Abstract
We analyzed the direct medical costs for Korean patients with type 2 diabetes according to the type of complications and the number of microvascular complications. We analyzed costs for type 2 diabetes and associated complications in 3,125 patients. These data were obtained from the Korean National Diabetes Program (KNDP), a large, ongoing, prospective cohort study that began in 2005. The cost data were prospectively collected, using an electronic database, for the KNDP cohort at six hospitals. The costs were analyzed according to complications for 1 yr from enrollment in the study. Among 3,125 patients, 918 patients had no vascular complications; 1,883 had microvascular complications only; 51 had macrovascular complications only; and 273 had both complications. The annual direct medical costs for a patient with only macrovascular, only microvascular, or both macrovascular and microvascular complications were 2.7, 1.5, and 2.0 times higher than the medical costs of patients without complications. Annual direct medical costs per patient increased with the number of microvascular complications in patients without macrovascular complications. The economic costs for type 2 diabetes are attributable largely to the management of microvascular and macrovascular complications. Proper management of diabetes and prevention of related complications are important for reducing medical costs.
Diabetes is a major health problem worldwide, and the incidence, prevalence, and mortality associated with diabetes have increased consistently (1). According to the World Health Organization and International Diabetes Federation, the number of patients with diabetes will increase from 135 million in 1995 to 300 million in 2025 (2, 3), an increase of more than twofold over the course of 30 yr.
Type 2 diabetes is a chronic disease that is always associated with long-term and life-threatening complications. These complications can be divided into two categories: macrovascular and microvascular complications. Macrovascular complications include cardiovascular, cerebrovascular, and peripheral artery obstructive disease. Microvascular complications include retinopathy, nephropathy, and neuropathy. Most patients with diabetes ultimately suffer from these complications.
With the increasing incidence of diabetes, the economic burden of diabetes, given its chronic nature, severe complications, and need for long-term care, has become an important public health issue (4). In particular, the management of microvascular and macrovascular complications accounts for a large portion of costs during diabetic care (5-7). The economic costs of diabetes have been well researched and recognized in the USA (8) and many developed countries of western Europe (9). However, few studies have been performed in developing Asian countries, including Korea.
The prevalence of type 2 diabetes is rapidly increasing in Asian countries, especially in Korea (10). The prevalence of type 2 diabetes is reported to be increasing at a rate of 7.9% among Koreans 20 to 79 yr of age (11). The economic burden of type 2 diabetes is also increasing in Korea. According to the Korea National Health and Nutrition Examination Survey, the aggregate annual direct costs of diabetes were 260 million dollars in 2009 (12).
The Korean National Diabetes Program (KNDP), a large, ongoing, prospective cohort study that begin in 2005, is aimed at investigating the pathophysiology of type 2 diabetes in Korean patients (13). This 9-yr study will provide clinical evidence on the pathophysiology of Korean patients with type 2 diabetes and patients with a high risk for type 2 diabetes. The goal of the KNDP is to develop accurate guidelines for the prevention and treatment of diabetes that will ultimately lead to increased quality of life and decreased mortality.
In this study, we used the KNDP data to analyze and compare the annual medical costs for type 2 diabetic patients with no complications and type 2 diabetic patients with microvascular complications, macrovascular complications, or both.
Type 2 diabetic patients who were participants in the KNDP at six hospitals in Korea were enrolled. Inclusion criteria for the type 2 diabetic patients included: older than 20 yr of age, newly diagnosed with type 2 diabetes according to American Diabetes Association (ADA) criteria (in 2004) (14); and treatment with oral hyperglycemic agents, insulin, or lifestyle modification. Age, gender, duration of diabetes, height, weight, abdominal circumference, and blood pressure were recorded. Blood was drawn for a fasting blood glucose test, HbA1c assay, lipid profile determination, and other biochemical tests. Information on concurrent diseases such as hypertension and dyslipidemia, and a medical history, including macrovascular and microvascular complications, were collected for each patient through questionnaires, medical records, and examinations. Among the KNDP cohort, we analyzed 3,125 patients at six hospitals.
Macrovascular complications consisted of myocardial infarction, angina, other cardiovascular complications with congestive heart failure, cerebral infarction, peripheral arterial obstructive disease (PAOD), and amputation of extremities. PAOD was determined only after diagnosis by angiography. Microvascular complications consisted of diabetic retinopathy, neuropathy, and nephropathy, including dialysis and renal transplantation. Diabetic retinopathy was defined with a past medical history and abnormal results of fundus photography. Diabetic neuropathy was defined with a past medical history and any abnormal results of autonomic neuropathy tests, vibration perception, or current perception thresholds. To define diabetic nephropathy, the albumin/creatinine ratio or estimated glomerular filtration rate (GFR) of random urine sampling was used. Diabetic nephropathy was diagnosed based on microalbuminuria or a GFR below 60 mL/min/1.73 m2, where GFR was calculated as:
Estimated GFR (mL/min/1.73 m2) = 186.3 × (serum creatinine)-1.154 × (age)-0.203.
This value was multiplied by 0.742 to calculate the GFR in females.
The cost data were prospectively collected using electronic databases from six of the KNDP hospitals and comprised medical costs covered by insurance and those not covered. We calculated direct medical costs and did not included non-direct nonmedical costs (e.g., costs associated with transportation and care of dependents). Direct medical costs included outpatient and hospitalization costs. Outpatient costs consisted of costs associated with physician services, medications, examinations, and other (medical supplies). Hospitalization costs were identified from aggregate departmental expenditures.
To compare the costs of patients with and without complications, we classified patients into four disease groups: diabetes without complications, diabetes with microvascular complications, diabetes with macrovascular complications, and diabetes with both complications. We analyzed the costs of type 2 diabetes according to complications for 1 yr after registration in the KNDP cohort.
Statistical analyses were performed using PASW version 18.0 software (PASW Inc., Chicago, IL, USA). Differences in the baseline characteristics between the groups were compared using the chi-square test for dichotomous variables and one-way analysis of variance (ANOVA) for continuous variables. ANOVA was performed to assess annual costs. For significant ANOVA results, a Tukey post hoc multiple comparison was used to establish differences between the groups. Values of P < 0.05 were considered to indicate statistical significance.
The institutional medical ethics committee at each hospital approved the methods involved in the present study (Ajou University Hospital: AJIRB-CRO-05-093; Kyung Hee University Hospital: KMC05-26-04; Inha University Hospital: 2006-67; Hanyang University Hospital: 2005-250; Korea University Guro Hospital: GR0542-001; Kyung Hee University Kangdong Hospital: KHNMC IRB 2006-017). Informed consent was provided by all of the patients following a sufficient explanation of the study.
The baseline characteristics of the patients are shown in Table 1. Of the 3,125 patients, 1,768 (56.6%) patients were female. The mean patient age was 54.7 yr (range, 20-86 yr). The average duration of diabetes was 5.7 yr; the average HbA1c level was 7.7%. About half of all patients (46.2%) were treated with oral hypoglycemic agents only, 5.0% of patients were treated with insulin only, and 29.5% were taking drugs for hypertension. About 49% of the patients had a history of smoking.
Table 2 shows comparisons of patient baseline characteristics by complication type. Of the 3,125 patients, 918 (29.4%) did not exhibit vascular complications; 1,883 (60.3%) had microvascular complications without macrovascular complications; 273 (8.7%) had macrovascular and microvascular complications; and 51 (1.6%) had macrovascular complications without microvascular complications. Patients with both complications were significantly older and had a longer duration of illness. Diet and exercise accounted for treatment in half of the patients without complications. The proportion of patients using insulin was increased in patients with both complications. The percentage of patients treated with antihypertensive medication was higher in patients with complications.
Among those with microvascular complications, 470 patients had retinopathy, 804 patients had nephropathy, and 1,715 patients had neuropathy. There were no patients on dialysis or with a history of kidney transplantation. Among the patients with macrovascular complications, 58 had a history of myocardial infarction, 88 had a history of angina pectoris, and 162 had a history of cerebrovascular events. During the follow-up period, macrovascular complications occurred in 18 patients, and five patients died.
The annual mean cost per capita for type 2 diabetic patients is shown in Table 3 according to complications. The annual direct medical cost per patient was U$1,939 equivalent, of which outpatient costs were 74.9% (U$1,453 equivalent) and hospitalization costs were 25.1% (U$486 equivalent). Medications accounted for the largest portion (66.6%) of outpatient costs, followed by examinations (22.7%), physician services (8.5%), and other costs (2.3%). Comparing according to complications, the annual direct medical cost per capita was highest in patients with macrovascular complications compared with other patients (Fig. 1).
The annual direct medical costs for a patient with only macrovascular, only microvascular, or both macrovascular and microvascular complications were 2.7, 1.5, and 2.0 times higher than the costs for patients without complications. Costs for hospitalization were higher than costs for outpatient services in the group with only macrovascular complications; however, outpatient costs were highest in the group with both microvascular and macrovascular complications. Medication costs accounted for 64.5%, 67%, 68.5%, and 67.6% of outpatient costs for patients with no complications, microvascular complications only, macrovascular complications only, and both complications, respectively.
There were significant differences in the annual direct medical costs between patients with and without macrovascular complications. Among patients without macrovascular complications, the annual direct medical cost per patient increased with an increase in the number of microvascular complications. Specifically, costs for physician services, medications, and hospitalization were significantly higher in patients with more microvascular complications. However, there were no significant differences in costs among patients with macrovascular complications (Table 4). Comparisons between patients with one or more complications and those without complications are presented in Fig. 2.
In this study, we analyzed the direct medical costs for type 2 diabetic Korean patients according to the type and number of complications. Annual direct medical costs were higher for type 2 diabetic patients with macrovascular or both microvascular and macrovascular complications, and annual direct medical costs increased with an increased number of combined microvascular complications in patients without macrovascular complications.
Many retrospective studies have demonstrated that the presence, type, and number of diabetic complications have an impact on the cost of diabetic care. This prospective study showed similar results. Costs were higher for diabetic patients with complications than for those without complications, and macrovascular complications had a greater impact than microvascular complications. Other studies (e.g., the CODE-2 study) have reported that costs for patients with both complications were highest, followed by macrovascular only and then microvascular only complications. In contrast, our study found that the costs for patients with both complications were lower than the costs for patients with macrovascular complications only (9, 15). This difference may be due to a shorter duration of illness (4.5 yr vs 8.4 yr) or higher hospitalization costs for patients with only macrovascular complications compared to patients with both complications. Higher hospitalization costs for patients with a shorter duration of diabetes were associated with recent macrovascular complications. Brandle and colleagues reported high direct medical costs during the first year following the onset of macrovascular complications (16). A longer duration of diabetes in patients with both complications also suggested that operations or procedures which occupied a large portion of the costs of hospitalization had already been done. Thus the cost for patients with both complications was lower than that for patients with macrovascular complications only in our study.
Except in the macrovascular complications only group, medication costs accounted for the largest portion of total costs, and the percentage was highest in the microvascular and macrovascular complications group, followed by the microvascular complications only group, and the no complications group. With respect to the distribution of total costs, medications and hospitalization were the largest categories. These results are consistent with those of previous studies (8, 9, 15-17).
In patients without macrovascular complications, the total costs increased with an increased number of microvascular complications. However, in patients with macrovascular complications, additional microvascular complications did not contribute significantly to the direct medical costs. This indicates that macrovascular complications are a major source of costs for diabetic patients and suggests that prevention and proper management of macrovascular complications may be effective interventions for reducing the long-term economic burden of diabetic therapy.
Early diagnosis, optimal management of blood glucose levels, blood pressure, and lipid concentrations; together with early detection and management of complications are important aspects of minimizing the occurrence of type 2 diabetes and its related complications (18). In general, the level of management for diabetics differs significantly between developing and developed countries (19). Unlike in acute care, prevention, early detection, and proper treatment of diabetes have not received adequate attention in developing countries (20). Thus, the prevalence of diabetes is increasing rapidly in developing countries. In Korea, the prevalence of diabetes increased rapidly until the late 1990s (21-23). In other developing Asian countries such as China and India, increased prevalence of diabetes has accompanied fast economic growth (24, 25). Recent reports indicate that the prevalence of diabetes in Korea did not change significantly for 7 yr after 1998, suggesting that the prevalence of diabetes in Korea is currently increasing at a rate intermediate between the rates in developing and developed countries. Although the prevalence of diagnosed diabetes in Korea was 68% in 2005 and has increased to a percentage matching that in developed countries, the control of diabetes has not yet achieved the level of control in developed countries (26). Based on these results, proper management of diabetes and prevention of its related complications may be better approaches than early detection for reducing the cost of diabetes treatment in Korea.
The cost of diabetes care tends to increase in relation to a country's degree of economic development, although it is difficult to compare costs between different countries because of social and economic differences and differences in the methods used. Nevertheless, it can be useful to assess the magnitude of the economic burden of diabetes in Korea. Annual direct medical costs per patient in this study (U$1,939 equivalent) were far less than the costs in developed countries such as the USA (direct medical costs, U$11,744) (8) and Germany (direct total cost, U$4,713) (27), but were more than those in developing countries such as Iran (direct total cost, U$152) (28), India (direct total cost, U$525.5) (29), and China (direct medical cost, U$1,321) (30). We suggest that the costs for diabetes treatment in Korea, similar to the prevalence of diabetes, are intermediate between those of developing and developed countries.
This study had some limitations. First, because the enrolled patients were from only six general hospitals, this study did not represent the general type 2 diabetic population in Korea. Furthermore, general hospital charges are more expensive than those of non-general hospitals in Korea. Second, the costs in this study reflected only direct medical costs and did not include direct nonmedical costs or indirect costs, making cost comparisons with other countries difficult. Third, although the present study was a prospective cohort study, the costs of medical services provided by other hospitals to the patients enrolled in the current study were not included. Fourth, because the presence of diabetic complications was identified by questionnaires and examinations, reporting bias might have affected the classification of complications and costs. Finally, we did not distinguish the stage of each diabetic complication, which might have affected the cost differences. Future studies are necessary to evaluate the most effective treatment regimens for the prevention of diabetic complications. The strength of our study is its prospective cohort study design. We collected total cost data of enrolled patients in the same hospital for 1 yr. In Korea, most patients who use a general hospital tend to always use the same hospital. Thus, we believe that the costs estimated using these data were reliable.
In conclusion, the economic cost for type 2 diabetes is highly associated with the management of macrovascular complications, rather than microvascular complications. Moreover, the cost increases as the number of combined microvascular complications increases in patients without macrovascular complications. The present study indicates that proper management of diabetes and prevention of related complications are important to reduce the economic burden associated with diabetes.
Figures and Tables
Fig. 1
Annual direct medical costs per patient according to microvascular and macrovascular complications. (A) Annual direct medical cost breakdown by type of complication. (B) Cost categories contributing to annual direct medical costs per patient. (C) Cost categories contributing to outpatient costs per patient.

Fig. 2
Annual direct medical costs per patients by number of microvascular complications. (A) In patients without macrovascular complications. (B) In those with macrovascular complications. *P < 0.001 by ANOVA.

Table 2
Comparison of study population characteristics according to complications
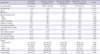
Data are expressed as the number of patients (%), range, or mean ± SD. Differences between groups were compared using a chi-square test for dichotomous variables and one-way analysis of variance for continuous variables. BMI, Body mass index; BP, Blood pressure; HDL, High density lipoprotein; LDL, Low density lipoprotein; OHA, Oral hyperglycemic agent.
References
1. Bjork S. The cost of diabetes and diabetes care. Diabetes Res Clin Pract. 2001. 54:S13–S18.
2. Rekkedal G. WHO world health report 1997. Tidsskr Sykepl. 1997. 85:37–39.
3. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998. 21:1414–1431.
4. Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007. 370:1929–1938.
5. Huse DM, Oster G, Killen AR, Lacey MJ, Colditz GA. The economic costs of non-insulin-dependent diabetes mellitus. JAMA. 1989. 262:2708–2713.
6. Brown JB, Pedula KL, Bakst AW. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med. 1999. 159:1873–1880.
7. Williams R, Van Gaal L, Lucioni C. Assessing the impact of complications on the costs of Type II diabetes. Diabetologia. 2002. 45:S13–S17.
8. American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008. 31:596–615.
9. Massi-Benedetti M. The cost of diabetes Type II in Europe: the CODE-2 Study. Diabetologia. 2002. 45:S1–S4.
10. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006. 368:1681–1688.
11. Unwin N, Mbanya JC, Ramachandran A, Roglic G, Shaw J, Soltèsz G, Whiting D, Zgibor J, Zhang P, Zimmet P. Diabetes Atlas fourth edition committee. The IDF Diabetes Atlas 2010. accessed on 23 December 2010. Available from http://www.diabetesatlas.org/content/wp-data.
12. Korea Centers for Disease Control and Prevention(KCDC). The Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV-3),2009. 2010. Seoul: KCDC.
13. Rhee SY, Chon S, Kwon MK, Park IB, Ahn KJ, Kim IJ, Kim SH, Lee HW, Koh KS, Kim DM, et al. Prevalence of chronic complications in Korean patients with type 2 diabetes mellitus based on the Korean national diabetes program. Diabetes Metab J. 2011. 35:504–512.
14. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2004. 27:S15–S35.
15. Morsanutto A, Berto P, Lopatriello S, Gelisio R, Voinovich D, Cippo PP, Mantovani LG. Major complications have an impact on total annual medical cost of diabetes: results of a database analysis. J Diabetes Complications. 2006. 20:163–169.
16. Brandle M, Zhou H, Smith BR, Marriott D, Burke R, Tabaei BP, Brown MB, Herman WH. The direct medical cost of type 2 diabetes. Diabetes Care. 2003. 26:2300–2304.
17. Oliva J, Lobo F, Molina B, Monereo S. Direct health care costs of diabetic patients in Spain. Diabetes Care. 2004. 27:2616–2621.
18. European Diabetes Policy Group 1999. A desktop guide to type 2 diabetes mellitus. Diabet Med. 1999. 16:716–730.
19. Kapur A. Economic analysis of diabetes care. Indian J Med Res. 2007. 125:473–482.
20. Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, Haines A. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008. 372:940–949.
21. Kim KS, Choi CH, Lee DY, Kim EJ. Epidemiological study on diabetes mellitus among rural Koreans. Korean Diabetes J. 1972. 1:17–24.
22. Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in Yonchon County, South Korea. Diabetes Care. 1995. 18:545–548.
23. Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK, Baik SH, Choi DS, Choi KM. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care. 2006. 29:226–231.
24. Hu D, Fu P, Xie J, Chen CS, Yu D, Whelton PK, He J, Gu D. Increasing prevalence and low awareness, treatment and control of diabetes mellitus among Chinese adults: the InterASIA study. Diabetes Res Clin Pract. 2008. 81:250–257.
25. Ramachandran A, Mary S, Yamuna A, Murugesan N, Snehalatha C. High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India. Diabetes Care. 2008. 31:893–898.
26. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009. 32:2016–2020.
27. Koster I, von Ferber L, Ihle P, Schubert I, Hauner H. The cost burden of diabetes mellitus: the evidence from Germany--the CoDiM study. Diabetologia. 2006. 49:1498–1504.
28. Esteghamati A, Khalilzadeh O, Anvari M, Meysamie A, Abbasi M, Forouzanfar M, Alaeddini F. The economic costs of diabetes: a populationbased study in Tehran, Iran. Diabetologia. 2009. 52:1520–1527.
29. Tharkar S, Devarajan A, Kumpatla S, Viswanathan V. The socioeconomics of diabetes from a developing country: a population based cost of illness study. Diabetes Res Clin Pract. 2010. 89:334–340.
30. Wang W, McGreevey WP, Fu C, Zhan S, Luan R, Chen W, Xu B. Type 2 diabetes mellitus in China: a preventable economic burden. Am J Manag Care. 2009. 15:593–601.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download