INTRODUCTION
Although metastatic neoplasms of the spine are common, pure intramedullary spinal cord metastasis (ISCM) is a rare manifestation of systemic cancer, which indicates the occurrence of remote dissemination, and thus, the terminal phase of cancer (1-3). The most common primary tumors of ISCM are from the lung, breast and melanoma, which account for about three-fourth, but lymphoma, kidney, colon and thyroid are uncommon (4-6). There are only a few reports presenting ISCM originated from renal cell carcinoma which was histologically confirmed, and there is no report in Korea (7-9). We report a unique case of a patient with an ISCM originated from RCC who underwent surgery due to a rapid progression of paraparesis during focal radiotherapy.
CASE DESCRIPTION
A 44-yr-old male was diagnosed with renal cell carcinoma on the left kidney with lung metastasis and was treated by molecular target agent therapy (Sunitinib, 37.5 mg/day, per oral, 4/2 week scheduled) without surgery (Fig. 1). After 6 months later from a diagnosis of RCC, he presented rapid progressive paraparesis and both leg numbness. His motor power of both hip flexion was 3/5 (0; none, 5; normal) and other distal lower extremity was 4/5.
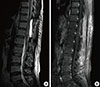
Magnetic resonance image (MRI) of the spine revealed intramedullary mass lesion on T12 level (Fig. 2). This lesion showed iso-signal intensity (SI) on T1 weighted images (T1WI) and high-SI on T2 weighted images (T2WI) with significant rim enhancement after gadolinium based contrast agent injection. Extensive edematous infiltration on intramedullary space which shows high SI on T2WI was checked up to the upper thoracic level.
Focal radiotherapy on the spine was initiated due to his refusal for surgery. Over the following 10 days during radiotherapy, his neurological deficit rapidly progressed to 2-3/5 on the right lower extremity and 0-1/5 on the left lower extremity. Under the umbilicus level (sensory dermatome level T10), all components of sensory, including pain, touch, vibration and temperature, were decreased and painful paresthesia on both lower extremities was checked. He also complained of urinary incontinence and decreased anal sphincter tone was checked on the neurological examination.
For the rapid progression of neurological deficit, emergency surgery was performed. Under the neural integrity monitoring (NIM-SPINE, Medtronic Sofamor Danek, USA), laminectomy of T10, T11, and T12 was performed. Under the intra-operative ultrasonographic view, mass lesion was confirmed near the T12 pedicle. After midline dural incision, arachnoid membrane was opened. For abnormal lesion was not checked on the surface of the spinal cord, posterior myelotomy through midline posterior sulcus was performed. After gentle dissection, soft and grayish colored tumor lesion distinguishable on microscopic view was checked. Microsurgical removal of the tumor with the use of Cavitron Ultrasonic Aspirator (CUSA, Valleylab, USA) was performed. On the neural integrity monitoring, no abnormal signal change was checked during the whole operation.
After surgery, painful paresthesia of both lower extremities was immediately improved on the visual analogue scale (VAS) from 7 to 2. Significant improvement of motor power to self-ambulation with walking stick was checked on an outpatient follow-up after 2 months later from surgery. Follow up MRI imaging after 2 months later from surgery, enhancing mass lesion was nearly total removed and edematous infiltration on T2WI was significantly reduced (Fig. 3).
On a histological examination, it was composed of nests of clear tumor cells with intermediate nuclear grade vascular meshwork and showed a strong cytoplasmic reaction within tumor cells in immunohistochemical staining for both cytokeratin and vimentin (Fig. 4).
On the neurological examination of 6 months from surgery, the motor power of both lower limbs was improved to 3-4/5, and he could walk by himself with the assistant of a walking stick.
DISCUSSION
ISCM is rare and clinically affects only 0.1%-0.4% of all cancer patients (1, 2, 10). The most commonly described tumors in association with ISCM include lung cancer and breast cancer; on the other hand, RCC has been described to constitute about 4%-9% of the total number of ISCM (4-7). For the rarity of metastasis intramedullary, as well as the low incidence of itself, only a few cases of ISCM originated from RCC have been reported with histological confirmation in the literature (7-9, Table 1). To our best knowledge, this is the first published case report with histological confirmation in Korea.
There are several hypotheses to explain how to metastasize into the spinal cord parenchyma. Kalayci et al. (6) reviewed articles and summarized them into 3 pathologic mechanisms. First, haematogeneous spread via the artery or vertebral venous plexus (Batson's venous plexus) is believed to account for most cases. Second, tumor cells originated from carcinomatous meningitis infiltrate into the Virchow-Robin spaces of the vessels, penetrate the pial membrane and invade the spinal cord parenchyma. The third mechanism is direct invasion from contiguous structures. In our case, considering the high incidence of anastomosis between the left renal vein and the vertebral venous plexus, hematogenous spread can be a reasonable mechanism (10).
Treatment modalities for ISCM include radiotherapy, surgery, and chemotherapy. The modality of treatment should be decided by clinical and neurological status. Focal radiotherapy has been accepted for an effective treatment modality for ISCM with arresting tumor growth and preventing further neurological deficit (11). However, the efficacy of radiotherapy may be limited to radio-sensitive tumors, such as small cell lung cancer, breast cancer, and lymphoma. These radio-sensitive tumors are most frequently found as the origin of ISCM (4-6). Previous reports favoring radiation therapy are somewhat biased as their clinical elements mainly consist of these radio-sensitive tumors. Despite the radio-resistance of RCC itself, focal radiotherapy has been preferred for the first-line treatment modality of ISCM from RCC due to the absence of effective systemic therapy for metastatic RCC and short life expectancy which estimated at 3 to 9 months (3, 12). However, in selected cases with solitary lesion and rapidly progressing neurological deficits but incomplete, surgical management can be an effective salvage procedure. In our case, despite the focal radiotherapy, his neurological symptom was rapidly deteriorated, but improved after surgery.
Our case indicates that the ISCM, despite the extremely rare incidence, is a considerable pathology in patients with RCC. Additionally, our case emphasizes the importance of surgical management as a salvage option in cases with progressive neurological deficit, especially for the patients with radio-resistant primary tumor, such as RCC.
In conclusion, we report a case of ISCM originated from RCC that was removed successfully by a surgical procedure. This is the first published Korean case, to our best knowledge, which shows an ISCM from RCC with histological report via surgery.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download