Abstract
We investigated the demographic characteristics and risk factors of Korean patients with naÏve central or branch retinal vein occlusion (CRVO or BRVO). This study enrolled 41 clinical sites throughout Korea and included 557 consecutive patients with retinal vein occlusion (RVO) from May through November 2010. A total of 557 patients with new-onset RVO participated in this study. Two hundred and three (36.4%) patients were diagnosed with CRVO and 354 (63.6%) patients were diagnosed with BRVO. Comparisons between the two groups showed that the prevalence of diabetes mellitus was significantly higher in CRVO patients and hypertension was significantly higher in BRVO patients (P = 0.001 and 0.002, respectively). Poor baseline visual acuity was significantly associated with female and old age in BRVO patients (P = 0.002 and 0.013, respectively), whereas the wide intraretinal hemorrhage (CRVO, P = 0.029; BRVO, P < 0.001) and the macular ischemia (CRVO, P < 0.001; BRVO, P < 0.001) were associated with both groups. The study results show the clinical features of RVO in Korean patients. Hypertension is strongly associated with BRVO and diabetes mellitus is more strongly associated with CRVO in Korean patients with RVO. As the first nationwide study performed by the Korean Retinal Society, the results of this study can be applied to future studies on RVO.
Retinal vein occlusion (RVO) is a major retinal vascular disorder that causes sight-threatening conditions in older adults. Secondary macular edema usually results in decreased visual acuity due to either central retinal vein occlusion (CRVO) or branch retinal vein occlusion (BRVO) (1). Previously reported major epidemiologic studies have described the prevalence, systemic risk factors, and clinical course of RVO, but most of these studies were performed in white populations (2-6). Only limited studies on RVO in Asian populations have been performed (7-9). In addition, there are no large-scale studies on the incidence, risk factors, or clinical patterns of RVO in Korean populations.
The purpose of this study was to examine the demographic characteristics and risk factors of naïve RVO patients who visited tertiary care centers in Korea. Because Korea is a racially homogenous nation, the study results can provide additional information about the clinical features of RVO in other northeast Asian countries.
This multicenter, cross-sectional study was performed as a nationwide survey in 2010. The survey included a detailed interview regarding RVO-related risk factors. In addition, the systemic and ocular findings in each patient were confirmed by retinal specialists.
All 557 consecutive new cases of RVO that presented at each institute were included in this study. For each patient, complete physical and ocular examinations were performed, including an interview regarding past medical history. To confirm RVO, an ocular examination was performed on all patients that included fundus photography, fluorescein angiography, and optical coherence tomography (OCT).
All patients included in this study were diagnosed with new-onset RVO (≤ 6 months). Patients with diabetic retinopathy (except mild nonproliferative diabetic retinopathy), RVO due to other causes (e.g., known uveitis or vasculitis), RVO accompanied by arterial occlusion or ocular ischemic syndrome, or a prior history of intraocular injection, laser treatment, or vitrectomy for RVO were excluded from the study population.
Detailed data on patient demographics, past medical histories, and ocular symptoms were collected. Each patient's complete systemic medical history related to RVO was examined for indications of hypertension, diabetes mellitus (DM), heart disease, cerebrovascular accidents, renal disease, and hyperlipidemia. Lifestyle factors, such as smoking habits and alcohol consumption, were determined from the initial interview. Resting blood pressure was measured using standard protocols. In addition, 24-hr blood pressure monitoring was performed, if needed, for the diagnosis of hypertension. To confirm other systemic diseases, some patients underwent laboratory testing that included a complete blood count, electrolyte and chemical batteries, lipid panel, determination of fasting blood sugar, postprandial blood sugar test, and hemophilia testing.
Snellen best-corrected visual acuity (BCVA), refractive error, and intraocular pressure were determined and recorded. A detailed anterior segment examination was carried out to determine if neovascularization of the iris had occurred. After dilation of the pupil, the lens status was determined and a fundus examination was performed. The findings of the fundus examination were recorded in terms of the type of RVO (CRVO or BRVO), presence of any optic disc abnormalities, macular edema, neovascularization at the disc or elsewhere, extent of retinal hemorrhage, and other abnormal findings such as vitreous hemorrhage. The patient's history of ocular surgery was also determined, including cataract surgery, vitrectomy, and glaucoma surgery.
Baseline fundus photography, fundus fluorescein angiography, and OCT were performed on all patients. Each scan set was independently graded by two different readers. In cases of disagreement, the senior reader made a unilateral decision regarding unresolved data. Using imaging data, the scan quality was first evaluated. Then, using fundus photography, the type of RVO, location of RVO, and abnormalities in the optic disc area and macular area were reassessed. Using early- and peak-phase fluorescein angiography, abnormalities in the optic disc area (e.g., leakage, presence of collaterals, and neovascularization), the presence of macular ischemia (e.g., foveal avascular zone disruption, leakage, and intraretinal cystoid spaces), the extent of capillary nonperfusion, and the presence of neovascularization in the parafoveal area were examined. In this study, eyes with hemiretinal vein occlusion are regarded as eyes with CRVO and assigned to the CRVO group. Using the horizontal and vertical OCT images, the central macular thickness and abnormalities of the vitreomacular interface, including epiretinal membrane, macular edema, photoreceptor inner segment/outer segment disruption, intraretinal cyst, and the presence of subretinal fluid, were assessed. Differences in central macular thickness, depending on the OCT machine used, were corrected according to an established reference (10).
Differences in the baseline continuous variables between the patients with CRVO and BRVO were evaluated using the t test. The Pearson chi-square test and Fisher exact test were used to test for differences in the baseline categorical variables between participants with CRVO and BRVO. The Pearson correlation coefficient was used to measure the linear association between baseline logMAR visual acuity and the central thickness determined using OCT. Univariate analysis was performed to determine the association between the baseline variables and Snellen visual acuity. The patients were divided into 3 groups according to baseline Snellen visual acuity: ≤ 0.2, 0.2-0.5, and > 0.5. In patients with RVO, one-way analysis of variance (ANOVA) was used to identify associations between baseline BCVA and the continuous variables, and the Pearson chi-square test was used to identify the association between baseline BCVA and the categorical variables.
After identifying the significant factors using univariate analysis, multiple linear regression models were used to describe the association between variables and baseline logMAR visual acuity. Standardized beta coefficients were used to compare changes in baseline BCVA that were associated with the independent variables that were expressed in incomparable units of measurement. SPSS (version 18.0; SPSS Inc., Chicago, IL, USA) was used to conduct all of the statistical analyses, and P < 0.05 was considered statistically significant.
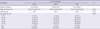
Baseline data were collected from 557 consecutive RVO patients from 41 clinical sites throughout Korea during the 7-month period from May through November 2010. Baseline demographic data on the study population are shown in Table 1. This study included data on 203 patients with CRVO (36.4%) and 354 patients with BRVO (63.6%). The CRVO population contained similar proportions of men and women, however the number of female patients was higher in the BRVO population. The mean ages were similar in both groups (59.8 yr [range: 16-89]) for CRVO and 58.2 yr [range: 31-97] for BRVO). Also, there were no differences in terms of the age distributions.
The baseline systemic and ocular conditions of the study population are shown in Table 2. The prevalence of DM and hypertension was generally high in both groups. However, the prevalence of hypertension at baseline was higher in the BRVO group (48.2%) than the CRVO group (34.7%, P = 0.002). In terms of DM, CRVO patients (20.2%) demonstrated a higher prevalence at baseline than BRVO patients (9.9%, P = 0.001). The mean resting systolic and diastolic blood pressures were also higher in BRVO patients (P = 0.003 and 0.008, respectively). There was no statistically significant difference between the 2 groups in terms of the incidence of cerebrovascular accident (CVA), renal disease, ocular surgery, or smoking.
In terms of ocular symptoms, even though the CRVO patients tended to visit a hospital a few days earlier than the BRVO group, there was no difference between the 2 groups in terms of the reported duration of symptoms at the initial consultation (P = 0.063).
BCVA demonstrated a significant difference between 2 groups. The percentage of CRVO patients with Snellen BCVA < 0.2 was higher and the mean logMAR BCVA of the CRVO patients was also significantly worse (P = 0.025 and 0.002, respectively). The number of CRVO patients with a Snellen BCVA ≤ 0.2 was 91 (44.8%). The distribution of visual acuity was significantly different from that of the BRVO patients, which consisted of 118 patients with a Snellen BCVA ≤ 0.2 (35.1%).
Also, the baseline OCT-measured center macular thickness was higher in the CRVO patients. The mean OCT-measured center point thickness was 499.65 µm in CRVO patients and 444.38 µm in BRVO patients (P = 0.002). In terms of wide intraretinal hemorrhage in the central area, BRVO patients demonstrated a higher percentage of occurrence (80.4%) than CRVO patients (69.3%, P = 0.005). However, more CRVO patients presented with a wide nonperfusion area on angiography (P = 0.005).
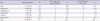
The relationship between BCVA at baseline and the other demographic and ocular characteristics was analyzed using univariate analysis and multiple regression analysis (Table 3 and Table 4). Using univariate analysis, old age, female sex, wide area of intraretinal hemorrhage, and the presence of macular ischemia on fluorescein angiography were found to be significant factors associated with poor BCVA in BRVO patients. For CRVO patients, old age, high systolic blood pressure, wide area of intraretinal hemorrhage, and the presence of macular ischemia on fluorescein angiography were also significant factors. On multiple regression analysis, the significant factors associated with the development of poor baseline visual acuity were female sex and old age for the BRVO patients, whereas a wide area of intraretinal hemorrhage and the presence of macular ischemia were significant factor for both groups. In both groups, high OCT-measured central macular thickness was a significant factor associated with a low initial BCVA. However, the correlation coefficients were relatively low (CRVO = 0.396; BRVO = 0.390; Fig. 1).
This study was performed as a nationwide study in Korea. Forty-one clinical sites throughout Korea participated. Comparing the national distribution of the participating clinical sites with that of the general population of Korea, the number of participating clinical sites that were located in Seoul is relatively high (Table 5) (11, 12). However, considering the national distribution of upper-level general hospitals (officially designated as tertiary hospital by the Ministry of Health and Welfare of Korea), the number of upper-level general hospitals and participating clinical sites in Seoul are similar (17 [38.6%] and 18 [43.9%]), respectively). Furthermore, the distribution of participating clinical sites in other areas also shows a similar pattern with that of the upper-level general hospitals. In addition, in the case of the diagnosis of a relatively serious disease, such as RVO, many Koreans tend to visit general hospitals in major cities, including Seoul, rather than staying at local primary healthcare clinics. Considering these facts, the characteristics of the consecutive new-onset RVO patients who were enrolled in this study might be representative of the nature of Korean RVO patients, including the incidence of RVO and the distribution ratio of BRVO: CRVO.
The results of the current study demonstrate the association between both types of RVO, systemic hypertension, and DM. According to recent reports, the prevalence of systemic hypertension and diabetes in adults > 30 yr old in Korea are 26.9% and 9.7%, respectively (13). Compared with these data, the prevalences of both diseases are high in this study group. These findings have already been noted in previous studies on CRVO and BRVO (14-19). In this study, the prevalence of hypertension in BRVO patients (48.2%) was significantly higher compared with the prevalence of hypertension in CRVO patients (34.7%; P = 0.002). Also, the mean resting blood pressure (both systolic and diastolic) was significantly higher in BRVO patients (BRVO, 137.1/82.4 mmHg; CRVO, 132.3/79.7 mmHg). This may suggest that hypertension is a more important risk factor for the development of BRVO than CRVO in Korean RVO patients. A previously reported large-scale study also noted that systemic hypertension was a greater risk factor for the development of BRVO (270 patients) than CRVO (258 patients), demonstrating a borderline level of statistical significance (P = 0.09) (20).
This result may reflect differences in the pathogeneses of BRVO and CRVO. The well-known important factors that demonstrate a relationship between BRVO and hypertension are degenerative changes in the vessel wall and compression of the vein at the arteriovenous crossing site. A number of studies have also shown histological changes in vessel walls. Seitz (21) suggests that compression of the overlaying artery causes trophic changes to the venous endothelium and intima media that are the root of BRVO pathogenesis. In addition, Frangieh et al. (22) reported that 90% of patients showed evidence of intima-medial layer hypertrophy and intravenous thrombosis. Anatomical features can also be related to the development of hypertension, such as sharing a common adventitial sheath and a relatively anteriorly positioned retinal artery.
The prevalence of DM was significantly higher in CRVO patients (CRVO, 20.2%; BRVO, 9.9%; P = 0.001). The cumulative evidence gathered from previous studies supports our data. However, treatment of DM is associated with a higher risk of developing CRVO than the risk factors associated with CRVO and BRVO (18, 20). Also, Suzuki et al. (23) noted that multiple inflammatory cytokines and neurotrophic factors (such as vascular endothelial growth factor [VEGF] and anti-inflammatory cytokines including interleukin [IL]-10 and IL-13) may be involved in the common pathogenic mechanisms of CRVO and diabetic retinopathy. The associations between the cardiovascular risk factors of Korean RVO patients appear to be similar to those of other population-based studies. Hypertension may be a more important contributing factor to the development of BRVO, and DM may be related to the development of CRVO.
The current study analyzed the relationship between baseline BCVA and demographic features, ocular findings, and several other parameters determined by ocular examinations. This study shows that female sex was one of the demographic factors associated with low baseline BCVA in BRVO group. To identify the possible reason, we compared the age distributions of the male and female patients in the BRVO group. The proportion of elderly persons (> 60 yr of age) in the female subgroup was higher compared with that of the male subgroup (50.2% vs 37.2%, respectively). Old age itself may act as causative factor for low visual acuity, as it is also associated with senile cataracts, age-related macular degeneration, and other degenerative conditions. Also, the baseline demographic data of this study show that the proportion of female patients in the BRVO group was significantly higher compared with that of the CRVO group. These facts might reflect the difference in the incidence of BRVO between males and females, especially in the elderly Korean population.
In terms of the findings on the ocular examinations, wide (> 5 disc areas) areas of intraretinal hemorrhage and the presence of macular ischemia in both groups were significant factors associated with a low baseline BCVA. These findings indicate that a large amount of intraretinal hemorrhage and severe ischemic retinal damage follow vascular occlusion and are the main causes of the loss of visual acuity.
In addition, this study may provide data on the natural courses of both ischemic and nonischemic CRVO. Even though we did not define ischemic CRVO, such as areas ≥ 10 disc areas of retinal capillary nonperfusion on fluorescein angiography, we can classify CRVO patients according to their initial ocular condition and examination results. Large areas of capillary nonperfusion (≥ 5 disc areas), severe venous dilatation and tortuosity, retinal hemorrhage, macular edema, cotton wool spots, and severely decreased initial visual acuity could be the criteria for the diagnosis of ischemic and nonischemic CRVO. At the end of data collection and analysis, not only were the natural courses of ischemic and nonischemic CRVO described, but so were the contributing factors for the conversion from nonischemic to ischemic CRVO.
Similar to other studies, the OCT-measured macular and foveal thickness did not show a strong correlation with visual acuity in either group (CRVO, 0.396; BRVO, 0.390; Fig. 1). These findings also support the notion that OCT-measured macular thickness does not exactly represent visual acuity. A previously published study explained the weak correlation between OCT-measured macular thickness, macular ischemia, photoreceptor damage, and the accumulation of subfoveal hard exudates, not only in RVO but also other retinal disease such as diabetic retinopathy and age-related macular degeneration (24-29).
The limitations of our study include the nature of its cross-sectional design. Causality cannot be inferred from the results. Second, this study was performed as a survey, not a clinical trial. This means that there was no strict protocol for acquiring data. Because of that, various kinds of machines (e.g., fundus cameras and OCT machines) and scan methods were used. This fact makes it impossible to apply a standard protocol to each case. However, all of the imaging data were interpreted by highly skilled retinal specialists who were blind to the clinical characteristics using a common grading protocol. Also, poor-quality images, such as those with an off-centered placement or poor focus, were excluded from the data analysis. These efforts may make up for the weak points of this study.
In conclusion, the results of this study show that hypertension is strongly associated with BRVO and DM is more strongly associated with CRVO in Korean patients with RVO. Furthermore, severe intraretinal hemorrhage and macular ischemia were significantly associated with poor baseline visual acuity in both patients with CRVO and BRVO. The findings obtained at the initial visit and the ocular imaging data obtained at baseline give us additional information related to visual acuity. This is the first nationwide cross-sectional study performed by the Korean Retinal Society that describes the clinical features of RVO. The results of this study can be applied to future studies on RVO.
Figures and Tables
Fig. 1
Scatter plot of baseline OCT-measured central macular thickness and BCVA in (A) CRVO (correlation coefficient = 0.396, P < 0.001) and (B) BRVO patients (correlation coefficient = 0.390, P < 0.001). BCVA, best-corrected visual acuity; OCT, optical coherence tomography; CRVO, central retinal vein occlusion; BRVO, branch retinal vein occlusion.

ACKNOWLEDGMENTS
The Korean RVO Study Group Members
Writing Committee
Joo Yong Lee (Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Young Hee Yoon (Chair, Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Ha Kyoung Kim (Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine), Hee Seong Yoon (Sungmo Eye Hospital), Se Woong Kang (Samsung Medical Center, Sungkyunkwan University College of Medicine), June-Gone Kim (Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Kyu Hyung Park (Department of Ophthalmology, Seoul National University College of Medicine and Bundang Hospital), Young Joon Jo (Department of Ophthalmology, Chungnam National University Hospital).
Investigators
Se Woong Kang (Samsung Medical Center, Sungkyunkwan University College of Medicine), Hyoung Jun Koh (Department of Ophthalmology, The Institute of Vision Research, Yonsei University College of Medicine), Eui Young Kweon (Department of Ophthalmology, Chonbuk National University Medical School), Kwang Soo Kim (Department of Ophthalmology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine), Seong Woo Kim (Department of Ophthalmology, Korea University College of Medicine), Young Gyun Kim (Department of Ophthalmology, Eulji University School of Medicine), Yu Cheol Kim (Department of Ophthalmology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine), Yun Young Kim (Department of Ophthalmology, Catholic University of Daegu College of Medicine), In Taek Kim (Department of Ophthalmology, Kyungpook National University School of Medicine), Jung Yeul Kim (Department of Ophthalmology, Chungnam National University Hospital), June-Gone Kim (Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Chul Gu Kim (Myung-Gok Eye Research Institute, Kim's Eye Hospital, Konyang University College of Medicine), Tae Wan Kim (Department of Ophthalmology, Seoul National University College of Medicine and Seoul Metropolitan Boramae Hospital), Ha Kyoung Kim (Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine), Hyun Woong Kim (Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine), Hyun-Jin Kim (Department of Ophthalmology, Ewha Womans University School of Medicine), Hyung Chan Kim (Department of Ophthalmology, Konkuk University Medical Center, Konkuk University School of Medicine), Dong Heun Nam (Department of Ophthalmology, Gachon University Gil Medical Center, Gachon University), Woo Ho Nam (Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine), Sang Woong Moon (Department of Ophthalmology, East-West Neo Medical Center, KyungHee University College of Medicine), Yeon Sung Moon (Department of Ophthalmology, Inha University School of Medicine), Kyu Hyung Park (Department of Ophthalmology, Seoul National University College of Medicine and Bundang Hospital), Young Sook Park (HanGil Eye Hospital), In Won Park (Department of Ophthalmology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine), Jong Mun Park (Department of Ophthalmology, Gyeongsang National University School of Medicine), Jong Seok Park (Department of Ophthalmology, Eulji General Hospital, Eulji University School of Medicine), Tae Kwann Park (Department of Ophthalmology, Soonchunhyang University College of Medicine), Joon Hong Sohn (HanGil Eye Hospital), Yumi Song (Dae Jin Medical Center), Ji Hun Song (Department of Ophthalmology, Ajou University School of Medicine), Yang Seung Jae (Department of Ophthalmology, Gangneung Asan Hospital, University of Ulsan College of Medicine), Yunsik Yang (Department of Ophthalmology, College of Medicine, Wonkwang University), Jae Ryung Oh (Department of Ophthalmology, Korea University College of Medicine), Jae Yoon Oh (Saevit Eye Center), Young-Hoon Ohn (Department of Ophthalmology, Soonchunhyang University College of Medicine), Se Joon Woo (Department of Ophthalmology, Seoul National University College of Medicine and Bundang Hospital), Seung Young Yu (Department of Ophthalmology, Kyung Hee University School of Medicine), Hyeong Gon Yu (Department of Ophthalmology, Seoul National University College of Medicine), Ho Min Lew (Department of Ophthalmology, Ajou University School of Medicine), Young Hee Yoon (Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Hee Seong Yoon (Sungmo Eye Hospital), Dae Young Lee (Department of Ophthalmology, Gachon University Gil Medical Center, Gachon University), Byung Ro Lee (Department of Ophthalmology, Hanyang University College of Medicine), Sang Joon Lee (Department of Ophthalmology, Kosin University College of Medicine), Sung Jin Lee (Department of Ophthalmology, Soonchunhyang University College of Medicine), Sung Chul Lee (Department of Ophthalmology, Yonsei University College of Medicine), Jae Heung Lee (Myung-Gok Eye Research Institute, Kim's Eye Hospital), Jong Hyun Lee (Department of Ophthalmology, Inje University Ilsan Paik Hospital, Inje University College of Medicine), Joo Yong Lee (Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine), Joo Eun Lee (Department of Ophthalmology, Inje University Haeundae Paik Hospital, Inje University College of Medicine), Tae Gon Lee (Department of Ophthalmology, Konyang University Hospital), Moo Hwan Chang (Department of Ophthalmology, Dankook University Medical College), Young Joon Jo (Department of Ophthalmology, Chungnam National University Hospital), Ho Kyun Cho (Department of Ophthalmology, Chung-Ang University College of Medicine), Ju Byung Chae (Department of Ophthalmology, College of Medicine, Chungbuk National University), Kyung Seek Choi (Department of Ophthalmology, Soonchunhyang University College of Medicine), Gwang Ju Choi (Department of Ophthalmology, School of Medicine, Chosun University), Jung Il Han (Department of Ophthalmology, Kim's Eye Hospital, Myung-Gok Eye Research Institute Konyang University), Don Il Ham (Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine), Kuhl Huh (Department of Ophthalmology, Korea University College of Medicine).
The authors have no conflicts of interest to disclose.
References
1. Hayreh SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res. 2005. 24:493–519.
2. Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the beaver dam eye study. Trans Am Ophthalmol Soc. 2000. 98:133–141.
3. Mitchell P, Smith W, Chang A. Prevalence and associations of retinal vein occlusion in Australia: the blue mountains eye study. Arch Ophthalmol. 1996. 114:1243–1247.
4. Wong TY, Larsen EK, Klein R, Mitchell P, Couper DJ, Klein BE, Hubbard LD, Siscovick DS, Sharrett AR. Cardiovascular risk factors for retinal vein occlusion and arteriolar emboli: the atherosclerosis risk in communities & cardiovascular health studies. Ophthalmology. 2005. 112:540–547.
5. Varma R, Paz SH, Azen SP, Klein R, Globe D, Torres M, Shufelt C, Preston-Martin S. The Los Angeles Latino Eye Study: design, methods, and baseline data. Ophthalmology. 2004. 111:1121–1131.
6. Cheung N, Klein R, Wang JJ, Cotch MF, Islam AF, Klein BE, Cushman M, Wong TY. Traditional and novel cardiovascular risk factors for retinal vein occlusion: the multiethnic study of atherosclerosis. Invest Ophthalmol Vis Sci. 2008. 49:4297–4302.
7. Lim LL, Cheung N, Wang JJ, Islam FM, Mitchell P, Saw SM, Aung T, Wong TY. Prevalence and risk factors of retinal vein occlusion in an Asian population. Br J Ophthalmol. 2008. 92:1316–1319.
8. Liu W, Xu L, Jonas JB. Vein occlusion in Chinese subjects. Ophthalmology. 2007. 114:1795–1796.
9. Arakawa S, Yasuda M, Nagata M, Ninomiya T, Hirakawa Y, Doi Y, Kiyohara Y, Ishibashi T. Nine-year incidence and risk factors for retinal vein occlusion in a general Japanese population: the Hisayama Study. Invest Ophthalmol Vis Sci. 2011. 52:5905–5909.
10. Retinal Physician. Normative databases in SD-OCT: a status report. accessed on 1 April 2012. Available at http://www.retinalphysician.com/articleviewer.aspx?articleID=104438.
11. Statistics Korea. Korean statistical information service. accessed on 1 April 2012. Available at http://kosis.kr/abroad/abroad_01List.jsp.
12. Ministry of Health & Welfare [Rep.of Korea]. Statistical information by Ministry of Health and Welfare. accessed on 1 April 2012. Available at http://www.mw.go.kr/front/jb/sjb0601vw.jsp?PAR_MENU_ID=03&MENU_ID=03160501&page=1&CONT_SEQ=238954&SEARCHKEY=TITLE&SEARCHVALUE=%C1%BE%C7%D5%BA%B4%BF%F8.
13. Korea Centers for Disease Control & Prevention. Korea National Health & Nutrition Examination Survey. accessed on 1 April 2012. Available at http://knhanes.cdc.go.kr/knhanes/sub04/sub04_03.do?classType=7.
14. Appiah AP, Greenidge KC. Factors associated with retinal-vein occlusion in Hispanics. Ann Ophthalmol. 1987. 19:307–309. 312
15. Appiah AP, Trempe CL. Risk factors associated with branch vs. central retinal vein occlusion. Ann Ophthalmol. 1989. 21:153–155. 157
16. Elman MJ, Bhatt AK, Quinlan PM, Enger C. The risk for systemic vascular diseases and mortality in patients with central retinal vein occlusion. Ophthalmology. 1990. 97:1543–1548.
17. Johnston RL, Brucker AJ, Steinmann W, Hoffman ME, Holmes JH. Risk factors of branch retinal vein occlusion. Arch Ophthalmol. 1985. 103:1831–1832.
18. McGrath MA, Wechsler F, Hunyor AB, Penny R. Systemic factors contributory to retinal vein occlusion. Arch Intern Med. 1978. 138:216–220.
19. Rath EZ, Frank RN, Shin DH, Kim C. Risk factors for retinal vein occlusions: a case-control study. Ophthalmology. 1992. 99:509–514.
20. Sperduto RD, Hiller R, Chew E, Seigel D, Blair N, Burton TC, Farber MD, Gragoudas ES, Haller J, Seddon JM, et al. Risk factors for hemiretinal vein occlusion: comparison with risk factors for central and branch retinal vein occlusion: the eye disease case-control study. Ophthalmology. 1998. 105:765–771.
21. Seitz R. The retinal vessels: comparative ophthalmoscopic and histologic studies on healthy and diseased eyes. 1964. Saint Louis: CV Mosby;102–146.
22. Frangieh GT, Green WR, Barraquer-Somers E, Finkelstein D. Histopathologic study of nine branch retinal vein occlusions. Arch Ophthalmol. 1982. 100:1132–1140.
23. Suzuki Y, Nakazawa M, Suzuki K, Yamazaki H, Miyagawa Y. Expression profiles of cytokines and chemokines in vitreous fluid in diabetic retinopathy and central retinal vein occlusion. Jpn J Ophthalmol. 2011. 55:256–263.
24. Klein R, Klein BE, Moss SE, Linton KL. The beaver dam eye study: Retinopathy in adults with newly discovered and previously diagnosed diabetes mellitus. Ophthalmology. 1992. 99:58–62.
25. Jahn CE, Töpfner von Schutz K, Richter J, Boller J, Kron M. Improvement of visual acuity in eyes with diabetic macular edema after treatment with pars plana vitrectomy. Ophthalmologica. 2004. 218:378–384.
26. Pendergast SD, Hassan TS, Williams GA, Cox MS, Margherio RR, Ferrone PJ, Garretson BR, Trese MT. Vitrectomy for diffuse diabetic macular edema associated with a taut premacular posterior hyaloid. Am J Ophthalmol. 2000. 130:178–186.
27. Goebel W, Kretzchmar-Gross T. Retinal thickness in diabetic retinopathy: a study using optical coherence tomography (OCT). Retina. 2002. 22:759–767.
28. Shah SP, Patel M, Thomas D, Aldington S, Laidlaw DA. Factors predicting outcome of vitrectomy for diabetic macular oedema: results of a prospective study. Br J Ophthalmol. 2006. 90:33–36.
29. Otani T, Kishi S. A controlled study of vitrectomy for diabetic macular edema. Am J Ophthalmol. 2002. 134:214–219.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download