Abstract
The study aimed to identify the clinical characteristics of coexisting chronic lymphocytic thyroiditis (CLT) in papillary thyroid carcinoma (PTC) and to evaluate the influence on prognosis. A total of 1,357 patients who underwent thyroid surgery for PTC were included. The clinicopathological characteristics were identified. Patients who underwent total thyroidectomy (n = 597) were studied to evaluate the influence of coexistent CLT on prognosis. Among the total 1,357 patients, 359 (26.5%) had coexistent CLT. In the CLT group, the prevalence of females was higher than in the control group without CLT (P < 0.001). Mean tumor size and mean age in the patients with CLT were smaller than without CLT (P = 0.040, P = 0.047, respectively). Extrathyroidal extension in the patients with CLT was significantly lower than without CLT (P = 0.016). Among the subset of 597 patients, disease-free survival rate in the patients with CLT was significantly higher than without CLT (P = 0.042). However, the multivariate analysis did not reveal a negative association between CLT coexistence and recurrence. Patients with CLT display a greater female preponderance, smaller size, younger and lower extrathyroidal extension. CLT is not a significant independent negative predictive factor for recurrence, although presence of CLT indicates a reduced risk of recurrence.
Papillary thyroid carcinoma (PTC) is the most common form of thyroid cancer, and its incidence is rapidly increasing in many countries (1). Chronic lymphocytic thyroiditis (CLT) is the most common inflammatory disorder of the thyroid gland. Although the frequency of CLT varies widely from 0.5%-38%, the coexistence of CLT and PTC has been reported in several studies since first reported in 1955 (2-6).
The prevalence of CLT in patients with PTC has been reported to be significantly higher than with benign thyroid tumors (5). Patients with CLT are believed to be at higher risk for PTC compared with patients without CLT (7). The presence of CLT in patients with PTC has been associated with better prognostic outcome, lower recurrence rate and less aggressive disease at the time of surgery (3, 4, 8-10). However, it has been conversely reported that the coexistence of CLT has no protective effect on patient outcome (11). Thus, the pathogenesis and prognostic outcome of the coexistence of PTC and CLT remains controversial.
A number of investigators have reported that clinicopathologic factors, including age, gender, tumor size, multi-focality, capsular invasion, extrathyroidal extension and lymph node (LN) metastasis are related to the prognosis of PTC (12-14). To investigate that coexistent CLT might contribute to a better prognosis in patients with PTC, the present study was undertaken to evaluate the prevalence of coexistent CLT in a population of PTC patients firstly and determine the association, if any, of CLT with clinicopathological parameters that are indicative of better prognosis at the time of initial diagnosis secondarily. The final goal of the study was to determine whether CLT is an independent risk factor for the prognosis of PTC.
Patients with PTC who underwent thyroid surgery between January 2005 and December 2006 at Yonsei University Hospital, Seoul, Korea were enrolled. All patients underwent pre-operative ultrasonography and fine needle aspiration cytology (FNAC) of the primary tumor, and were diagnosed with PTC pathologically. Of these patients, excluding patients with another subtype of thyroid carcinoma and a variant of PTC, and patients who had been diagnosed with CLT or any thyroid disease before being diagnosed with PTC were also excluded to prevent selection bias, because they had more opportunity for early detection of PTC that could lead to better treatment outcomes. A total 1,357 patients who received initial treatment for PTC at our institution and whose medical records were accessible for review as included in the first study arm to identify clinical characteristics of coexistent CLT in PTC patients at the time of surgery.
Among these 1,357 patients, those who were lost to follow-up, who had a history of the coexistence of another cancer, and who revealed lateral neck LN metastasis or distant metastasis at the time of surgery were excluded. Five hundred ninety seven consecutive patients with PTC who underwent total thyroidectomy with prophylatic ipsilateral central compartment node dissection followed by immediate 131I remnant ablation were enrolled in the second study arm to evaluate the influence on prognostic outcome of coexistent CLT in PTC patients.
Patient data were collected by retrospective medical record review. Patient demographics (age and gender), histopathological findings (tumor size, extrathyroidal extension, multifocality, LN metastasis and presence of CLT), preoperative laboratory finding (thyroid stimulating hormone [TSH], anti-thyroglobulin [Tg] autoantibody and anti-microsomal autoantibody) and clinical outcomes (loco-regional recurrences and distant metastasis) were analyzed. Pathologic staging was defined according to the Tumor, LN, and Metastasis (TNM) classification system based on the 6th edition of the UICC/AJCC TNM classifications. In addition, two well-established prognosis classification systems of differentiated thyroid cancer - the low/high risk group determination based on the Age, Metastasis, Extent of disease, Size (AMES) stage system (15) and the Metastasis, Age at presentation, Completeness of surgical resection, Invasion (extrathyroidal extension), Size (MACIS) formula-based scoring system (16) - were used to analyze various clinicopathological parameters. The systems have established that high scores are strongly correlated with a poor prognosis. Serum anti-microsomal and anti-Tg antibody analysis was performed by radioimmunoassay with commercial kits (Brahms, Berlin, Germany). TSH level was determined by an immunoradiometric assay (Coat-ACount, TSH IRMA; DPC, Los Angeles, CA, USA). The analytical sensitivity of the assay for anti-microsomal antibody, anti-Tg and TSH was 5.5, 5.5, and 0.3 IU/mL, respectively. The intraassay coefficients of variation ranged from 2.9%-4.5%, 2.0%-7.5%, and 1.9%-5.8%, respectively. The reference ranges for both anti-microsomal antibody and antithyroglobulin were < 60 IU/mL and for TSH 0.3-5.0 mL/L.
The diagnosis of CLT was obtained from a review of the pathologic slides by one pathologist. Pathologically proven CLT was defined as the presence of diffuse lymphoplasmacytic infiltrate, oxyphilic cells, formation of lymphoid follicles with germinal centers and atrophic changes in the area of normal thyroid tissue. Only peri-tumoral lymphocytic infiltration was not considered as CLT (2, 3, 9, 17).
At our institution, thyroid resection consisted of total thyroidectomy and less than total thyroidectomy. The definition of "less than total thyroidectomy" is specified by unilateral thyroid lobectomy, ipsilateral total and contralateral partial thyroidectomy, and ipsilateral total and contralateral subtotal thyroidectomy. Thyroid lobectomy with isthmusectomy was performed only when the following criteria were met: the cancer was an intrathyroidal, unifocal micro-carcinoma (< 1 cm), with no cervical lymph node involvement. In other cases, total thyroidectomy was performed. Ipsilateral central compartment node dissection was performed in all cases. If the patients have evidence of lateral lymph node metastasis in preoperative evaluation, Modified radical neck dissection was performed. The choice of surgical extension was based on ATA guidelines (18). During thyroid resection, only central compartment lymph nodes (CCLN) located in the ipsilateral site of the primary tumor were dissected prophylatically. The CCLN or level VI included the pretracheal, paratracheal, prelaryngeal, perithyroidal nodes, and lymph nodes located along the recurrent laryngeal nerve. The central compartment was delimited superiorly by the hyoid bone, inferiorly by the substernal notch, laterally by the median portion of the carotid sheath, and dorsally by the prevertebral fascia. Recurrent laryngeal nerves and parathyroid glands were identified and preserved in all cases. The procedures were performed by the same surgical team. If patients had evidence of lateral LN metastasis in preoperative evaluation, modified radical neck dissection was performed. Radioactive iodine remnant ablation was performed within 6 weeks after surgery. Indication for radioiodine ablation in this cohort of patients was based on ATA guidelines (18). A 131I whole body scan was taken on day 2 following radioiodine therapy. All patients received thyroid-stimulating hormone suppression treatment with levothyroxine according to ATA guidelines. Patient follow-up was based on physical examination, neck ultrasound (US), and serum Tg measurement at intervals of 3 or 6 months.
Statistical analysis was performed using SPSS (version 14.0; SPSS, Chicago, IL, USA). Continuous data are represented as mean ± standard deviation. To compare continuous variables, age, tumor size and mean, MACIS scores according to CLT status were tested using an independent t-test. The association between CLT (present or absent) and prognostic variables was assessed using a chi-squared test or Fisher's exact test for gender, extrathyroidal extension, multifocality, LN metastasis, TNM and AMES stage. The Kaplan-Meyer method with a log-rank test was used to account for recurrence and disease free rates during the follow-up period. Statistically significant variables based on univariate analysis were included in a multivariate analysis using a binary logistic regression test. With regard to the results, P values were two-sided throughout and the statistical significance was defined as P < 0.05.
Among the 1,357 patients, there were 181 men and 1,176 women. Mean age was 45.53 yr. The mean tumor size was 1.08 ± 0.77 cm. Multifocality, extrathyroidal extension and LN metastasis were detected in 450 (33.2%), 752 (55.4%) and 619 patients (45.6%), respectively. Three hundred fifty nine (26.5%) of 1,357 patients with PTC had co-existing CLT. Based on univariate analysis, the mean age of patients with and without CLT was 44.50 ± 10.65 and 45.90 ± 11.68 yr, respectively (P = 0.047). Predominance of female gender was observed in patients with CLT compared to patients without CLT (P = 0.001). The mean tumor size was smaller in patients with CLT than patients without CLT (1.01 ± 0.66 cm vs 1.10 ± 0.81 cm, respectively; P = 0.040). The prevalence of extrathyroidal extension was higher in patients without CLT (P = 0.016). There was no statistically significant difference in the prevalence of operation methods, multifocality and TNM stage between the two groups (P = 0.094, 0.845, and 0.781, respectively). The rate of total LN metastasis was not significantly different in patients with and without CLT patients (P = 0.294). There was no difference in the prevalence of central LN metastasis and lateral LN metastasis between the two groups (P = 0.322 and 0.252, respectively). Table 1 summarizes the results of the univariate analyses.
The clinical and pathological parameters of the second study cohort are summarized in Table 2. When total thyroidectomy patients results were compared with the results from the total patient population, the prevalence of women and small tumor size were evident in the group of patients who had PTC with CLT (P = 0.001 and 0.035, respectively), although there was no difference in extrathyroidal extension and age between the two groups (P = 0.724 and 0.153, respectively). There was no difference in the prevalence of LN metastasis, multifocality and TNM stage between the two groups (P = 0.784, 0.316, and 0.620, respectively). However, LN metastasis ratio (metastatic LN number/dissected LN number) was lower in patients with CLT compared to patients without CLT (P = 0.001). The recurrence rate in the patients with CLT (1.5%) was lower than that in without CLT (5.0%) (P = 0.042).
Evaluation of the expected prognostic outcome using the AMES (15) clinical staging system and the MACIS scoring system (16) was also performed. With the AMES staging system, the proportion of high-risk group of patients with PTC alone was higher than that of patients with PTC and CLT (31.3% and 21.0%, respectively; P = 0.009). Using the MACIS scoring system, the proportion of the high-risk group of patients with PTC alone was also higher than that of patients with PTC and CLT. Patients with PTC alone exhibited a higher mean score (4.89 vs 4.74; P = 0.049) and a higher percentage (15.4% vs 7.2%) of the patients scoring ≥ 6 on the MACIS scoring system (P = 0.004; Table 3).
All patients in whom recurrence was suspected were confirmed using cytology and/or histology. During the mean 58-month follow-up period in the PTC with CLT group, three (1.5%) of 195 patients experienced recurrence and all of the recurrent diseases occurred at the ipsilateral lateral LN. Comprehensive neck dissection followed by high-dose radioactive iodine remnant ablation therapy was performed in all of these patients, and none have died at the time of the present evaluation. Of the patients in PTC without CLT with a mean 58-month follow-up period, a total of 20 (5.0%) have experienced recurrence, the main locations were the regional LN (18 patients; 3 patients = ipsilateral central LN, 15 patients = ipsilateral lateral LN), and 2 patients had distant lung metastasis. Comprehensive neck dissection followed by high-dose radioactive iodine remnant ablation therapy was performed in all of these patients, and none have died at the time of the present evaluation. Patients with PTC and CLT tended to have a better prognosis compared with that of patients with PTC alone. Disease free survival (DFS) rate in the patients with CLT was significantly higher than that without CLT during follow-up period (log-rank = 4.11, P = 0.042; Fig. 1). DFS was evaluated according to the presence or absence of LN metastasis at the time of surgery. Especially in PTC patients with central LN metastasis, DFS was significantly higher in patients with CLT compared with those without CLT (log-rank = 4.31, P = 0.038; Fig. 2).
We separately analyzed the outcomes for lower-risk group and high-risk groups by AMES stage and MACIS scoring systems. In lower-risk patients, DFS was significantly different in patients with CLT compared with those without CLT (P = 0.009 and P = 0.018, respectively). But, there were no significant differences in high-risk patients with CLT compared with those without CLT by AMES stage and MACIS scoring system (P = 0.778 and P = 0.456, respectively).
Based on univariate analysis, LN metastasis (P = 0.001, odds ratio [OR] = 9.676) and CLT (P = 0.042, OR = 0.298) were observed in patients with recurrence compared with patients without recurrence. However, gender (i.e., prevalence of females), extrathyroidal extension, age, tumor size and multifocality were not significantly different based on the univariate analysis between the two groups (Table 4). However, based on multivariate analysis, only LN metastasis (P = 0.001, OR = 9.278) was observed in patients with recurrence compared with patients without recurrence. The multivariate analysis did not show a negative association between the coexistence of CLT and recurrence.
We analyzed the CLT patients separately to evaluate the correlation between pathologic diagnosis and laboratory finding. CLT patients who were confirmed pathologically were divided into group A (anti-Tg Ab and anti-microsomal Ab were all negative) and group B (anti-Tg Ab positive or anti-microsomal Ab positive). In group A patients, CLT was confirmed by pathological examination but laboratory examination was negative, while CLT was confirmed in group B patients by pathological and laboratory examinations. The clinical and pathological parameters are summarized in Table 5. There was no statistically significant difference in age, gender, size, prevalence of extrathyroidal extension, multifocality, LN metastasis, TNM stage and recurrences between the two groups.
PTC is the most common cancer involving the thyroid gland, with a 10-yr relative survival rate of 93% (19). Although the prognosis for patients with PTC is excellent, patient age at diagnosis, stage of PTC, tumor size, presence of cervical node or distant metastasis, extrathyroidal extension, delay in diagnosis, extent of thyroidectomy and postoperative radioiodine ablation influence patient outcome (20). The frequency of co-existing CLT in patients with PTC has been variously reported to range from 0.5%-38% (3-5). This variability results from differences in patient selection (gender, age and history of autoimmune thyroid disorder) or indication for thyroidectomy, differences of the histopathologic definition for CLT, environmental factors (history of radiation exposure), genetic background and geographic factors (e.g., iodine intake) (3-5). Presently, CLT was defined as the presence of lymphoid follicles with germinal centers, atrophic changes in the area of normal thyroid parenchyma and excluded only lymphocytic infiltration within or surrounding a tumor focus. Using this definition, 26.5% of the PTC patients had CLT in our study. This frequency of CLT with PTC is consistent with recent reports in patients undergoing thyroidectomy (3, 4, 9, 21).
The autoimmune response to thyroid-specific antigens in patients with CLT may be involved in the destruction of cancer cells expressing thyroid-specific antigen in PTC, thus preventing recurrences and improving survival. However, it remains unclear whether or not the presence of CLT affects the biologic behavior of PTC, although the association between CLT and PTC has been reported in many studies (2-6, 8, 9, 11).
Bagnasco et al. (22) reported a higher proportion of cytotoxic T cells with natural killer (NK)-like or lymphokine-activated killer activity in PTC infiltrating T cells compared to those occurring in autoimmune thyroid disorders (Hashimoto's thyroiditis and Graves' disease). In addition to the primarily cell-mediated inflammatory reaction observed in PTC. Lucas et al. (23) demonstrated that more humoral-mediated immune reactions occur with PTC (80% of PTC cases) than with other thyroid neoplasms or autoimmune thyroid disorders. This study suggests that a humoral-specific tumor immune response consisting of an immunoglobulin/complement-mediated reaction may also occur with PTC. Therefore, both humoral and cytotoxic T cell-mediated destruction involved in autoimmune thyroid disorders may have a direct or indirect effect in patients with PTC associated with CLT (24). The Fas-mediated apoptotic pathway activated by Fas and Fas ligand is expressed in follicular cells in patients with CLT, and might be involved in the destruction of tumor cells in patients with Hashimoto's thyroiditis, which is similar to CLT histopathologically (25). Kimura et al. (26) reported that interleukin-1 secreted by infiltrating lymphocytes inhibits human thyroid carcinoma cell growth. Therefore, destruction of tumor cells via humoral and cytotoxic T cell-mediated immune mechanisms might be related to the favorable effect of CLT on PTC. In a large retrospective study conducted by Kim et al. (3), the presence of CLT in patients with PTC was associated with a smaller tumor size, younger age, female predominant and a reduced risk of recurrence; these findings echo those of Kebebew et al. (3, 4).
Based on univariate analysis in our study, PTC in patients with CLT was significantly associated with younger age, female gender, smaller tumor size, a lower incidence of extrathyroidal extension and a lower incidence of LN metastasis ratio compared to patients without CLT. If our hypothesis that coexistent CLT might contribute to a better prognosis in patients with PTC is correct, patients with more severe CLT would have better prognostic factors of PTC. However, there were no significant differences in the clinicopathologic parameters evaluating the correlation between the pathologic and laboratory findings among patients with pathologically confirmed CLT.
Emerging literature suggests a protective effect of CLT in patients with PTC. In a large retrospective study, Kashima et al. (9) reported a 0.7% cancer specific mortality and a 95% relapse-free 10-yr survival rate in patients with CLT, compared to a 5% mortality and 85% relapse-free 10-yr survival rate without CLT. These findings were similar to another study (6). Singh et al. (8) identified a positive correlation between CLT in patients with PTC and DFS and overall survival, and concluded that patients with PTC in the presence of CLT had a more favorable clinical outcome in terms of recurrence and mortality. Also, in our study, 98.46% relapse-free 5-yr survival rate in patients with CLT was evident, compared to a 95.02% relapse-free 5-yr survival rate in patients without CLT.
In our study, coexisting CLT was assumed to be associated with better prognostic factors, such as younger age, smaller tumor size, female and lower extrathyroidal extension at the time of initial surgery than in patients with PTC alone. However, the statistical significance was not verified by multivariate analysis (Table 4). Furthermore, we analyzed the outcomes separately for the lower-risk group and high-risk group by AMES stage and MACIS scoring system. Although, there were significant differences in lower-risk patients with CLT compared with those without CLT by AMES stage and MACIS scoring system, there were no significant difference in high-risk patients with CLT compared with those without CLT by AMES stage and MACIS scoring system. So, CLT was not an independent negative predictive factor. This result was most likely because most of the patients with CLT had other good prognostic factors, such younger age and female gender. The results echo those of Kebebew et al. (4).
This study has some potential limitations. The study was based on patients who had suspected malignant nodules and underwent thyroid surgery. This would introduce a selection bias into the study population. Moreover, since many patients with CLT are not treated surgically, we were unable to account for the true incidence of CLT. A prospective cohort study of the general population should be performed to overcome these limitations.
In conclusion, we found a relatively common occurrence of CLT in patients with PTC. Compared to patients with PTC without CLT, patients with CLT were younger, predominantly female, had a small tumor size and a lower extrathyroidal extension rate at the time of surgery, which are the most important and well-known prognostic variables for thyroid cancer mortality. Although coexistent CLT in PTC patients reduced the risk of recurrence, especially in patients with LN metastasis at the time of surgery, CLT was not an independent predictive factor for recurrence.
Figures and Tables
Fig. 1
Disease free survival rate in patients who underwent total thyroidectomy with central compartment node dissection.

Table 1
Initial clinical manifestation of total patients who underwent thyroid surgery for PTC at the time of surgery

Table 2
Clinicopathologic characteristics of patients who underwent total thyroidectomy with CCND for PTC and follow up for 5 yr
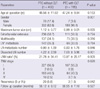
Table 3
Evaluation of the expectant prognostic outcome using the AMES clinical staging system and the MACIS scoring system

Table 4
Univariate and multivariate analysis for recurrence with the statistically significant variables

References
1. Hodgson NC, Button J, Solorzano CC. Thyroid cancer: is the incidence still increasing? Ann Surg Oncol. 2004. 11:1093–1097.
2. Dailey ME, Lindsay S, Skahen R. Relation of thyroid neoplasms to Hashimoto disease of the thyroid gland. AMA Arch Surg. 1955. 70:291–297.
3. Kim EY, Kim WG, Kim WB, Kim TY, Kim JM, Ryu JS, Hong SJ, Gong G, Shong YK. Coexistence of chronic lymphocytic thyroiditis is associated with lower recurrence rates in patients with papillary thyroid carcinoma. Clin Endocrinol (Oxf). 2009. 71:581–586.
4. Kebebew E, Treseler PA, Ituarte PH, Clark OH. Coexisting chronic lymphocytic thyroiditis and papillary thyroid cancer revisited. World J Surg. 2001. 25:632–637.
5. Okayasu I, Fujiwara M, Hara Y, Tanaka Y, Rose NR. Association of chronic lymphocytic thyroiditis and thyroid papillary carcinoma. A study of surgical cases among Japanese, and white and African Americans. Cancer. 1995. 76:2312–2318.
6. Loh KC, Greenspan FS, Dong F, Miller TR, Yeo PP. Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab. 1999. 84:458–463.
7. Holm LE, Blomgren H, Lowhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 1985. 312:601–604.
8. Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999. 126:1070–1076.
9. Kashima K, Yokoyama S, Noguchi S, Murakami N, Yamashita H, Watanabe S, Uchino S, Toda M, Sasaki A, Daa T, et al. Chronic thyroiditis as a favorable prognostic factor in papillary thyroid carcinoma. Thyroid. 1998. 8:197–202.
10. Lee MJ, Lee BK, Youn HJ, Jung SH. Is Hashimoto's thyroiditis associated with the prognostic factor of papillary thyroid carcinoma. Korean J Endocr Surg. 2010. 10:29–33.
11. Del Rio P, Cataldo S, Sommaruga L, Concione L, Arcuri MF, Sianesi M. The association between papillary carcinoma and chronic lymphocytic thyroiditis: does it modify the prognosis of cancer? Minerva Endocrinol. 2008. 33:1–5.
12. Koo BS, Yoon YH, Kim JM, Choi EC, Lim YC. Predictive factors of level IIb lymph node metastasis in patients with papillary thyroid carcinoma. Ann Surg Oncol. 2009. 16:1344–1347.
13. Mercante G, Frasoldati A, Pedroni C, Formisano D, Renna L, Piana S, Gardini G, Valcavi R, Barbieri V. Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid. 2009. 19:707–716.
14. Sciuto R, Romano L, Rea S, Marandino F, Sperduti I, Maini CL. Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1503 patients treated at a single institution. Ann Oncol. 2009. 20:1728–1735.
15. Sanders LE, Cady B. Differentiated thyroid cancer: reexamination of risk groups and outcome of treatment. Arch Surg. 1998. 133:419–425.
16. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993. 114:1050–1057.
17. Hunt JL, Baloch ZW, Barnes L, Swalsky PA, Trusky CL, Sesatomi E, Finkelstein S, LiVolsi VA. Loss of heterozygosity mutations of tumor suppressor genes in cytologically atypical areas in chronic lymphocytic thyroiditis. Endocr Pathol. 2002. 13:321–330.
18. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.
19. Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985-1995. Cancer. 1998. 83:2638–2648.
20. Treseler PA, Clark OH. Prognostic factors in thyroid carcinoma. Surg Oncol Clin N Am. 1997. 6:555–598.
21. DeGroot LJ, Kaplan EL, McCormick M, Straus FH. Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab. 1990. 71:414–424.
22. Bagnasco M, Venuti D, Paolieri F, Torre G, Ferrini S, Canonica GW. Phenotypic and functional analysis at the clonal level of infiltrating T lymphocytes in papillary carcinoma of the thyroid: prevalence of cytolytic T cells with natural killer-like or lymphokine-activated killer activity. J Clin Endocrinol Metab. 1989. 69:832–836.
23. Lucas SD, Karlsson-Parra A, Nilsson B, Grimelius L, Akerstrom G, Rastad J, Juhlin C. Tumor-specific deposition of immunoglobulin G and complement in papillary thyroid carcinoma. Hum Pathol. 1996. 27:1329–1335.
24. Cunha LL, Ferreira RC, Marcello MA, Vassallo J, Ward LS. Clinical and pathological implications of concurrent autoimmune thyroid disorders and papillary thyroid cancer. J Thyroid Res. 2011. 2011:387062.
25. Giordano C, Stassi G, De Maria R, Todaro M, Richiusa P, Papoff G, Ruberti G, Bagnasco M, Testi R, Galluzzo A. Potential involvement of Fas and its ligand in the pathogenesis of Hashimoto's thyroiditis. Science. 1997. 275:960–963.
26. Kimura H, Yamashita S, Namba H, Tominaga T, Tsuruta M, Yokoyama N, Izumi M, Nagataki S. Interleukin-1 inhibits human thyroid carcinoma cell growth. J Clin Endocrinol Metab. 1992. 75:596–602.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download