Abstract
We performed a nationwide epidemiological study to evaluate the prevalence and characteristics of nocturnal enuresis (NE) in Korean adolescents and adults. A questionnaire was sent via e-mail to 51,073 people aged 16-40 yr by stratified sampling according to age, sex, and region among a 200,000 internet survey panel pool. The questionnaire included following information; presence or absence of NE, frequency of NE, possible risk factors for NE, self-esteem scale score and depression score results, and measures for the treatment of NE. Among the 2,117 responders, 54 (2.6%) had NE (≥1 enuretic episode within 6 months). Of 54 bedwetters, 9.3% wet ≥1 night per week and 20.5% wet ≥1 per month. The prevalence rates remained relatively stable with no apparent trend of reduction with age. The presence of sleep disturbance, family history, urgency, or urge incontinence increased the probability of NE episode significantly. The self-esteem score was lower (P=0.053) and the depression scale score was higher (P=0.003) in bedwetters compared with non-bedwetters. Overall 2.6% of Korean aged 16-40 yr have NE. The higher rate of urgency and urge incontinence in adolescent and adult enuretics suggests that bladder function has an important role in adolescent and adult NE.
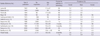
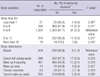
Nocturnal enuresis (NE) is defined as an intermittent incontinence of urine or bedwetting while sleeping regardless of the presence or absence of concomitant daytime voiding symptoms by the International Children's Continence Society (1). The terminology of NE can be applicable only after the attainment of bladder control or age 5 yr, and is one of the most common pediatric health issues. The leading pathophysiological mechanisms of pediatric NE are several factors such as increased nocturnal urine production, decreased nocturnal bladder capacity or bladder instability, or decreased sensation perception of stimulus by bladder fullness during sleeping (2). Pediatric NE is thought be a self-limiting problem because most children outgrow bedwetting with advancing age. The prevalence of NE in children is known as 15%-20% at 5 yr, and decreases with age (3-5). In spite of the spontaneous cure rate of 15% per year, the prevalence of NE in the adolescent and adult population has been reported as 0.2%-3.8% by several researchers (6-16) (Table 1). From an etiologic view, a large percentage of adolescent and adult NE patients are thought to be patients whose pediatric NE persists.
Another pathophysiology of adolescent and adult NE may include various medical problems or underlying urological diseases. However, to date, there has been only minimal research regarding NE in the adolescent and adult population. Some of the previous studies cover only selected populations such as military officers, adolescents, or the elderly. Therefore, we performed a nationwide epidemiological study to evaluate the prevalence and characteristics of NE in Korean adolescents and adults.
A nationwide cross-sectional study was conducted through the internet survey automation system in Korea between March and April 2005. A questionnaire was made by experts who were affiliated to the Korean Children's Continence and Enuresis Society. It was sent to randomly select 51,073 people aged from 16 to 40 yr via e-mail among 200,000 internet survey panel pool (Embrain Co., Korea, http://www.embrain.com) by stratified sampling according to age, sex, and region.
The questionnaire was designed for the convenience of the web-based responders and included demographic information such as age, gender, final education level, occupation, and marital state; characteristics of NE such as whether or not the responder had NE, NE episode according to the proposed period (1, 3, 6, and 12 months), and frequency of NE. In addition, measures for the treatment of NE; possible risk factors such as sleep disorder, family history, past history of urological disease, present urological disease, urinary frequency, urgency, and urge incontinence, self-esteem scale score (SES) and depression score (Center for Epidemiologic Studies and Depression Scale; CES-D) (17, 18) were analyzed.
We assessed the cumulative prevalence of NE in Korean adolescents and adults during the past l, 3, 6, and 12 months before the survey date. Then we analyzed the frequency of NE, the risk factors for NE, and the influence of NE to self-esteem state and depression score in the persons who experienced at least one enuretic episode during the past 6 months.
Statistical analysis was performed using SPSS 18.0 for Windows (SPSS for Windows, SPSS Inc, Chicago, IL, USA). A logistic regression analysis was used to evaluate the association between risk factors and NE. A t-test was used to compare self-esteem/depression scale score between non-enuretic and enuretic people. A chi square test was used to compare NE prevalence according to the sleep variables. A P value less than 0.05 was considered to be statistically significant.
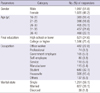
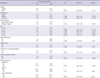
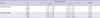
Among 51,073 people who were sent the questionnaire via e-mail, 8,748 persons checked the e-mail. We selected 2,117 respondents (1,097 males and 1,020 females) for the final analysis using stratified sampling according to age, sex, and region on the basis of population data of Statistics Korea (the National Statistical Office of Korea). The demographic data of the total 2,117 responders including gender, age, education, occupation, and marital state were summarized in Table 2. Analyzed by the period (at least one enuretic episode per given period), the cumulative prevalence of NE in Korean adolescent and adults was 0.5% in one month, 1.4% in 3 months, 2.6% in 6 months, and 4.5% in 12 months. Of the 54 responders who experienced at least one enuretic episode within 6 months, 2 (3.7%) responders experienced 2-3 enuretic episodes per week, 3 (5.6%) responders 1 episode per week, 1 (1.9%) responder 2-3 episodes per month, 5 (9.3) responders 1 episode per month, 4 (7.4%) responders 1 episode per 2-3 months, 7 (13.0%) responders 1 episode per 3-6 months, and 32 (59.3%) responders 1 episode per 6-12 months. In other words, 5 (9.3%) had at least one NE episode per week, and 11 (20.5%) had at least one NE episode per month. The analyzed data of the 54 responders who experienced at least one enuretic episode per 6 months was summarized in Table 3. The overall prevalence was 2.6%, and the prevalence of males and females was 2.1% and 3.0% respectively. The prevalence rates remained relatively stable among different age groups, with no apparent trend of a reduction with age. A past history of urological disease, present urological disease, and combined urinary frequency increased the probability of NE without statistical significance. The presence of sleep disturbance (odds ratio=3.546, P=0.001), family history (odds ratio= 3.242, P=0.001), urgency (odds ratio=2.477, P=0.001), or urge incontinence (odds ratio=5.823, P<0.001) increased the probability of NE episodes significantly. The self-esteem score was lower (P=0.053) and the depression scale score was higher (P=0.003) in bedwetters compared with non-enuretic persons (Table 4). There seems to be no relationship between the sleeping time and the prevalence of NE even though the prevalence of NE was higher when the sleeping time was 8 to 10 hr (P=0.047). When the sleep disturbance was subdivided and analyzed, the prevalence of NE was higher when responders had sleep disturbance of 'cannot fall asleep easily' (P=0.035), 'wake up frequently' (P=0.024), 'wake up early' (P=0.027), or 'chronic insomnia' (P=0.003) (Table 5). For the treatment of NE, 37 (68.5%) did not take any measures for specific treatment, and only 5 (9.3%) visited the hospital. The others (22.2%) used herb medicine or consulted with pharmacists.
There are not many reports discussing adolescent and adult NE. In published literature, the prevalence of adolescent and adult NE was reported to be 0.2%-3.8% (6-16). Levin (6) first reported the prevalence of adolescent and adult NE by investigating its prevalence in a male military personnels aging from 17 to 27 yr, and it was 1.2%. Afterwards, many researchers reported the incidence of adolescent and adult NE, some of them studying military personnels (6-8), and proceeded to investigate the elderly (12), and then adolescents associated with longitudinal cohorts of children (11, 14). More recently, 3 reports with a large population based cross sectional studies were published (13, 15, 16). In a study investigating 11,406 adults aged 18-64 yr old in the Netherlands, the prevalence of NE was reported to be 0.5% (13). The incidence was lower than previously reported studies, because the criteria of NE were narrower than other studies, based on bedwetting once a month or more. In a study performed in Hong Kong on 8,534 adolescents and adults aged 16-40 yr the incidence of NE was reported to be 2.3%, however, the criteria of NE was not explicitly mentioned (15). In a study performed on 1,040 adults aged 18 to >65 yr in the United Kingdom, the incidence of NE was high, and was reported to be 6% (16).
In reports discussing adolescent and adult NE, the criteria of NE were reported differently, and due to this lack of uniformity, adolescent and adult NE prevalence varies from study to study. However, our study provides more information concerning NE duration and frequency compared with previous studies. We consider that using internet based questionnaire research enabled us to describe the duration and frequency of NE in detail and diversely in an identical group. The patients participating in the questionnaire replied by email, and therefore, various replies were possible. In our study, the incidence of patients who experienced at least one episode of bedwetting per one month was 0.5%, and at 3 months 1.4%, at 6 months 2.6%, and at 12 months 4.5%, which was similar to previous studies (12, 13). Among the 54 patients who answered that they experienced NE within the past 6 months, 9.3% experienced NE at least once a week, and 3.7% did 2-3 times per week. This differs significantly from the study of Yeung et al. (15) reported that 53% of adolescent and adult NE patients experience severe NE at least 3 times per week. Although the definite reason for this discrepancy is not yet known, we suppose that differences in answering phone surveys and internet questionnaires, differences in the definition of NE, and cultural differences could be attributed to this difference.
The causes of adolescent and adult NE are basically similar to those of pediatric NE. It is thought that a large percentage of adolescent and adult NE patients are actually patients whose pediatric NE persists. It is also known that patients with pediatric NE more frequently experience lower urinary tract symptoms, including NE (19-21). In studies comparing symptoms in pediatric and adolescent NE patients, adolescents more frequently wet the bed every night (48.3% vs 14.3%) and more frequently experience daytime urinary incontinence (32% vs 14.6%). It is hypothesized that more severe pediatric NE persists into adolescence (22).
Many factors other than persistence of pediatric NE affect adolescent and adult NE. In NE newly occurring in adulthood, NE is related to several medical disease, hormones, cardiovascular diseases, sleep and central nervous system dysfunction, and diverse urological causes (23). Moreover, adolescent and adult NE shows high correlation with voiding dysfunction, and we found evidence for this in previous studies. In studies about adult NE, there was a tendency to show a higher prevalence in older populations, due to age-associated lower urinary tract symptoms. In addition, adults who showed NE in adulthood often had severe accompanying voiding symptoms or severe urological diseases requiring immediate intervention (24, 25).
In this research, the incidence of adolescent and adult NE did not decrease with age. It is because adolescent and adult NE differs from pediatric NE, and does not disappear with time. In adults, lower urinary tract symptoms trigger NE, and voiding symptoms tend to increase with age, however, contrary to our estimation, the incidence of NE did not increase with age in our study. This was probably due to the fact that we investigated patients 16-40 yr old, who were not yet affected by age-related voiding symptoms. However, in our study, the incidence of NE was higher in women than men, which differs from the higher incidence of NE in boys in the pediatric population. We attributed this difference to the higher probability of lower urinary tract symptoms in women than in men in adolescents and adults younger than 40 yr.
Several researchers reported that voiding symptoms such as urge incontinence, and stress urinary incontinence increase anxiety, and depression, and worsen mental health (15, 26). In this study, in an analysis of NE and the self-esteem scale and depression scale, in patients with NE, the self-esteem scale decreased, and was statistically significant in men. In patients with NE, the depression scale increased, and was statistically significant in women. These results are similar with previous studies, and we confirmed the negative effect of NE on mental health associated with self-esteem or depression in the adolescent and adult population. An interesting finding was that according to this study, the effect of NE on mental health differed according to gender. Bedwetting decreased self-esteem in men, and increased depression in women.
According to an analysis of the relationship between NE and sleep, based upon the incidence of NE within the recent 6 months, the incidence of NE was high in patients who slept for 8-10 hr; however, the prevalence in patients whose sleep time was different from the above-mentioned times was similar. Based upon these findings, we concluded that there was no direct correlation between sleep time and incidence of NE. However, concerning sleep disturbance, in patients suffering with even mild disorder, there was a 3.3% incidence of NE, compared with a 1.2% incidence in patients who slept well, showing a relationship between sleep disturbance and NE incidence. The incidence of NE was especially high in the adolescent and adult population with chronic insomnia, and we think that this could be a result of severe NE.
Few studies report on the treatment of adolescent and adult NE, which is still controversial (23). The basic treatment is similar to that of pediatric patients, and can be divided into nonpharmacologic and pharmacologic treatment. The enuresis alarm treatment, which is a first-line treatment method in pediatric patients, requires a lot of effort, and disturbs sleep, and therefore adolescent and adult patients have a high rate of discontinuation (27). However, evidence still suggests that alarm therapy may give a comparable response in compliant patients (28). Just as desmopressin is effective in pediatric patients with nocturnal polyuria and low urine osmolality, desmopressin is effective in adolescents and adults with nocturnal polyuria, and can be safely administered for a long period of time. In pediatric patients, the biggest problem of desmopressin is recurrence of NE after discontinuation of the medication (29). Unlike pediatric NE, adolescent and adult NE is often related with various medical diseases, and voiding symptoms, and when it is caused by urologic problems, surgical treatment is often necessary. Therefore, in treating adolescent and adult NE, in addition to basic diagnostic tools used in pediatric patients, various diagnostic tools are required. According to the severity of voiding symptoms, antimuscarinics, smooth muscle relaxants, botulinum toxoid, and clean intermittent catheterization can be necessary, and when severe, surgical treatment is necessary (24, 25). However, another fact that deserves attention is that 68.5% of adolescent and adults with NE did not seek active treatment, and only 9.3% visited the hospital for treatment. In many previous studies reported in western countries, the percentage of adults with NE who visited the hospital was not high (16), and the percentage was much lower in Korea. The reason is that compared to western countries, Koreans do not consider NE as a severe symptom culturally, and rely on traditional remedies or oriental herb treatment, and this tendency continues into adulthood. Various methods of treatment in pediatric patients have been introduced in treating adolescent and adult NE patients, and have shown success. If risk factors could be defined and eliminated, the symptoms of adolescent and adult NE patients could more improve. We consider that regarding such treatment efficacy, public education is necessary.
One potential limitation of this study was the possibility of selection bias. All the questionnaires were collected by e-mail; therefore, there was a risk of selection of subjects who have easy access to the internet. In reality, more than half of the subjects who replied were office workers or students.
Conclusively, the present study is the first large scale nationwide study on the prevalence of adolescent and adult NE in Korea. The overall prevalence of NE of Korean adolescents and adults in the age of 16-40 yr was 2.6% when we defined the NE as at least one enuretic episode per 6 months. The higher rate of urgency and urge incontinence in adolescent and adult bedwetters means bladder function has an important role in adolescent and adult NE. Bedwetting in the adolescent and adult period had a bad influence on patients' mental health including self-esteem or depression. Clinicians should make an effort to give proper information to adolescent and adult NE patients and also to prepare appropriate strategies for enhancing the treatment outcomes.
Figures and Tables
References
1. Nevéus T, von Gontard A, Hoebeke P, Hjälmås K, Bauer S, Bower W, Jørgensen TM, Rittig S, Walle JV, Yeung CK, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society. J Urol. 2006. 176:314–324.
2. Neveus T, Eggert P, Evans J, Macedo A, Rittig S, Tekgül S, Vande Walle J, Yeung CK, Robson L. International Children's Continence Society. Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International Children's Continence Society. J Urol. 2010. 183:441–447.
3. Fergusson DM, Horwood LJ, Shannon FT. Factors related to the age of attainment of nocturnal bladder control: an 8-year longitudinal study. Pediatrics. 1986. 78:884–890.
4. Bakker E, van Sprundel M, van der Auwera JC, van Gool JD, Wyndaele JJ. Voiding habits and wetting in a population of 4,332 Belgian schoolchildren aged between 10 and 14 years. Scand J Urol Nephrol. 2002. 36:354–362.
5. Howe AC, Walker CE. Behavioral management of toilet training, enuresis, and encopresis. Pediatr Clin North Am. 1992. 39:413–432.
6. Levine A. Enuresis in the navy. Am J Psychiatry. 1943. 100:320–325.
7. Wadsworth ML. Persistent enuresis in adults. Am J Orthopsychiatry. 1944. 14:313–320.
8. Thorne FO. Incidence of nocturnal enuresis after age five. Am J Psychiatry. 1944. 100:686–689.
9. Bieger PP. Nocturnal enuresis in military personnel. Ned Tijdschr Geneeskd. 1954. 98:1839–1846.
10. Cushing FC Jr, Baller WR. The problem of nocturnal enuresis in adults: special reference to managers and managerial aspirants. J Psychol. 1975. 89:203–213.
11. Hellström A, Hanson E, Hansson S, Hjälmäs K, Jodal U. Micturition habits and incontinence at age 17: reinvestigation ofa cohort studied at age 7. Br J Urol. 1995. 76:231–234.
12. Burgio KL, Locher JL, Ives DG, Hardin JM, Newman AB, Kuller LH. Nocturnal enuresis in community-dwelling older adults. J Am Geriatr Soc. 1996. 44:139–143.
13. Hirasing RA, van Leerdam FJ, Bolk-Bennink L, Janknegt RA. Enuresis nocturna in adults. Scand J Urol Nephrol. 1997. 31:533–536.
14. Swithinbank LV, Brookes ST, Shepherd AM, Abrams P. The natural history of urinary symptoms during adolescence. Br J Urol. 1998. 81:90–93.
15. Yeung CK, Sihoe JD, Sit FK, Bower W, Sreedhar B, Lau J. Characteristics of primary nocturnal enuresis in adults: an epidemiological study. BJU Int. 2004. 93:341–345.
16. Buckley BS, Lapitan MC. Prevalence of urinary and faecal incontinence and nocturnal enuresis and attitudes to treatment and help-seeking amongst a community-based representative sample of adults in the United Kingdom. Int J Clin Pract. 2009. 63:568–573.
17. Rosenberg M. Society and the adolescent self-image. 1965. Princeton: Princeton University Press.
18. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977. 1:385–401.
19. Bower WF, Yip SK, Yeung CK. Dysfunctional elimination symptoms in childhood and adulthood. J Urol. 2005. 174:1623–1627.
20. Bower WF, Sit FK, Yeung CK. Nocturnal enuresis in adolescents and adults is associated with childhood elimination symptoms. J Urol. 2006. 176:1771–1775.
21. Fitzgerald MP, Thom DH, Wassel-Fyr C, Subak L, Brubaker L, Van Den Eeden SK, Brown JS. Reproductive Risks for Incontinence Study at Kaiser Research Group. Childhood urinary symptoms predict adult overactive bladder symptoms. J Urol. 2006. 175:989–993.
22. Yeung CK, Sreedhar B, Sihoe JD, Sit FK, Lau J. Differences in characteristics of nocturnal enuresis between children and adolescents: a critical appraisal from a large epidemiological study. BJU Int. 2006. 97:1069–1073.
23. Shadpour P, Shiehmorteza M. Enuresis persisting into adulthood. Urol J. 2006. 3:117–129.
24. Abeygunasekera AM, Jayasinghe RJ, Duminda MT, Chamintha TH, Guruge RW. Significance of recent onset nocturnal enuresis in adult men: a prospective study. Ceylon Med J. 2004. 49:79–81.
25. Sakamoto K, Blaivas JG. Adult onset nocturnal enuresis. J Urol. 2001. 165:1914–1917.
26. Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012. 61:88–95.
27. Läckgren G, Hjälmås K, van Gool J, von Gontard A, de Gennaro M, Lottmann H, Terho P. Nocturnal enuresis: a suggestion for a European treatment strategy. Acta Paediatr. 1999. 88:679–690.
28. Vandersteen DR, Husmann DA. Treatment of primary nocturnal enuresis persisting into adulthood. J Urol. 1999. 161:90–92.
29. Matthiesen TB, Rittig S, Djurhuus JC, Nørgaard JP. A dose titration, and an open 6-week efficacy and safety study of desmopressin tablets in the management of nocturnal enuresis. J Urol. 1994. 151:460–463.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download