INTRODUCTION
There is increasing uncertainty about the effectiveness of new medical technologies that are rapidly implemented in clinical practice.
Variations in the medical practices such as surgery rate, admission rate, and medication dosage rate are unexplained; however, there is insufficient scientific evidence to reconcile these variations.
Regarding healthcare spending, the need to induce proper behavior by healthcare providers is emerging because decisions by physicians have considerable discretion.
CLINICAL PRACTICE GUIDELINES IN GENERAL
Effects on healthcare practice
-
Many previous studies examined whether clinical practice guidelines contribute to promoting appropriate medical care. The majority of studies suggest clinical practice guidelines have a positive effect. A survey by the American College of Physicians (ACP) showed that 60% of the members felt that clinical practice guidelines had positive effects on decisions by physicians (5). In another example, the study on the effectiveness of guidelines for upper respiratory infection treatments showed that clinical practice guideline-driven treatment reduced the dosage of antibiotics, while the symptom reduction times of the test and control groups were similar (6).
The results of evaluation of the effectiveness of clinical practice guidelines for treating cystitis have shown that the urinalysis rate, urine culture rate, number of hospital visits of the patients subjected to clinical practice guidelines were reduced, and the dosage rate of antibiotics recommended by clinical practice guidelines were increased (7). -
The effects of clinical practice guidelines differ with the participation level of physicians and the contents of clinical practice guidelines (8).
The effectiveness of clinical practice guidelines can differ by the policies and environment of the hospitals at which the physicians work. When an institution initiates a hospital-wide program that evaluates physician performance based on guidelines and recommends the use of clinical practice, physicians often resorted to the use of clinical practice guidelines in actual practice.
Implementation of clinical practice guidelines resulted in reduced medical care costs as well as improved health outcomes. Based on a study on the economic benefits of clinical practice guidelines for stroke patients, patients who were treated according to clinical practice guidelines incurred lower treatment costs than others and a tangible reduction in the use of hospital resources. The patients treated with the clinical practice guidelines had improved life expectancy and the degree of disability was less severe.
The result is that clinical practice guidelines benefit doctors, patients, and clinical researchers. Clinical practice guidelines improve the quality of medical decisions during treatment and, clinical practice guidelines facilitate the improvement of health outcomes through the promotion of proven and effective treatments and the avoidance of ineffective treatments.
Methods of development
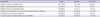
Activities in developed countries
The development of clinical practice guidelines are connected to policies of that improve the quality of healthcare.
An evidence based approach is used to develop most clinical practice guidelines.
Development of clinical practice guidelines is tightly linked to implementation and dissemination strategies.
CURRENT STATUS OF CLINICAL PRACTICE GUIDELINES IN KOREA
Characteristics of Korean clinical practice guidelines
Dissemination and implementation of clinical practice guidelines
Problems in developing clinical practice guidelines in Korea
There is a lack of interdisciplinary approaches to develop clinical practice guidelines.
There is an intention to use and evidence based approach; however, guidelines that detail rigorous evidence based approaches are scarce.
They want reflect the situations in Korea; however, it is not possible due to insufficient domestic research.
Recommendations are made through a consensus of experts with an unclear connection between recommendations and evidence.
Within development groups, there were limited methodologists with detailed techniques (19).




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download