Abstract
There are little information on prevalence of obstructive sleep apnea syndrome (OSAS) and clinical features in the young military population. The purpose of this study was to estimate the prevalence of snoring and high risk of OSAS in young male soldiers in Korea and to identify the risk factors of OSAS. A total of 665 participants (aged 20-23 yr) who visited the Armed Forces Ildong Hospital for regular physical examination were enrolled. All participants completed the Berlin Questionnaire and underwent a physical examination. The participants with high risk for OSAS completed portable sleep monitoring. The prevalence of snoring and high risk of OSAS in young male soldiers in Korea was 13.5% and 8.1%, respectively. The prevalence of high arched palate, tongue indentation, long uvula, large tonsil and retrognathia was significantly higher in the high risk OSAS group. High arched palate, long uvula or low lying soft palate, tonsil size III or IV, Epworth Sleepiness Scale score > 10 and obesity (BMI > 27 kg/m2) were found to independently predict OSAS. For early identification and treatment of young soldiers with OSAS in a military environment, a precise screening by questionnaire and physical examination is needed.
Snoring and sleep disordered breathing (SDB) are common among middle-aged adults and are characterized by repeated cessations of breathing during sleep. Obstructive sleep apnea syndrome (OSAS), the most common form of SDB, can cause serious adverse consequences including an increased risk of cardiovascular diseases and neurocognitive morbidities (1,2). In a large population study, the prevalence of SDB was 4% in men and 2% in woman (3).
Several reports showed that OSAS was associated with higher risks of traffic accidents and involvement in occupational accidents due to excessive daytime sleepiness (EDS) and cognitive impairment (4-6). Due to the nature of group accommodation in military environment, sleep deprivation can result in EDS for the patients with OSAS and persons sharing the same room. However, there are little information on prevalence of OSAS and clinical features in the military population. Therefore, it is necessary to determine the associated risk factors of OSAS in active duty military personnel for early diagnosis and treatment. The purpose of this study was to estimate the prevalence of snoring and high risk of OSAS in young male soldiers in Korea and identify the risk factors of OSAS.
A total of 665 participants aged 20 to 23 yr who went to the Armed Forces Il Dong Hospital for their regular physical examination were studied from July to September 2011. All participants completed the Korean version of the Berlin Questionnaire and Epworth Sleepiness Scale (ESS). They underwent otorhinolaryngologic evaluation by a specialist. Fifty participants who were identified as high-risk for OSAS by the Berlin Questionnaire completed portable sleep monitoring, Stardust II (Respironics Inc., Murraysville, PA, USA).
The questionnaire used to evaluate the risk of OSAS was the Korean version of the Berlin questionnaire. It has been previously validated in several surveys. The content of the Berlin questionnaire has been previously described in detail (7). Briefly, the questionnaire is divided into three sections. In section 1, respondents are asked whether they snore. Those who respond affirmatively are asked how loud the snoring is, how often it occurs, and whether their snoring bothers other people. Respondents are also asked whether anyone has ever noticed cessation of their breathing during sleep. In section 2, respondents are asked how often they feel tired or fatigued right after sleep, how often they feel tired, fatigued, or not up to par during wake time, and whether they ever fall asleep driving a car. In section 3, respondents are asked about a personal history of hypertension, as well as their height, weight, age, and sex. Body mass index (BMI) was calculated from the information in section 3. A section was considered positive if there were two affirmative answers in either section 1 or 2, or one affirmative response in section 3. Individuals who had positive scores in two of the three sections were considered to be at risk for OSAS. Daytime sleepiness was estimated using the Epworth sleepiness scale (8). Habitual snoring was defined as a snoring frequency ≥ 4 days per week.
A single otorhinolaryngologist performed all examinations. Tonsillar size and palatal position were classified into 4 grades according to Friedman's grade. The uvula was considered long if it was more than 1.5 cm in length. The soft palate was considered low lying if greater than one-third of the uvula extended below the level of the mandibular occlusal plane. Subjects were evaluated for tongue indentation by oral cavity examination. The mandible retrognathia was investigated by placing the patient seated in the Frankfort horizontal position with a virtual vertical line dropped from the vermilion border of the lower lip to the chin. If the anterior prominence of the chin (soft tissue pogonion) is great than 2 mm behind this line, mandibular retrodisplacement may be present (9). High arched palate was defined by the presence of all the following features: 1) a narrow and high palatal vault, 2) a corresponding narrow arch form, and 3) unilateral or bilateral buccal tilting of the maxillary alveolar arches with posterior teeth in crossbite (10). A BMI ≥ 27 was defined as obesity.
The Stardust II (STD II) (Respironics Inc., Murraysville, PA, USA) is a type 3 portable monitoring (PM) that is designed to measure and record 5 diagnostic parameters: SpO2 (via finger probe), pulse rate (from the oximeter probe), airflow (pressure based airflow through a nasal cannula), respiratory effort (piezoelectric sensor in a belt placed mid-thorax), and body position (mercury switch built into the STD II unit and worn mid-sternum). An internal 9 V battery powers the STD II and allows up to 10 hr of data collection. Data are collected and stored on internal memory in the device. The data are then downloaded to a computer for automated analysis by the host software (Stardust Host Software, Respironics, Inc.). Manual review and validation of the automatically scored data can be performed. A research assistant instructed the participants how to use the STD II at home. The explanation consisted of consistent verbal and written instructions illustrating the correct hook-up of the STD II, and included diagrams and a brief demonstration (11).
For STD II scoring, hypopnea was defined as more than a 50% discernable decrement in airflow lasting ≥ 10 sec with a 3% reduction in SpO2. Apneas were required to show cessation of airflow ≥ 10 sec (whether central, obstructive, or mixed). The total recording time was used in the denominator to calculate the apnea-hypopnea index (AHI).
Statistical analyses were performed using SPSS version 18.0 for Windows (SPSS Inc., Chicago, IL, USA). Categorical data were analyzed using the chi-square test, and continuous data using the independent t test. Logistic regression analysis was used to identify variables independently correlated with OSAS. Results were presented as mean ± SD or as an adjusted odds ratio and corresponding 95% confidence intervals. P values of < 0.05 were considered as having statistical significance.
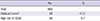
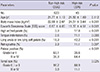
Ninety subjects (13.5%) of all participants reported habitual snoring. Fifty subjects (8.1%) were predicted to be at high risk of OSAS by the questionnaire (Table 1). All subjects classified as being at high risk of OSAS underwent portable monitoring. Among the 50 subjects, 45 persons were found to have AHI ≥ 5. The distribution of the AHI in subjects at high risk of obstructive sleep apnea syndrome shows in Table 2. Table 3 shows the clinical differences between the groups of non-snorers and habitual snorers. The mean ages were 21.7 and 21.6 yr in the non-snorers and habitual snorers, respectively. There was no significant difference between the groups in age. BMI and ESS score were significantly higher in habitual snorers. The prevalence of high arched palate, tongue indentation, long uvula or low lying soft palate and retrognathia was significantly higher in habitual snorers. In addition, the prevalence of grade III or IV in palatal position and tonsil size was higher in habitual snorers. Table 4 shows the clinical differences between the high risk OSAS group and non-high risk OSAS group. The results of the comparison between the two groups showed that they were similar results in Table 3.
To identify predictive factors associated with OSAS in subjects, we divided the subjects into two groups according to the presence of OSAS. We utilized the backward stepwise method of multiple logistic regression analysis. Finally, high arched palate (odds ratio [OR] = 5.300; P = 0.005), long uvula or low lying soft palate (OR = 2.579; P = 0.022), tonsil size III or IV (OR = 5.351; P = 0.012), ESS > 10 (OR = 4.152; P < 0.001) and obesity (BMI > 27 kg/m2) (OR = 3.157; P = 0.039) were found to independently predict OSAS in subjects (Table 5).
The aim of this study was to estimate the prevalence and risk factors of snoring and high risk of OSAS in young male soldiers in Korea. The prevalence of habitual snoring was 13.5% and high risk of OSAS by the Berlin questionnaire was 8.1%.
To our knowledge, this study is the first report on the prevalence and risk factors of OSAS in the young military population in Korea. There have been many previous epidemiologic studies of the prevalence of SDB, but there is little data on its prevalence in young adults.
In a study on the prevalence of snoring and SDB in a university student population using a questionnaire survey followed by home sleep monitoring, overall, 25.7% of subjects reported snoring, and the prevalence of SDB in monitored subjects was 2.3% (12). The questionnaire used in this study was the Sleep and Health Questionnaire. In this questionnaire, questions are categorized into mild, moderate, and severe according to the severity of snoring. Therefore, it did not estimate the frequency of snoring. In our study, the habitual snorer was defined as a person who snores frequently (4-5/week) or always (6-7/week). In addition, the female to male ratio in the population was 1.8:1. Therefore, it is likely that our results of the young adult male population show a higher prevalence rate compared with that of the university student population. According to results from the National Sleep Foundation Sleep in America 2005 poll, of the 1,506 respondents, 26% (31% of the men and 21% of the women) met the Berlin questionnaire criteria (13). Particularly, 18% of those persons 18 to 29 yr of age were at high risk. Moreno et al. (14) applied the Berlin Questionnaire to 10,101 truck drivers and reported that 26% were high risk for OSAS. When our results are compared with those of the previous two studies, the prevalence of high risk for OSAS in our study shows a lower rate. The possible reason for having a lower prevalence of high risk for OSAS compared with western studies may be due to the difference in the prevalence of obesity, a strong risk factor for OSAS. Moreover, the mean BMI of our subjects was 21.98 ± 2.5 which was lower than that of the Korean adult population (15).
The significance of physical examination for detection of OSAS is controversial. While Viner et al. (16), Friedman et al. (17), and Zonato et al. (18) concluded that it is possible to identify patients with OSAS based on the history and anatomical findings, Dreher et al. (19) claimed that medical history and anatomical findings are insufficient to adequately predict the presence or absence of OSAS (19). However, for the otorhinolaryngologist, routine physical examination and history taking are essential to identify OSAS in patients seeking treatment for snoring. These examinations allow for better treatment prioritisation and a more evidence-based approach in patient management. In our results, all variables of upper airway bony and soft tissue structural abnormalities that we checked were significantly more frequent in subjects with a higher risk of OSAS.
If there were any obstructions in the nasal or nasopharyngeal pathways such as adenotonsillar hypertrophy or allergic rhinitis in childhood, the nasal breathing pattern might be changed to a mouth breathing pattern (20). Mouth-breathing individuals have been classically described as having a narrow, V-shaped maxillary arch, a high palatal vault, proclined upper incisors and a Class II occlusal relationship (21). High arched palate from among these can be a major reason for high nasal airway resistance that may contribute to the development of obstructive sleep apnea (OSA). Also, Cistulli et al. (22) observed modest correlations between indexes of maxillary constriction and sleep apnea severity. It is known that a long uvula or low lying soft palate and enlarged tonsil can be lead to airway obstruction by decreasing airway caliber. Previous pathologic studies have demonstrated thickening, fibrosis and fat deposition in the uvula and soft palate of the patient with OSA (23). Tonsil hypertrophy is the most common risk factor for sleep-disordered breathing in children (24). But in previous studies, in which the study population was mainly middle aged, enlarged tonsil was more infrequent than in our study (19, 25). A possible reason for this might be that enlarged tonsil was an independent predictive value in our study unlike other studies.
Overall, we found that the prevalence of snoring and high risk of OSAS in young male soldiers in Korea was 13.5% and 8.1%, respectively. It is not a low prevalence, considering the populations are young and non-overweight individuals. High arched palate, long uvula or low lying soft palate, tonsil size III or IV, ESS > 10 and obesity were independent predictive factors of OSAS. For early identification and treatment of young soldiers with OSAS in a military environment, a precise screening by questionnaire and physical examination is needed.
Figures and Tables
References
1. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000; 342:1378–1384.
2. Canessa N, Castronovo V, Cappa SF, Aloia MS, Marelli S, Falini A, Alemanno F, Ferini-Strambi L. Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med. 2011; 183:1419–1426.
3. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; 328:1230–1235.
4. Findley LJ, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM. Cognitive impairment in patients with obstructive sleep apnea and associated hypoxemia. Chest. 1986; 90:686–690.
5. Ulfberg J, Carter N, Edling C. Sleep-disordered breathing and occupational accidents. Scand J Work Environ Health. 2000; 26:237–242.
6. Haraldsson PO, Carenfelt C, Diderichsen F, Nygren A, Tingvall C. Clinical symptoms of sleep apnea syndrome and automobile accidents. ORL J Otorhinolaryngol Relat Spec. 1990; 52:57–62.
7. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999; 131:485–491.
8. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14:540–545.
9. Ridley MB. Aesthetic facial proportions. In : Papel ID, Nachlas NE, editors. Facial plastic and reconstructive surgery. St Louis: Mosby-Year Book;1992. p. 106.
10. Seto BH, Gotsopoulos H, Sims MR, Cistulli PA. Maxillary morphology in obstructive sleep apnoea syndrome. Eur J Orthod. 2001; 23:703–714.
11. Ahmed M, Patel NP, Rosen I. Portable monitors in the diagnosis of obstructive sleep apnea. Chest. 2007; 132:1672–1677.
12. Hui DS, Chan JK, Ho AS, Choy DK, Lai CK, Leung RC. Prevalence of snoring and sleep-disordered breathing in a student population. Chest. 1999; 116:1530–1536.
13. Hiestand DM, Britz P, Goldman M, Phillips B. Prevalence of symptoms and risk of sleep apnea in the US population: results from the national sleep foundation sleep in America 2005 poll. Chest. 2006; 130:780–786.
14. Moreno CR, Carvalho FA, Lorenzi C, Matuzaki LS, Prezotti S, Bighetti P, Louzada FM, Lorenzi-Filho G. High risk for obstructive sleep apnea in truck drivers estimated by the Berlin questionnaire: prevalence and associated factors. Chronobiol Int. 2004; 21:871–879.
15. Moon OR, Kim NS, Jang SM, Yoon TH, Kim SO. The relationship between body mass index and the prevalence of obesity-related diseases based on the 1995 National Health Interview Survey in Korea. Obes Rev. 2002; 3:191–196.
16. Viner S, Szalai JP, Hoffstein V. Are history and physical examination a good screening test for sleep apnea? Ann Intern Med. 1991; 115:356–359.
17. Friedman M, Tanyeri H, La Rosa M, Landsberg R, Vaidyanathan K, Pieri S, Caldarelli D. Clinical predictors of obstructive sleep apnea. Laryngoscope. 1999; 109:1901–1907.
18. Zonato AI, Bittencourt LR, Martinho FL, Júnior JF, Gregório LC, Tufik S. Association of systematic head and neck physical examination with severity of obstructive sleep apnea-hypopnea syndrome. Laryngoscope. 2003; 113:973–980.
19. Dreher A, de la Chaux R, Klemens C, Werner R, Baker F, Barthlen G, Rasp G. Correlation between otorhinolaryngologic evaluation and severity of obstructive sleep apnea syndrome in snorers. Arch Otolaryngol Head Neck Surg. 2005; 131:95–98.
20. Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981; 79:359–372.
21. McNamara JA. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981; 51:269–300.
22. Cistulli PA, Richards GN, Palmisano RG, Unger G, Berthon-Jones M, Sullivan CE. Influence of maxillary constriction on nasal resistance and sleep apnea severity in patients with Marfan's syndrome. Chest. 1996; 110:1184–1188.
23. Stauffer JL, Buick MK, Bixler EO, Sharkey FE, Abt AB, Manders EK, Kales A, Cadieux RJ, Barry JD, Zwillich CW. Morphology of the uvula in obstructive sleep apnea. Am Rev Respir Dis. 1989; 140:724–728.
24. Potsic WP, Wetmore RF. Sleep disorders and airway obstruction in children. Otolaryngol Clin North Am. 1990; 23:651–663.
25. Schellenberg JB, Maislin G, Schwab RJ. Physical findings and the risk for obstructive sleep apnea. The importance of oropharyngeal structures. Am J Respir Crit Care Med. 2000; 162:740–748.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download