.jsp?parentId=D.
7. Song IH, Kim KS. Current status of liver diseases in Korea: hepatocellular carcinoma. Korean J Hepatol. 2009; 15:S50–S59.
8. National cancer control programs in Korea. J Korean Med Sci. 2007; 22:S3–S4.
9. Lee JJ, Park SK, Kwon OS, Won IS, Kim DK, Jung YK, Ku YS, Kim YS, Choi DJ, Kim JH. Genetic polymorphism at codon 10 of the transforming growth factor-beta1 gene in patients with alcoholic liver cirrhosis. Korean J Hepatol. 2011; 17:37–43.
10. Korean Liver Cancer Study Group and National Cancer Center, Korea. Practice guidelines for management of hepatocellular carcinoma 2009. Korean J Hepatol. 2009; 15:391–423.
11. Lee J, Lee JM, Yoon JH, Lee JY, Kim SH, Lee JE, Han JK, Choi BI. Percutaneous radiofrequency ablation with multiple electrodes for medium-sized hepatocellular carcinomas. Korean J Radiol. 2012; 13:34–43.
12. Jang ES, Yoon JH, Chung JW, Cho EJ, Yu SJ, Lee JH, Kim YJ, Lee HS, Kim CY. Survival of infiltrative hepatocellular carcinoma patients with preserved hepatic function after treatment with transarterial chemoembolization. J Cancer Res Clin Oncol. 2013; 139:635–643.
13. Cho YB, Lee KU, Suh KS, Kim YJ, Yoon JH, Lee HS, Hahn S, Park BJ. Hepatic resection compared to percutaneous ethanol injection for small hepatocellular carcinoma using propensity score matching. J Gastroenterol Hepatol. 2007; 22:1643–1649.
14. Stravitz RT, Heuman DM, Chand N, Sterling RK, Shiffman ML, Luketic VA, Sanyal AJ, Habib A, Mihas AA, Giles HC, et al. Surveillance for hepatocellular carcinoma in patients with cirrhosis improves outcome. Am J Med. 2008; 121:119–126.
15. Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004; 127:S5–S16.
16. Lee HS, Han CJ, Kim CY. Predominant etiologic association of hepatitis C virus with hepatocellular carcinoma compared with hepatitis B virus in elderly patients in a hepatitis B-endemic area. Cancer. 1993; 72:2564–2567.
17. Umemura T, Ichijo T, Yoshizawa K, Tanaka E, Kiyosawa K. Epidemiology of hepatocellular carcinoma in Japan. J Gastroenterol. 2009; 44:102–107.
18. Jung SH, Kim BH, Joung YH, Han YS, Lee BH, Dong SH, Kim HJ, Chang YW, Lee JI, Chang R. Clinical features of hepatocellular carcinoma in the 1990s. Korean J Gastroenterol. 2003; 42:322–329.
19. Purohit V, Rapaka R, Kwon OS, Song BJ. Roles of alcohol and tobacco exposure in the development of hepatocellular carcinoma. Life Sci. 2013; 92:3–9.
20. Arase Y, Kobayashi M, Suzuki F, Suzuki Y, Kawamura Y, Akuta N, Kobayashi M, Sezaki H, Saito S, Hosaka T, et al. Effect of type 2 diabetes on risk for malignancies includes hepatocellular carcinoma in chronic hepatitis C. Hepatology. 2013; 57:964–973.
21. Wang P, Kang D, Cao W, Wang Y, Liu Z. Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev. 2012; 28:109–122.
22. Wang C, Wang X, Gong G, Ben Q, Qiu W, Chen Y, Li G, Wang L. Increased risk of hepatocellular carcinoma in patients with diabetes mellitus: a systematic review and meta-analysis of cohort studies. Int J Cancer. 2012; 130:1639–1648.
23. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309:71–82.
24. Schlesinger S, Aleksandrova K, Pischon T, Fedirko V, Jenab M, Trepo E, Boffetta P, Dahm CC, Overvad K, Tjønneland A, et al. Abdominal obesity, weight gain during adulthood and risk of liver and biliary tract cancer in a European cohort. Int J Cancer. 2013; 132:645–657.
25. Tanaka K, Tsuji I, Tamakoshi A, Matsuo K, Ito H, Wakai K, Nagata C, Mizoue T, Sasazuki S, Inoue M, et al. Obesity and liver cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol. 2012; 42:212–221.
26. Gouas D, Shi H, Hainaut P. The aflatoxin-induced TP53 mutation at codon 249 (R249S): biomarker of exposure, early detection and target for therapy. Cancer Lett. 2009; 286:29–37.
27. Sherman M. The resurrection of alphafetoprotein. J Hepatol. 2010; 52:939–940.
28. Park KW, Park JW, Choi JI, Kim TH, Kim SH, Park HS, Lee WJ, Park SJ, Hong EK, Kim CM. Survival analysis of 904 patients with hepatocellular carcinoma in a hepatitis B virus-endemic area. J Gastroenterol Hepatol. 2008; 23:467–473.
29. Oliveri RS, Wetterslev J, Gluud C. Hepatocellular carcinoma. Lancet. 2012; 380:470.
30. Chua TC, Liauw W, Saxena A, Chu F, Glenn D, Chai A, Morris DL. Systematic review of neoadjuvant transarterial chemoembolization for resectable hepatocellular carcinoma. Liver Int. 2010; 30:166–174.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download