Abstract
Urinary biomarkers of acute kidney injury (AKI) have been revealed recently to be useful for prior prediction of AKI. However, it is unclear whether these urinary biomarkers can also detect recovery from established AKI. Urinary biomarkers, including neutrophil gelatinase-associated lipocalin (NGAL) and cystatin C, were measured every 2 days for 8 days in 66 patients with AKI. At day 0, there were no significant differences in plasma creatinine, BUN, and urine cystatin C between AKI patients in the recovery (n = 33) and non-recovery (n = 33) groups. Plasma creatinine concentrations were significantly lower in the recovery group (3.0 ± 2.0 mg/dL) than in the non-recovery group (5.4 ± 1.9 mg/dL) on day 4 after AKI diagnosis (P < 0.001). In contrast, there were significant differences in urine NGAL between the two groups starting on day 0 (297.2 ± 201.4 vs 407.6 ± 190.4 ng/mL, P = 0.025) through the end of the study (123.7 ± 119.0 vs 434.3 ± 121.5 ng/mL, P < 0.001). The multiple logistic regression analysis showed that urine NGAL could independently predict recovery from AKI. Conclusively, this prospective observational study demonstrates that urine NGAL can be a highly versatile marker for early detection of the recovery phase in established AKI patients.
Acute kidney injury (AKI) is a common and serious complication for hospitalised patients. AKI increases morbidity and mortality, especially in the intensive care unit (ICU) (1). Many studies report AKI complications in up to 7% of all hospital admissions and 50%-80% of ICU patients (2), with 5% requiring renal replacement therapy (3). The incidence of AKI increased 13% per year between 1979 and 2004 in the US (4). A history of AKI is associated with an increased risk of end stage renal disease (ESRD) (5). Despite significant improvement in our understanding of the pathophysiology of AKI over the past several decades (6-9), as well as the discovery of several interventional treatments, the mortality rate of AKI has not improved. Difficulty at early detection and lack of early intervention tools are the main causes of AKI treatment failures.
Diagnostic markers for AKI, which have been used for several decades, include plasma creatinine, blood urea nitrogen (BUN), presence or absence of urinary casts, fractional excretion of sodium (FENa), and urinary concentration. However, these markers are of limited use for early detection of AKI (10, 11).
Recently, several sensitive and specific biomarkers for the early detection of AKI have been identified. Neutrophil gelatinase-associated lipocalin (NGAL), cystatin C, kidney injury molecule-1 (KIM-1), N-acetyl-β-D-glucosaminidase (NAG), interleukin-18 (IL-18), hepatocyte growth factor (HGF), and vascular endothelial growth factor (VEGF) are some of the novel and promising biomarkers for early diagnosis of AKI (12).
However, it is unclear whether such biomarkers can also detect the recovery of kidney function from established AKI. In this study, we investigated whether decreases in urine NGAL and cystatin C precede the changes in plasma creatinine in the recovery phase of AKI. We also assessed the utility of urine NGAL and cystatin C for early prediction of recovery.
This study was conducted at Kwandong University Myongji Hospital between May 2009 and April 2010. We measured urine NGAL and cystatin C levels every 2 days for 8 days in AKI patients. AKI was defined as a 50% or greater increase in plasma creatinine from baseline. Baseline renal function was defined as the lowest known plasma creatinine value during the preceding 3 months. This study included AKI patients 18-70 yr old, excluding those with pre-existing chronic kidney disease stage 3-5, oliguria less than 100 mL/day, a history of hemodialysis or continuous renal replacement therapy during their hospitalization, or diagnosed prerenal acute renal failure or those without baseline plasma creatinine measurements. Of the 98 patients screened for study enrolment, 32 were excluded because they met one or more of the exclusion criteria. The primary end point was recovery from AKI, defined as a 50% or greater decrease in plasma creatinine from the peak level. Demographic and clinical data, including age, gender, baseline serum creatinine, comorbidities, and prior renal disease, were obtained from medical records. Following enrolment, BUN, plasma creatinine, and urine creatinine levels were measured along with urine collection every 2 days. The modified Jaffé method was used to measure plasma creatinine. For the control group, serum and urine samples were collected from 15 individuals without diagnosed renal disease.
Random spot urine samples were centrifuged at 2,000 g for 5 min, and the supernatants were stored in aliquots at -80℃. Urine NGAL and cystatin C levels were measured using the human NGAL Enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis, MN, USA) and the cystatin ELISA kit (Bio-Vendor LLC, Candler, NC, USA). The laboratory investigators were blind to information about the samples. The mean intra-assay coefficient of variation in the laboratory was 10.0%.
Statistical analyses were used to compare the recovery and non-recovery AKI patients. Continuous variables, including urine NGAL and cystatin C level, were expressed as mean ± standard deviation (SD) and compared using Student's t test. Skewed data were expressed as median with interquartile range and compared using Mann-Whitney U test. Categorical variables were expressed as proportions and compared using the chi-square test or Fisher's exact test. We generated a nonparametric receiver operating characteristic (ROC) curve to evaluate the ability of urinary biomarkers to detect AKI recovery. P < 0.05 was considered statistically significant. Univariate and multivariate stepwise regression analyses were used to assess predictors of AKI recovery. Statistical analyses were performed using SPSS, version 10.0 (SPSS Inc, Chicago, IL, USA).
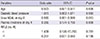
Of the 98 patients who developed AKI during hospitalisation, 66 were included in the study, 33 in the recovery group and 33 in the non-recovery group (Table 1). There were no significant differences between the recovery and non-recovery groups with respect to age, sex, and underlying diseases or baseline serum haemoglobin, total cholesterol, albumin, BUN, plasma creatinine, and new simplified acute physiology (SAPS II) score. However, the recovery group has higher RIFLE-F prevalence, lower-diastolic blood pressure (70.0 ± 12.0 vs 63.2 ± 13.1 mmHg, P = 0.04), and higher in-hospital mortality (12.1% vs 39.4%, P = 0.023).
The most common cause of AKI was sepsis/infection (50.0%), followed by ischemia (27.3%), and nephrotoxins (19.7%) (Table 2). There were no significant differences in the causes of AKI between the groups.
On day 0, there were no significant differences in plasma creatinine and BUN between the recovery and non-recovery groups (Fig. 1). On day 4, there was a statistically significant difference in plasma creatinine (3.0 ± 2.0 vs 5.4 ± 1.9 mg/dL, P < 0.001). However, there was a significant difference in urine NGAL from day 0 (297.2 ± 201.4 vs 407.6 ± 190.4 ng/mL, P = 0.025), which was continued through day 8 (123.7 ± 119.0 vs 434.3 ± 121.5 ng/mL, P < 0.001). This pattern was observed day 0 through day 8 even after urine NGAL was normalised with urine creatinine.
These early changes were not observed with urine cystatin C. The recovery group's urine cystatin C level was not significantly lower than the non-recovery group's level until day 4 (263.8 ± 202.1 vs 302.4 ± 121.9 mg/L, P = 0.383). The significant difference in urine cystatin C between groups on day 4 was observed only after normalisation with urine creatinine (7.5 ± 1.6 vs 12.8 ± 1.8 mg/g Cr, P = 0.03). In the control group, urine NGAL and cystatin C level were 69.0 ± 10.5 ng/mL and 37.24 ± 7.3 mg/L, respectively.
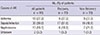
The ability of urine NGAL to predict recovery from AKI was assessed using an ROC curve (Fig. 2). Urine NGAL at day 0 was a useful predictor of renal recovery (AUC = 0.78, 95% CI 0.65-0.90, P < 0.01) and the cut-off value of urine NGAL was 348.2 ng/mL (sensitivity = 0.840, specificity = 0.687). The AUCs for predicting AKI recovery using urine NGAL from days 2, 4, 6, and 8 were 0.813, 0.854, 0.884, and 0.969, respectively.
According to the multiple logistic regression model, which included age, diastolic BP, urine NGAL on day 0, plasma creatinine on day 4, and RIFLE criteria, urine NGAL on day 0, prior to changes in plasma creatinine, was predictive of recovery from AKI (Table 3).
Recently, the term "acute renal failure" was replaced by "acute kidney injury" (13, 14). A terminological change results from a conceptual paradigm shift. As many studies have shown, a mild elevation in plasma creatinine may reflect severe kidney damage and poor prognosis.
In addition, plasma creatinine does not reflect early kidney injury. For that reason, the RIFLE (Risk-Injury-Failure-Loss-End stage kidney disease) classification for AKI was created in 2004 to provide consensus criteria for defining and classifying AKI (15). However, because plasma creatinine does not change until about 50% of renal function is lost, it is not a sensitive marker for early detection of AKI, even when the new AKI classification is applied (16). For this reason, researchers are looking for alternative biomarkers. Changes in urine NGAL, cystatin C, NAG, KIM-1 and IL-18, which precede a decline in glomerular filtration rate, are commonly used as biomarkers for tubular cell damage (17-19). The ideal renal enzyme establishment for detecting AKI could be helpful for early intervention and better prognosis.
NGAL is a 25-kDa protein of the lipocalin family that is initially bound to gelatinase in specific granules of neutrophils and other epithelial cells, including those of the proximal collecting tubule. Its expression is induced in injured epithelia, including epithelia of the lungs, colon, and especially the kidneys (20). In a prospective study of 71 pediatric patients undergoing cardiopulmonary bypass for cardiac corrective surgery by Mishra et al. (21), changes in urine NGAL helped detect AKI 1-3 days before any increase in plasma creatinine. In a study of 426 adult patients undergoing cardiac surgery, the increase in urine NGAL was closely related to cardiopulmonary bypass time and aortic cross-clamp time (22). Hypo-perfusion time was correlated with urine NGAL but not plasma creatinine. Since the publication by Mishra et al. (23), many studies have used urine NGAL for early detection of AKI. Currently, NGAL is the most promising biomarker (19, 24-26). Cystatin C is a 13-kDa protein produced by all nucleated cells, which acts as an important extracellular inhibitor of cysteine proteases. It is filtered by the glomerulus and completely reabsorbed by the proximal tubule and, therefore, is not detected in the urine of normal subjects. Elevated urinary cystatin C reflects tubular cell damage; it is not affected by sex, age, race, and muscle mass. Urine cystatin C is available for early AKI detection almost 2 days before plasma creatinine levels change (27, 28).
Although the ability of NGAL and cystatin C to detect AKI early has been shown under various conditions, the ability of NGAL and cystatin C to predict recovery from AKI has not been sufficiently investigated. Identifying non-recovery patients have several potential benefits such as identification of patients who will receive the most benefit from interventions, determination of the optimal timing to initiate intervention, initiation of intervention or medications to slow deterioration of renal function, and determination of the quality of life after hospital discharge (29). In addition, this has therapeutic implications such as to identify patients who are at risk for failure to recover early and enroll a uniform cohort of patients who are unlikely to recover in a biomarker-guided clinical trial of severe AKI (30).
In this study, we demonstrated that urine NGAL and cystatin C levels correlate with renal recovery and that urine NGAL decreases 4 days before plasma creatinine changes in AKI patients without renal replacement therapy. This study suggests that urine NGAL may be helpful in predicting recovery from AKI early, and the cut-off value was 348 ng/mL. Some reports are accordance with our present study. Srisawat et al. (30, 31) reported that plasma NGAL can predict recovery from AKI following community acquired pneumonia and that urine NGAL and urine HGF can predict renal recovery in critically ill patients with renal support. Decreasing urine NGAL and urine HGF in the first 14 days was associated with greater odds of renal recovery. Kümpers et al. (25) suggested that serum NGAL is an independent predictor of 28-day mortality in ICU patients with renal replacement therapy. The cut-off value of serum NGAL for 28-day mortality was 360 ng/mL. AUC of the ROC curve is 0.74 (95% CI 0.64-0.84). In addition, Hollmen et al. (32) reported that NGAL is a marker of graft recovery after kidney transplantation. The urinary NGAL on day 1 predicted prolonged delayed graft function lasting longer than 7, 14 days (AUC 0.748) with cut-off value 560 ng/mL. Also, Yang et al. (33) reported that initial urine NGAL is an independent predictor of not only in-hospital mortality, but also persistent loss of renal function after one month in 100 patients with AKI, in Korea.
Many studies evaluating AKI non-recovery have studied only patients receiving renal replacement therapy (RRT). In the study for patients with RRT, AKI non-recovery was only defined as patients who are alive and dialysis-dependence (29), because the levels of biomarker could be affected with RRT. Therefore, we exclude the patients who need RRT early, because RRT may effect and change the levels of serum and urine biomarkers, then be confounding factors for decision of renal function recovery. This is an important difference compared with other studies.
Some authors suggest that results using one biomarker parameter have modest prediction, therefore, a model combined biomarkers and clinical variables is the most predictive. Add on clinical model to plasma NGAL increased the AUC for prediction of failure to renal function recovery from 0.74 to 0.80 in patients with AKI following community-acquired pneumonia (30). Because of the heterogeneous causes of AKI and underlying comorbidity, the use of multiple biomarker panels to predict renal recovery seems reasonable. In addition, mortality rate in AKI patients is very high (34). Therefore, several factors associated with mortality, such as happening of other complications during treatment and whether recovery of underlying disease or not, must be considered as important in the study for recovery of renal function.
There are several limitations to our study. First, because of the small sample size, we could not control for selection bias. Second, because our data came from a single centre, our results lack external validity. Also, because this study is just observational, it would not be so affective. Third, our study did not control for AKI etiology and lack of blinding. In the future, a large prospective, multi-center, controlled study should be conducted.
In conclusion, this study demonstrates that urine NGAL levels decline earlier than plasma creatinine levels in the recovery phase of patients with AKI and that urine NGAL can detect recovery from AKI.
Figures and Tables
 | Fig. 1BUN (A), plasma Cr (B), urine NGAL (C), urine NGAL/Cr (D), urine cystatin C (E), urine cystatin C/Cr (F) levels every 2 days for 8 day period stratified by recovery and non-recovery from AKI. Urine NGAL level shows statistically significant difference between groups since day 0 preceding the difference in plasma Cr level.*P < 0.01 comparing recovery group vs non-recovery group; †P < 0.05 comparing recovery group vs non-recovery group. BUN, blood urea nitrogen; Cr, creatinine; NGAL, Neutrophil gelatinase-associated lipocalin; AKI, acute kidney injury. |
 | Fig. 2ROC curve for the detection of AKI recovery using urine NGAL at day 0 after AKI diagnosis. ROC curve demonstrates the prognostic sensitivity and specificity of urine NGAL in the prediction of AKI recovery (AUC = 0.78; 95% CI 0.64-0.90). AUC, Area under the curve; ROC, Receiver operating characteristic; AKI, Acute kidney injury; NGAL, Neutrophil gelatinase-associated lipocalin. |
Table 1
Baseline characteristics and mortality stratified by recovery and non-recovery from established acute kidney injury (AKI)

*Data are expressed as median (interquartile range). RIFLE, Risk-Injury-Failure-Loss-End stage kidney disease; ICU, intensive care unit; SAPS, simplified acute physiology score; BP, blood pressure; BUN, blood urea nitrogen; Cr, creatinine; CRP, C-reactive protein; FENa, fractional excretion of sodium.
Notes
References
1. Thadhani R, Pascual M, Bonventre JV. Acute renal failure. N Engl J Med. 1996; 334:1448–1460.
2. Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005; 16:3365–3370.
3. Koyner JL, Bennett MR, Worcester EM, Ma Q, Raman J, Jeevanandam V, Kasza KE, O'Connor MF, Konczal DJ, Trevino S, et al. Urinary cystatin C as an early biomarker of acute kidney injury following adult cardiothoracic surgery. Kidney Int. 2008; 74:1059–1069.
4. Schrier RW. Early intervention in acute kidney injury. Nat Rev Nephrol. 2010; 6:56–59.
5. Wald R, Quinn RR, Luo J, Li P, Scales DC, Mamdani MM, Ray JG. University of Toronto Acute Kidney Injury Research Group. Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA. 2009; 302:1179–1185.
6. Price PM, Safirstein RL, Megyesi J. The cell cycle and acute kidney injury. Kidney Int. 2009; 76:604–613.
7. Okusa MD. The inflammatory cascade in acute ischemic renal failure. Nephron. 2002; 90:133–138.
8. Day YJ, Huang L, Ye H, Li L, Linden J, Okusa MD. Renal ischemia-reperfusion injury and adenosine 2A receptor-mediated tissue protection: the role of CD4+ T cells and IFN-gamma. J Immunol. 2006; 176:3108–3114.
9. Del Rio M, Imam A, DeLeon M, Gomez G, Mishra J, Ma Q, Parikh S, Devarajan P. The death domain of kidney ankyrin interacts with Fas and promotes Fas-mediated cell death in renal epithelia. J Am Soc Nephrol. 2004; 15:41–51.
10. Devarajan P. Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol. 2006; 17:1503–1520.
11. Haase M, Bellomo R, Devarajan P, Schlattmann P, Haase-Fielitz A. NGAL Meta-analysis Investigator Group. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009; 54:1012–1024.
12. Vaidya VS, Waikar SS, Ferguson MA, Collings FB, Sunderland K, Gioules C, Bradwin G, Matsouaka R, Betensky RA, Curhan GC, et al. Urinary biomarkers for sensitive and specific detection of acute kidney injury in humans. Clin Transl Sci. 2008; 1:200–208.
13. Waikar SS, Liu KD, Chertow GM. Diagnosis, epidemiology and outcomes of acute kidney injury. Clin J Am Soc Nephrol. 2008; 3:844–861.
14. Goldstein SL, Chawla LS. Renal angina. Clin J Am Soc Nephrol. 2010; 5:943–949.
15. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004; 8:R204–R212.
16. Soni SS, Ronco C, Katz N, Cruz DN. Early diagnosis of acute kidney injury: the promise of novel biomarkers. Blood Purif. 2009; 28:165–174.
17. Han WK, Waikar SS, Johnson A, Betensky RA, Dent CL, Devarajan P, Bonventre JV. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008; 73:863–869.
18. Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002; 62:237–244.
19. Lebkowska U, Malyszko J, Lebkowska A, Koc-Zorawska E, Lebkowski W, Malyszko JS, Kowalewski R, Gacko M. Neutrophil gelatinase-associated lipocalin and cystatin C could predict renal outcome in patients undergoing kidney allograft transplantation: a prospective study. Transplant Proc. 2009; 41:154–157.
20. Bolignano D, Donato V, Coppolino G, Campo S, Buemi A, Lacquaniti A, Buemi M. Neutrophil gelatinase-associated lipocalin (NGAL) as a marker of kidney damage. Am J Kidney Dis. 2008; 52:595–605.
21. Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005; 365:1231–1238.
22. Wagener G, Gubitosa G, Wang S, Borregaard N, Kim M, Lee HT. Urinary neutrophil gelatinase-associated lipocalin and acute kidney injury after cardiac surgery. Am J Kidney Dis. 2008; 52:425–433.
23. Mishra J, Ma Q, Prada A, Mitsnefes M, Zahedi K, Yang J, Barasch J, Devarajan P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003; 14:2534–2543.
24. Cruz DN, de Cal M, Garzotto F, Perazella MA, Lentini P, Corradi V, Piccinni P, Ronco C. Plasma neutrophil gelatinase-associated lipocalin is an early biomarker for acute kidney injury in an adult ICU population. Intensive Care Med. 2010; 36:444–451.
25. Kümpers P, Hafer C, Lukasz A, Lichtinghagen R, Brand K, Fliser D, Faulhaber-Walter R, Kielstein JT. Serum neutrophil gelatinase-associated lipocalin at inception of renal replacement therapy predicts survival in critically ill patients with acute kidney injury. Crit Care. 2010; 14:R9.
26. Bennett M, Dent CL, Ma Q, Dastrala S, Grenier F, Workman R, Syed H, Ali S, Barasch J, Devarajan P. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: a prospective study. Clin J Am Soc Nephrol. 2008; 3:665–673.
27. Herget-Rosenthal S, Marggraf G, Hüsing J, Göring F, Pietruck F, Janssen O, Philipp T, Kribben A. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004; 66:1115–1122.
28. Villa P, Jiménez M, Soriano MC, Manzanares J, Casasnovas P. Serum cystatin C concentration as a marker of acute renal dysfunction in critically ill patients. Crit Care. 2005; 9:R139–R143.
29. Srisawat N, Murugan R, Wen X, Singbartl K, Clermont G, Eiam-Ong S, Kellum JA. Recovery from acute kidney injury: determinants and predictors. Contrib Nephrol. 2010; 165:284–291.
30. Srisawat N, Murugan R, Lee M, Kong L, Carter M, Angus DC, Kellum JA. Genetic and Inflammatory Markers of Sepsis (GenIMS) Study Investigators. Plasma neutrophil gelatinase-associated lipocalin predicts recovery from acute kidney injury following community-acquired pneumonia. Kidney Int. 2011; 80:545–552.
31. Srisawat N, Wen X, Lee M, Kong L, Elder M, Carter M, Unruh M, Finkel K, Vijayan A, Ramkumar M, et al. Urinary biomarkers and renal recovery in critically ill patients with renal support. Clin J Am Soc Nephrol. 2011; 6:1815–1823.
32. Hollmen ME, Kyllönen LE, Inkinen KA, Lalla ML, Salmela KT. Urine neutrophil gelatinase-associated lipocalin is a marker of graft recovery after kidney transplantation. Kidney Int. 2011; 79:89–98.
33. Yang HN, Boo CS, Kim MG, Jo SK, Cho WY, Kim HK. Urine neutrophil gelatinase-associated lipocalin: an independent predictor of adverse outcomes in acute kidney injury. Am J Nephrol. 2010; 31:501–509.
34. Singbartl K, Kellum JA. AKI in the ICU: definition, epidemiology, risk stratification, and outcomes. Kidney Int. 2012; 81:819–825.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download