Abstract
This study aimed to evaluate the effects of percutaneous coronary intervention (PCI) on short- and long-term major adverse cardiac events (MACE) in elderly (>75 yr old) acute myocardial infarction (AMI) patients with renal dysfunction. As part of Korea AMI Registry (KAMIR), elderly patients with AMI and renal dysfunction (GFR<60 mL/min) received either medical (n=439) or PCI (n=1,019) therapy. Primary end point was in-hospital death. Secondary end point was MACE during a 1 month and 1 yr follow-up. PCI group showed a significantly lower incidence of in-hospital death (20.0% vs 14.3%, P=0.006). Short-term and long-term MACE rates were higher in medical therapy group (31.9% vs 19.0%; 57.7% vs 31.3%, P<0.001), and this difference was mainly attributed to cardiac death (29.3% vs 17.6%; 51.9% vs 25.0%, P<0.001). MACE-free survival time after adjustment was also higher in PCI group on short-term (hazard ratio, 0.67; confidence interval, 0.45-0.98; P=0.037) and long-term follow-up (hazard ratio, 0.61, confidence interval, 0.45-0.83; P=0.002). In elderly AMI patients with renal dysfunction, PCI therapy yields favorable in-hospital and short-term and long-term MACE-free survival.
In the modern world, the elderly population constitutes the most rapidly growing population. Cardiovascular disease is the most frequent disease and leading cause of death in elderly people. The prevalence and severity of atherosclerosis and coronary artery disease increase with age. Moreover, elderly persons account for the majority of deaths from acute myocardial infarction (AMI) (1, 2). Percutaneous coronary intervention (PCI) has been shown to be an effective reperfusion strategy for patients with AMI, and expands eligibility for reperfusion to many patients, including the elderly, who would be considered ineligible for fibrinolytic therapy.
Most randomized clinical trials have enrolled few elderly patients, despite the fact that elderly patients constitute a large portion of the population. Elderly patients are often screened by strict inclusion criteria, because they poorly represent the average patient due to the presence of significant comorbid conditions (3, 4).
Renal dysfunction is a well-known poor prognostic factor after PCI (5-7). Previous studies have shown that PCI in patients with renal dysfunction is associated with poor clinical outcomes, such as lower procedural success rates, higher rates of in-hospital major adverse cardiac events (MACE), and worse clinical outcomes (8, 9). As a result, patients with renal dysfunction also have been excluded in most clinical studies, and available data from these clinical studies provides little information about elderly patients with renal dysfunction. Therefore, there are unresolved questions concerning benefits of PCI in elderly AMI patients with renal dysfunction.
The aims of this study were to evaluate the effects of PCI on the incidence of short- and long-term MACE in elderly AMI patients with renal dysfunction.
The Korea Acute Myocardial Infarction Registry (KAMIR) is a multicenter online registry designed to describe characteristics and clinical outcomes of patients with acute MI and reflects current management of patients with AMI in Korea. The registry included 52 community and university hospitals with capability of primary PCI. Data was collected at each site by a trained study coordinator based on standardized protocol retrospectively.
The registry included 13,901 consecutive patients who were admitted to the hospital between November 2005 and July 2008, whose discharge diagnosis was AMI based on cardiac enzymes and electrocardiographic findings. Patients who were lost to follow-up within one year of AMI as well as those with missing data were excluded. Overall, 12,636 patients (91% of the cohort) had all data available for the calculation of eGFR and constituted the final study sample. We analyzed elderly 1,458 AMI patients with renal dysfunction (GFR<60 mL/min) who received either medical (n=439) or PCI (n=1,019) therapy based on clinician discretion.
AMI, including both STEMI and non-STEMI was defined by clinical signs or symptoms: Patients were diagnosed with STEMI when they had new or presumed new ST-segment elevation of at least 1 mm seen in any location or new left bundle-branch block on the index or subsequent ECG with at least 1 positive cardiac biochemical marker of necrosis (including creatine kinase-MB and troponin I and T). Left ventricular ejection fraction (LVEF) was checked by 2-dimensional echocardiography at admission. Indices of global and segmental systolic and diastolic function were obtained. LVEF were determined using the Teicholz method or modified biplane Simpson's method (10).
Primary end point was death in hospital courses. Secondary end point was MACE that included cardiogenic death, myocardial infarction, and need for emergency or elective repeat revascularization, coronary artery bypass graft (CABG) during follow-up.
The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was used to estimate GFR in milliliters per minute per 1.73 m2 (11). The serum creatinine concentration was determined by the Jaffe method, which was calibrated to isotope dilution mass spectrometry (IDMS).
Baseline variables were age, sex, body mass index (BMI), coronary risk factor which included hypertension (defined as history of hypertension, admission blood pressure >140 mmHg systolic or >90 mmHg diastolic), current smoking, previous history of ischemic heart disease (IHD), hyperlipidemia (defined as history of hyperlipidemia, total cholesterol (TC) level of 240 mg/dL, or low density lipoprotein (LDL)-C level >101 mg/dL) and Killips class.
Use of certain medications was recorded on admission (aspirin, angiotensin converting enzyme inhibitor [ACEi], diuretics, statin, beta-blocker, nitrate or vasopressers). Surgical interventions (CABG, thrombolysis, or PCI) and coronary care unit (CCU) stay were recorded.
The records of cardiovascular risk factors and past history (age, sex, hypertension, hyperlipidemia, smoking, diabetes mellitus, family history of coronary heart disease, prior IHD) were dependent mainly on the patient's self-report, but the final records were left to the physician's discretion after he or she comprehensively considered the patient's self-report and the in-hospital examination results. All deaths were considered cardiac deaths if non-cardiac death could be excluded. Recurrent myocardial infarction was defined as recurrent symptoms with new ST-segment elevation or re-elevation of cardiac markers to at least twice the upper limit of normal. Target lesion revascularization (TLR) was defined as ischemia-induced PCI of the target lesion resulting from restenosis or reocclusion within the stent or in the adjacent 5 mm of the distal or proximal segment. Total major adverse cardiac events (MACEs) were defined as cardiogenic death, myocardial infarction, and need for emergency or elective repeat revascularization, coronary artery bypass graft (CABG) during follow-up.
Patients were required to visit the outpatient clinic of the cardiology department at the end of the first month, every 6 months after the PCI procedure, and when angina-like symptoms occurred. The various MACEs, in hospital and at 1-yr, were evaluated between the medical and PCI groups.
For continuous variables, differences between groups were evaluated by unpaired t test or Mann-Whitney rank-sum test. For discrete variables, differences were expressed as counts and percentages and were analyzed with χ2 (or Fisher exact) test between groups as appropriate. To adjust for potential confounders, a propensity score analysis was performed using the logistic regression model, testing the propensity to receive PCI rather than medical therapy. We tested all available variables that could be of potential relevance: age, sex, Killip class on admission, cardiovascular risk factors (hypertension, hyperlipidemia, smoking, diabetes mellitus, family history of coronary heart disease), prior myocardial infarction, number of diseased vessels, and cardiovascular medications (aspirin, clopidogrel, cilostazol, glycoprotein IIb/IIIa receptor blockers, heparins, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, β-blockers, calcium channel blockers, nitrate and statins). The logistic model by which the propensity score was estimated showed good predictive value (C statistic=0.734). Multivariable Cox regression analysis was then performed using the propensity score, medical therapy versus PCI and the aforementioned variables to determine the impact of the different therapies on short-term and long-term clinical outcomes. All continuous variables were described as mean±SD. All analyses were 2-tailed, with clinical significance defined as values of P<0.05. Statistical analysis was done with the Statistical Package for Social Sciences (SPSS) software version 17.0 for Windows (SPSS Inc. Chicago, USA).
The study was conducted according to the Declaration of Helsinki. The institutional review board of all participating centers approved the study protocol. The approval number was I-2008-1-009 of Chonnam National University Hospital. Written informed consent was obtained from all participating patients.
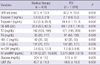
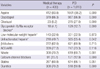
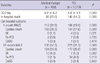
In all, 1,458 patients were included in the present study (439 in the medical therapy group and 1019 in the PCI group; ST-segment elevation myocardial infarction [STEMI]=53.9% and non-STEMI=46.1%). Table 1 lists the baseline characteristics of the patients, and Table 2 presents a summary of the biochemical parameters and left ventricular ejection fractions (LVEF) of the patients. As shown in Table 1, age, history of heart failure, and rate of ischemic heart disease (IHD) are higher in the medical group. In addition, GFR and LVEF were lower in the medical group (Table 2). Angiographic findings showed that the patients in the medical group were more likely to have type C lesions and three vessel disease (Table 3).
The in-hospital medications that were administered are listed in Table 4. Patients in the medical group were less likely to receive aspirin, clopidogrel, cilostazol, glycoprotein IIb/IIIa receptor blockers, and unfractionated heparin, and were more likely to receive nitrate, calcium channel blockers, and diuretics than those in the PCI group.
In-hospital clinical outcomes showed that the medical group exhibited a significantly higher incidence of in-hospital death than did the PCI group. In addition, short-term and long-term cardiac death and MACE rates were higher in the medical group than in the PCI group. In addition, the incidences of cardiac death and MI were higher in the medical group (Table 5). Multivariable Cox regression analysis using the propensity score method showed higher odds ratios for MACE-free survival in the PCI group, before and after adjustments using the propensity score (Table 6, Fig. 1).
The main findings of this study were that PCI effectively reduced in-hospital, short-term, and long-term MACE rates in elderly AMI patients with renal dysfunction. The MACE rate in elderly patients was not significantly higher if successful reperfusion was achieved.
Prior studies reported that PCI achieved favorable outcomes in patients not suited for thrombolysis (12-15). Our findings corroborated these reports, demonstrating that PCI could decrease cardiac mortality in elderly AMI patients with renal dysfunction. The fact that 1-month and 12-month MACE rates in the PCI group were significantly lower highlights the impact of primary PCI even in older patients with AMI and even in renal dysfunction. We suggest that aggressive PCI, even in older patients with renal dysfunction, can improve prognosis, and support the view that primary PCI should not be withheld because of age and renal function.
There are several possible reasons why older patients continue to experience high mortality rates. First, older patients have a higher incidence of comorbid conditions, such as hypertension, diabetes, atherosclerosis, prior stroke, and renal dysfunction. Renal dysfunction, in particular, has negatively affected outcomes of patients with AMI (16). Moreover, a number of other comorbid conditions, such as prior stroke, may have an additional role in poor prognosis. Second, elderly patients tend to have a greater delay in door-to-balloon time (17) which is significantly associated with increased mortality. A strong relationship has been reported between door-to-balloon time and in-hospital mortality (18-21). The relationship between door-to-balloon time and prognosis elucidates the need for a process specifically aimed at reducing the delay in rapid initiation of primary PCI. Third, elderly patients with renal dysfunction have been shown to have an increased incidence of PCI-related complications. In the case of cardiogenic shock, both increased age and renal dysfunction were important prognostic factors (22, 23). There was a higher incidence of contrast-induced (24) and bleeding complications in elderly patients with renal dysfunction (25).
In our study, the medical therapy group exhibited higher mean age, and significantly higher incidences of diabetes, hyperlipidemia, IHD history, and non-ST-segment elevation myocardial infarction. Coronary angiographic findings revealed significantly higher incidences of left main stem involvement, complex disease, and multivessel disease in the medical therapy group. In hospital medication, there was significantly lower usage of aspirin, clopidogrel, unfractionated heparin, and glycoprotein IIb/IIIa receptor blocker in the medical therapy group. These characteristics of the medical therapy group may increase poor outcomes in in-hospital death, and 1-month and 12-month MACE, and the rate of poor outcomes did not change after Cox regression analysis using the propensity score method. Compared with the medical therapy group, PCI decreased 1-month MACE by 33% and 12-month MACE by 39% in elderly patients with renal dysfunction.
In practice, PCI effectively decreased mortality and morbidity in AMI settings and improved short-term and long-term prognosis. However, the beneficial effect of PCI has been limited to younger people, because primary PCI in elderly patients with renal dysfunction carries an increased procedural risk. Physicians tend to hesitate when deciding whether to reperfuse by PCI or treat medically, especially in cases involving elderly AMI patients with renal dysfunction. However, our result demonstrated a beneficial effect of PCI even in elderly patients with renal dysfunction. Although PCI carries an increased procedural risk in elderly patients with renal dysfunction, the benefits after PCI can outweigh the procedural hazards in most patients with AMI, owing to improvements in PCI technology.
The present study has some limitations. First, although this study included a large number of subjects, there were baseline differences in several important prognostic factors between the primary comparison groups. These differences can be attributed to the fact that the study was not a prospective, randomized study. Although most confounders were included in the multivariable Cox regression model, including propensity scores to control baseline bias, some potential confounders may have been overlooked. Since we cannot fully understand why a physician would select a particular treatment strategy, we may have overlooked specific reasons based on which the physicians chose PCI or medical therapy. Second, in the KAMIR registry, there is no written information about hemodialysis, contrast-induced nephropathy, or postprocedural bleeding. Therefore, we could not evaluate the effect of these factors on the incidence of MACE. Third, clinical follow-up data were available for only 1 yr; a longer evaluation period will be needed to confirm our findings.
In conclusion, in elderly patients with AMI and renal dysfunction, PCI therapy yielded favorable in-hospital, short-term, and long-term MACE-free survival rates. Thus, even in very old patients with renal dysfunction, PCI should be considered in appropriate clinical settings.
Figures and Tables
ACKNOWLEDGMENTS
Korea Acute Myocardial infarction Registry (KAMIR) Investigators: Myung Ho Jeong, MD, Young Keun Ahn, MD, Sung Chull Chae, MD, Jong Hyun Kim, MD, Seung Ho Hur, MD, Young Jo Kim, MD, In Whan Seong, MD, Dong Hoon Choi, MD, Jei Keon Chae, MD, Taek Jong Hong, MD, Jae Young Rhew, MD, Doo Il Kim, MD, In Ho Chae, MD, Jung Han Yoon, MD, Bon Kwon Koo, MD, Byung Ok Kim, MD, Myoung Yong Lee, MD, Kee Sik Kim, MD, Jin Yong Hwang, MD, Myeong Chan Cho, MD, Seok Kyu Oh, MD, Nae Hee Lee, MD, Kyoung Tae Jeong, MD, Seung Jea Tahk, MD, Jang Ho Bae, MD, Seung Woon Rha, MD, Keum Soo Park, MD, Chong Jin Kim, MD, Kyoo Rok Han, MD, Tae Hoon Ahn, MD, Moo Hyun Kim, MD, Ki Bae Seung, MD, Wook Sung Chung, MD, Ju Young Yang, MD, Chong Yun Rhim, MD, Hyeon Cheol Gwon, MD, Seong Wook Park, MD, Young Youp Koh, MD, Seung Jae Joo, MD, Soo Joong Kim, MD, Dong Kyu Jin, MD, Jin Man Cho, MD, Byung Ok Kim, MD, Sang-Wook Kim, MD, Jeong Kyung Kim, MD, Tae Ik Kim, MD, Deug Young Nah, MD, Si Hoon Park, MD, Sang Hyun Lee, MD, Seung Uk Lee, MD, Hang-Jae Chung, MD, Jang Hyun Cho, MD, Seung Won Jin, MD, Yang Soo Jang, MD, Jeong Gwan Cho, MD, and Seung Jung Park, MD.
Notes
This research was supported by a grant from the Ministry of Science & Technology (MoST)/Korea Science & Engineering Foundation (KOSEF) (2010-0021808) and by the Korea Science and Engineering Foundation through the Medical Research Center for Gene Regulation grant (2012-0009448) at Chonnam National University.
References
1. Eagle KA, Nallamothu BK, Mehta RH, Granger CB, Steg PG, Van de Werf F, López-Sendón J, Goodman SG, Quill A, Fox KA. Trends in acute reperfusion therapy for ST-segment elevation myocardial infarction from 1999 to 2006: we are getting better but we have got a long way to go. Eur Heart J. 2008; 29:609–617.
2. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003; 361:13–20.
3. Jhun HJ, Kim H, Cho SI. Time trend and age-period-cohort effects on acute myocardial infarction mortality in Korean adults from 1988 to 2007. J Korean Med Sci. 2011; 26:637–641.
4. Sakai K, Nakagawa Y, Soga Y, Ando K, Yokoi H, Iwabuchi M, Yasumoto H, Nosaka H, Nobuyoshi M. Comparison of 30-day outcomes in patients <75 years of age versus >or=75 years of age with acute myocardial infarction treated by primary coronary angioplasty. Am J Cardiol. 2006; 98:1018–1021.
5. Na KY, Kim CW, Song YR, Chin HJ, Chae DW. The association between kidney function, coronary artery disease, and clinical outcome in patients undergoing coronary angiography. J Korean Med Sci. 2009; 24:S87–S94.
6. Nikolsky E, Mehran R, Turcot D, Aymong ED, Mintz GS, Lasic Z, Lansky AJ, Tsounias E, Moses JW, Stone GW, et al. Impact of chronic kidney disease on prognosis of patients with diabetes mellitus treated with percutaneous coronary intervention. Am J Cardiol. 2004; 94:300–305.
7. Best PJ, Lennon R, Ting HH, Bell MR, Rihal CS, Holmes DR, Berger PB. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002; 39:1113–1119.
8. Bae EH, Lim SY, Cho KH, Choi JS, Kim CS, Park JW, Ma SK, Jeong MH, Kim SW. GFR and cardiovascular outcomes after acute myocardial infarction: results from the Korea Acute Myocardial Infarction Registry. Am J Kidney Dis. 2012; 59:795–802.
9. Choi JS, Kim CS, Park JW, Bae EH, Ma SK, Jeong MH, Kim YJ, Cho MC, Kim CJ, Kim SW. Renal dysfunction as a risk factor for painless myocardial infarction: results from Korea Acute Myocardial Infarction Registry. Clin Res Cardiol. 2012; 101:795–803.
10. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography: American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989; 2:358–367.
11. Skali H, Uno H, Levey AS, Inker LA, Pfeffer MA, Solomon SD. Prognostic assessment of estimated glomerular filtration rate by the new Chronic Kidney Disease Epidemiology Collaboration equation in comparison with the Modification of Diet in Renal Disease Study Equation. Am Heart J. 2011; 162:548–554.
12. Mehta RH, Sadiq I, Goldberg RJ, Gore JM, Avezum A, Spencer F, Kline-Rogers E, Allegrone J, Pieper K, Fox KA, et al. Effectiveness of primary percutaneous coronary intervention compared with that of thrombolytic therapy in elderly patients with acute myocardial infarction. Am Heart J. 2004; 147:253–259.
13. Thiemann DR, Coresh J, Schulman SP, Gerstenblith G, Oetgen WJ, Powe NR. Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years. Circulation. 2000; 101:2239–2246.
14. Itoh T, Fukami K, Suzuki T, Kimura T, Kanaya Y, Orii M, Goto I, Matsui H, Sugawara S, Nakajima S, et al. Comparison of long-term prognostic evaluation between pre-intervention thrombolysis and primary coronary intervention: a prospective randomized trial: five-year results of the IMPORTANT Study. Circ J. 2010; 74:1625–1634.
15. De Boer MJ, Ottervanger JP, van 't Hof AW, Hoorntje JC, Suryapranata H, Zijlstra F. Zwolle Myocardial Infarction Study Group. Reperfusion therapy in elderly patients with acute myocardial infarction: a randomized comparison of primary angioplasty and thrombolytic therapy. J Am Coll Cardiol. 2002; 39:1723–1728.
16. Saltzman AJ, Stone GW, Claessen BE, Narula A, Leon-Reyes S, Weisz G, Brodie B, Witzenbichler B, Guagliumi G, Kornowski R, et al. Long-term impact of chronic kidney disease in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: the HORIZONS-AMI (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction) Trial. JACC Cardiovasc Interv. 2011; 4:1011–1019.
17. Sakai K, Nagayama S, Ihara K, Ando K, Shirai S, Kondo K, Yokoi H, Iwabuchi M, Nosaka H, Nobuyoshi M. Primary percutaneous coronary intervention for acute myocardial infarction in the elderly aged ≥75 years. Catheter Cardiovasc Interv. 2012; 79:50–56.
18. Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008; 51:210–247.
19. McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006; 47:2180–2186.
20. Nallamothu BK, Bradley EH, Krumholz HM. Time to treatment in primary percutaneous coronary intervention. N Engl J Med. 2007; 357:1631–1638.
21. Yasuda S, Shimokawa H. Acute myocardial infarction: the enduring challenge for cardiac protection and survival. Circ J. 2009; 73:2000–2008.
22. Tomassini F, Gagnor A, Migliardi A, Tizzani E, Infantino V, Giolitto S, Conte MR, Lanza GA, Gnavi R, Varbella F. Cardiogenic shock complicating acute myocardial infarction in the elderly: predictors of long-term survival. Catheter Cardiovasc Interv. 2011; 78:505–511.
23. Lim SY, Jeong MH, Bae EH, Kim W, Kim JH, Hong YJ, Park HW, Kang DG, Lee YS, Kim KH, et al. Predictive factors of major adverse cardiac events in acute myocardial infarction patients complicated by cardiogenic shock undergoing primary percutaneous coronary intervention. Circ J. 2005; 69:154–158.
24. Caruso M, Balasus F, Incalcaterra E, Ruggieri A, Evola S, Fattouch K, Bracale UM, Amodio E, Novo G, Andolina G, et al. Contrast-induced nephropathy after percutaneous coronary intervention in simple lesions: risk factors and incidence are affected by the definition utilized. Intern Med. 2011; 50:983–989.
25. Lopes RD, Subherwal S, Holmes DN, Thomas L, Wang TY, Rao SV, Magnus Ohman E, Roe MT, Peterson ED, Alexander KP. The association of in-hospital major bleeding with short-, intermediate-, and long-term mortality among older patients with non-ST-segment elevation myocardial infarction. Eur Heart J. 2012; 33:2044–2053.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download