Abstract
The number of HIV-infected individuals susceptible to Hepatitis A virus (HAV) infection is increasing in Korea; however, it has proven difficult to devise a vaccination policy therefore because limited seroepidemiologic data exists for them. Accordingly, anti-HAV IgG was measured in 188 HIV-infected adults between July 2008 and July 2010. The nadir CD4+ T lymphocyte counts were not different between the HAV-positive and -negative groups (197 ± 138 vs 202 ± 129, P = 0.821). The only factor independently associated with seropositive status was age under 40 yr old (OR 0.017, P < 0.001). Our findings suggest that HAV vaccination in HIV-infected adults should be targeted at persons under the age of 40 yr.
Worldwide seroprevalence estimates for the hepatitis A virus (HAV) suggest that middle-income regions in Asia, Latin America, Eastern Europe, and the Middle East have an intermediate or low level of endemicity, but a high proportion of susceptible adults due to rapid improvements in sanitation and living standards (1). Symptomatic HAV infections have been rapidly increasing in these countries (including the Republic of Korea), especially in the young adult population (1, 2). HAV infection in the young adult population has clinical importance because it can cause death by fulminant hepatic failure or acute kidney injury (3, 4).
Several outbreaks of symptomatic HAV infections have been reported among injecting drug users and men who have sex with men (MSM) (5, 6). The spread of HAV infection may occur in HIV-infected individuals because of shared transmission routes (7). Therefore, it is important that a policy for HAV vaccination in HIV-infected individuals should be introduced according to the seroepidemiological status of each country or region. However, data for clinical factors associated with HIV seropositivity in HIV-infected adults are unclear as to whether a corresponding vaccination policy for non-HIV infected persons can be equally applied to those infected with HIV. The objective of this study was to determine the clinical factors associated with seropositive status for HAV in HIV-infected adults living in a country with recent epidemiological shifts and use them to guide the development of vaccination policies.
Anti-HAV immunoglobulin G (IgG) antibody measurements using chemiluminescence immunoassay (VITROS® 3600, Ortho Clinical Diagnostics, Wycombe, UK) were taken in 188 HIV-infected adults between July 2008 and July 2010 at Severance Hospital, a 2000-bed, university-affiliated tertiary care hospital in Seoul, Republic of Korea. All adults over the age of 20 were eligible, irrespective of age and/or combined antiretroviral treatment (cART). However, HIV-infected individuals with the following conditions were excluded: 1) transfer from other medical centers, excluding public health centers, and 2) past history of adult booster vaccination against HAV (given to those over the age of 18). To compare differences in HAV seropositivity according to age in the young age group, we analyzed HAV IgG serology data obtained during regular health check-ups that were performed in May 2010 in non-HIV-infected health care workers who were less than 35 yr of age. Among the 1,191 health care workers, only data from the 816 individuals who had never received an adult booster vaccination against HAV were included. We identified HAV booster history through the review of medical records and history taking. This retrospective study received ethical approval from the Institutional Review Board of our institution, and the need for written informed consent was waived, because the design of the study posed no risk to the subjects' rights or welfare.
We retrospectively collected epidemiological, immunological, and virologic data, concerning mode of transmission, Centers for Disease Control and Prevention (CDC) categories, CD4+ T lymphocyte count and plasma HIV-RNA viral load (VL), through a review of the electronic medical records of HIV-infected individuals. The CDC disease classifications as revised in 1993 were used (8). We used the plasma HIV-RNA VL within 6 months before cART initiation with logarithmic transformation to exclude the association between age and VL.
Data were expressed as numbers (%), mean ± standard deviation (SD) or median (interquartile ranges). We used Student's t-test or Mann-Whitney U test for continuous variables and the chi-square test or Fisher's exact test for categorical/nominal variables to compare the characteristics between the anti-HAV IgG positive and negative groups. Multivariate logistic regression analysis was performed using the variables which had P values of less than 0.10 in the univariate analysis to identify clinical factors associated with HAV seropositivity in HIV-infected adults. The final regression model was expressed as odds ratios (OR) and 95% confidential intervals (CIs). All P values were two-tailed, and P < 0.05 was considered to be statistically significant. SPSS 18.0 software (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
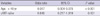
A total of 118 (62.8%) of 188 HIV-infected adults were seropositive for HAV. According to age group, the seropositive rates were 0% (< 25 yr), 14.3% (≥ 25 and < 30 yr), 37.5% (≥ 30 and < 35 yr), 67.6% (≥ 35 and < 40 yr), 97.0% (≥ 40 and < 45 yr), and 97.7% (≥ 45 yr). Individuals in the anti-HAV IgG positive group were older (44 ± 8 vs 31 ± 6 yr, P < 0.001) than those in the negative group. However, the nadir CD4+ T lymphocyte counts and log10[plasma HIV-RNA VL within 6 months before cART initiation] were similar between the HAV positive and negative groups (197 ± 138 vs 202 ± 129, P = 0.821, 4.94 [4.36-5.51] vs 4.94 [4.35-5.43], P = 0.974, respectively). The rate of cART-naïve individuals was significantly lower in the HAV seropositive group (7.6% vs 17.1%, P = 0.045) (Table 1).
In the multivariate final logistic regression model, age less than 40 yr old (OR 0.017, 95% CI 0.004-0.075, P < 0.001) was the only factor independently associated with anti-HAV IgG seropositive status (Table 2).
The seropositive rate between HIV-infected adults and non-HIV-infected health care workers was not significantly different in either the under 30 age group or the 30-35 age group (8.8% vs 11.9%, P = 0.786 and 37.5% vs 26.1%, P = 0.183, respectively).
The CDC currently recommends vaccination against HAV in all HIV-infected adults at a high risk of HAV infection, including MSM and intravenous (IV) drug abusers, irrespective of age and CD4+ T lymphocyte count (9). However, a few studies have reported that the immunogenecity for the hepatitis A vaccine was poor in HIV-infected adults with low CD4+ T lymphocyte count (10, 11). Also, the seropositive rate for HAV differs according to age and world region in the general global population (1). Therefore, policies for HAV vaccination in HIV-infected adults should be tailored according to age, country, and immune status.
Ida et al. (12) reported that load and duration of HAV viremia was significantly higher and longer in HIV-infected patients than in non-HIV-infected patients. In addition, HIV-infected patients had lower elevations in alanine aminotransferase than did non-HIV-infected patients. They suggested that the prolonged HAV viremia in HIV-infected patients might cause a long outbreak of HAV infection in MSM (12). The prolonged HAV viremia in HIV-infected patients was described as a case report in 2002 (13). Therefore, effective HAV vaccination may prevent the outbreak of HAV infection in HIV-infected patients carry out high-risk behaviors including MSM or IV drug abusers.
In the Republic of Korea, as in many developed countries and metropolitan communities, symptomatic HAV infections have generally shifted from children to older adults (2). Although the seroepidemiology of HAV has been reported in various non-HIV-infected groups, there is little data for HIV-infected adults (14-16).
This study hypothesized that immune status, evaluated according to CD4+ T lymphocyte count, may affect the seropositivity of HAV IgG in HIV-infected Koreans. In particular, we presumed that HIV-infected patients with lower CD4+ T lymphocyte counts will have a lower seropositivity of HAV IgG. However, our results did not reveal an association of CD4+ T lymphocyte counts with seropositivity of HAV IgG.
In this study, we confirmed that HIV-infected adults who were younger, especially less than 35 yr old, had low HAV seropositivity, similar to the non-HIV-infected general population (2, 15). There were no differences in HAV seropositivity in the under 35 age group, with low rates of less than 50%, among both HIV-infected and non-HIV-infected adults. Our study revealed that HAV seropositivity in HIV-infected Koreans was not associated with immunologic and virologic status, which were evaluated by nadir CD4+ T lymphocyte counts and plasma HIV-RNA VL at 6 months before cART initiation. If HIV-infected adults living in countries which have experienced epidemiological shifts similar to Republic of Korea are young, clinicians should consider vaccination against HAV. The seropositive rate of HAV and the age association in this study were similar to results from a Taiwanese study (7). However, HIV transmission due to drug use is very rare in the Republic of Korea, unlike Taiwan (17).
Our findings suggest that, in HIV-infected adults, HAV vaccination should be targeted at younger individuals, especially those less than 40 yr of age, irrespective of nadir CD4 + T lymphocyte count or plasma HIV-RAN VL before cART initiation.
Figures and Tables
Table 1
Comparison of clinical characteristics between anti-HAV IgG positive and negative HIV-infected individuals

The data are expressed as number (percent), mean ± standard deviation or median (interquartile ranges). *Comparisons between the anti-HAV IgG positive and negative group; †Fisher's Exact Test; ‡Independent Student's t-test; §Chi-square tests; ∥Mann-Whitney U test. HAV, hepatitis A virus; IgG, immunoglobulin G; CDC, Centers for Disease Control and Prevention; VL, viral load; cART, combined antiretroviral treatment.
References
1. Jacobsen KH, Wiersma ST. Hepatitis A virus seroprevalence by age and world region, 1990 and 2005. Vaccine. 2010. 28:6653–6657.
2. Kim YJ, Lee HS. Increasing incidence of hepatitis A in Korean adults. Intervirology. 2010. 53:10–14.
3. Jung YM, Park SJ, Kim JS, Jang JH, Lee SH, Kim JW, Park YM, Hwang SG, Rim KS, Kang SK, et al. Atypical manifestations of hepatitis A infection: a prospective, multicenter study in Korea. J Med Virol. 2010. 82:1318–1326.
4. Choi HK, Song YG, Han SH, Ku NS, Jeong SJ, Baek JH, Kim H, Kim SB, Kim CO, Kim JM, et al. Clinical features and outcomes of acute kidney injury among patients with acute hepatitis A. J Clin Virol. 2011. 52:192–197.
5. Dabrowska MM, Nazzal K, Wiercinska-Drapalo A. Hepatitis A and hepatitis A virus/HIV coinfection in men who have sex with men, Warsaw, Poland, September 2008 to September 2009. Euro Surveill. 2011. 16:19950.
6. Spada E, Genovese D, Tosti ME, Mariano A, Cuccuini M, Proietti L, Giuli CD, Lavagna A, Crapa GE, Morace G, et al. An outbreak of hepatitis A virus infection with a high case-fatality rate among injecting drug users. J Hepatol. 2005. 43:958–964.
7. Sun HY, Kung HC, Ho YC, Chien YF, Chen MY, Sheng WH, Hsieh SM, Wu CH, Liu WC, Hung CC, et al. Seroprevalence of hepatitis A virus infection in persons with HIV infection in Taiwan: implications for hepatitis A vaccination. Int J Infect Dis. 2009. 13:e199–e205.
8. CDC. 1993 revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Recomm Rep. 1992. 41:1–19.
9. CDC. Recommended adult immunization schedule: United States, 2011. MMWR Morb Mortal Wkly Rep. 2011. 60:1–4.
10. Launay O, Grabar S, Gordien E, Desaint C, Jegou D, Abad S, Girard PM, Belarbi L, Guerin C, Dimet J, et al. Immunological efficacy of a three-dose schedule of hepatitis A vaccine in HIV-infected adults: HEPAVAC study. J Acquir Immune Defic Syndr. 2008. 49:272–275.
11. Shire NJ, Welge JA, Sherman KE. Efficacy of inactivated hepatitis A vaccine in HIV-infected patients: a hierarchical bayesian meta-analysis. Vaccine. 2006. 24:272–279.
12. Ida S, Tachikawa N, Nakajima A, Daikoku M, Yano M, Kikuchi Y, Yasuoka A, Kimura S, Oka S. Influence of human immunodeficiency virus type 1 infection on acute hepatitis A virus infection. Clin Infect Dis. 2002. 34:379–385.
13. Costa-Mattioli M, Allavena C, Poirier AS, Billaudel S, Raffi F, Ferre V. Prolonged hepatitis A infection in an HIV-1 seropositive patient. J Med Virol. 2002. 68:7–11.
14. Jung SI, Lee CS, Park KH, Kim ES, Kim YJ, Kim GS, Lim DS, Moon JE, Min JJ, Bom HS, et al. Sero-epidemiology of hepatitis A virus infection among healthcare workers in Korean hospitals. J Hosp Infect. 2009. 72:251–257.
15. Lee D, Ki M, Lee A, Lee KR, Park HB, Kim CS, Yoon BY, Kim JH, Lee YS, Jeong SH. A nationwide seroprevalence of total antibody to hepatitis A virus from 2005 to 2009: age and area-adjusted prevalence rates. Korean J Hepatol. 2011. 17:44–50.
16. Lee H, Cho HK, Kim JH, Kim KH. Seroepidemiology of hepatitis A in Korea: changes over the past 30 years. J Korean Med Sci. 2011. 26:791–796.
17. Kee MK, Lee JH, Kim GJ, Choi BS, Hong KJ, Lee JS, Kim SS. Decrease of initial CD4+ T-cell counts at the time of diagnosis of HIV infection in Korea; 1988-2006. Int J STD AIDS. 2010. 21:120–125.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download