Abstract
Alopecia totalis (AT) and alopecia universalis (AU), severe forms of alopecia areata (AA), show distinguishable clinical characteristics from those of patch AA. In this study, we investigated the clinical characteristics of AT/AU according to the onset age. Based on the onset age around adolescence (< or ≥ 13 yr), 108 patients were classified in an early-onset group and the other 179 patients in a late-onset group. We found that more patients in the early-onset group had a family history of AA, nail dystrophy, and history of atopic dermatitis than those in the late-onset group. These clinical differences were more prominent in patients with AU than in those with AT. In addition, significantly more patients with concomitant medical disorders, especially allergic diseases were found in the early-onset group (45.8%) than in the late-onset group (31.2%). All treatment modalities failed to show any association with the present hair condition of patients. In the early-onset group, patients with AU or a family history of AA showed worse prognosis, whereas this trend was not observed in the late-onset group. Systemic evaluations might be needed in early-onset patients due to the higher incidence of comorbid diseases. It is suggested that patients with AU or family history of AA make worse progress in the early-onset group than in the late-onset group.
Alopecia areata (AA) is a common disorder that accounts for 1%-3% of patients visiting dermatology clinics (1). Although it usually presents as asymptomatic localized hair loss (patch AA), it is a disease of very broad spectrum. The hair of the entire scalp and the whole body can be affected, which are called alopecia totalis (AT) and alopecia universalis (AU), respectively. AT and AU are severe forms of AA and only 10% of patients with AT/AU experience full recovery (2, 3).
AA is characterized by a variety of clinical courses, and it is not easy for clinicians to predict prognosis and clinical outcome of each patient. However, several epidemiologic studies on clinical presentation of AA have reported that onset before adolescence is one of the important prognostic factors (4). The extent of involvement, ophiasis pattern of hair loss, long duration of hair loss, a positive family history, nail involvement, atopic diseases and other autoimmune diseases are also known as predictors of poor prognosis in patients with AA (1, 2, 5-8). However, their correlations were identified mainly based on patients with patch AA, and AT/AU has rarely been studied separately although these severe forms of AA show different characteristics and clinical features from patch AA.
In this study, we investigated the clinical characteristics of AT/AU retrospectively by review of medical records and telephone-interview. Patients with AT/AU were classified into the early- or late-onset group by the onset-age (< or ≥ 13 yr), and demographic data, type of AA, family history of AA, comorbid disorders, treatment modalities and the present state of hair loss were assessed and compared in these groups.
A total of 287 patients diagnosed as AT or AU in Seoul National University Hospital (SNUH) from 1999 to 2010 were enrolled in this study. The medical records were reviewed retrospectively and the patients were interviewed by telephone. All subjects were classified into the early-onset or late-onset group based on the age at onset of < or ≥ 13 yr, respectively, and the clinical profiles of these two groups regarding alopecia and associated conditions were then compared.
Clinical details including type of alopecia, age at onset, family history of AA, concomitant disorders, and treatment history were obtained from the review of medical records. Treatment modalities were classified as follows: application of topical steroids, intralesional injection of triamcinolone, immunotherapy with diphencyprone or squaric acid dibutyl ester, and oral administration of corticosteroids or systemic immunosuppressant like cyclosporine. Information on the present state of AT/AU was obtained from medical records for a total of 161 patients; 83 patients who recently visited our clinic and from telephone interviews for the other 78 patients; we could not follow-up the other 126 patients. We compared the present state with the state at the first visit and graded the disease state as described above: aggravation or no improvement (< 25%), partial improvement (25%-75%) and much improvement (> 75%). In case of telephone interview, we checked the compartment of hair re-growth (frontal, parietal, occipital, temporal, vertex) and percentage of that compartment (7). If the patient could not answer as percentage, we asked about the subjective assessment of their current scalp status.
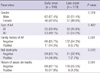
Clinical profiles of 287 patients (154 males, 133 females) with AT/AU were assessed. Among them, 137 patients had AT and the other 150 patients had AU. Their age of onset ranged from 1 yr to 61 yr (mean 19.7 ± 14.1 yr). Based on the age at onset of < or ≥ 13 yr, 108 patients were classified to the early-onset group and the other 179 patients to the late-onset group, respectively. Regarding gender and type of AA, no significant difference was found between the early- and late-onset groups. However, significantly more patients in the early-onset group had family history of AA, concomitant nail dystrophy, and history of atopic dermatitis than in the late-onset group (Table 1). These clinical differences were more prominent in patients with AU than in those with AT. Analysis of patients with AU showed that family history of AA (P = 0.007), nail dystrophy (P = 0.058), and history of atopic dermatitis (P < 0.001) were more frequently seen in the early-onset group than in the late-onset group. These tendencies were similarly observed in patients with AT but were not statistically significant (Fig. 1).
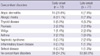
Fifty-seven patients (38.4%) in the study population had a medical history of concomitant disorders, most of which were previously reported with AA. Significantly more patients with a concomitant medical disorder were found in the early-onset group (n = 33, 45.8%) than in the late-onset group (n = 24, 31.2%). Allergic diseases such as atopic dermatitis, allergic rhinitis, and asthma were more common in the early-onset group (34.7%) than in the late-onset group (15.6%). After allergic diseases, thyroid disease was the most common comorbid disorder in both groups (Table 2).
Topical application (n = 217, 75.6%) and oral administration (n = 218, 76.0%) of steroids were most frequent treatment modalities for AT/AU, followed by immunotherapy (n = 161, 56.1%), triamcinolone intralesional injection (n = 116, 40.4%), and cyclosporine A (n = 110, 38.3%) regardless of onset-age and type of AA.
Progress of alopecia was assessed in 161 patients (71 with AT, 90 with AU) by comparing the present hair state with the state at the first visit. In the AT group, 33 patients (46.5%) experienced partial improvement and 12 patients (16.9%) experienced much improvement. Among the other 26 patients, 12 cases (16.9%) experienced disease progress to AU. However, only 5 patients (5.6%) in the AU group experienced much improvement and the difference was statistically significant (P = 0.011). In the early-onset group, AU made worse progress than AT and patients with family history of AA were significantly unimproved compared with those without family history of AA (P = 0.041), whereas there was no association with gender, atopic dermatitis and nail dystrophy. In contrast, even a family history of AA was not associated with disease progress in the late-onset group. Concerning the history of treatment modalities, we did not find any significant association between the present state of hair loss and the history of treatment modalities in either the early- or late-onset group.
AA is a disease of broad spectrum ranging from localized patch hair loss to hair loss over the whole body, and the clinical features are very different according to the severity of the disease. For example, AT/AU patients were younger at the age of onset and more likely to have concomitant disorders than those with patch AA (6). Several studies reported the clinical features and prognosis of AA (6, 9-11), but most subjects in these studies were patients with localized patch AA and the clinical features of AT/AU were therefore rarely assessed, especially by age at onset. The present study was performed on patients with AT/AU excluding patch AA. We classified patients into early- and late-onset groups based on the onset-age of 13 yr because previous epidemiologic studies have generally considered the onset-age of puberty as around 13 yr (12, 13). There was no significant difference in gender and ratio of AT and AU between groups. Interestingly, some clinical features, such as family history, atopic disorders, and nail changes, showed significant differences between early- and late-onset groups only in patients with AU, a more severe type of AA than AT.
As mentioned, several autoimmune diseases and atopic disorders are generally thought to be associated with AA (6, 7, 11). According to Goh et al. (6), 56% of AA patients had comorbidities other than AA and the proportion was higher in AT/AU than in patch AA. However, some studies reported that the incidence of concomitant disorders was not higher either in patients with severe type AA or in patients in whom AA had developed during childhood (7, 14). In our study, 38.4% of AT/AU patients had concomitant disorders and atopic dermatitis was most common, which was more prominent in the early-onset group.
The second most common comorbidity was thyroid disorder in both groups. Thyroid disease, including Grave's disease, Hashimoto's thyroiditis and simple goiter, are reported in 8% to 28% of AA patients (1). In one Korean report, 1.4% of AA individuals had autoimmune thyroid disease (15). Compared with those in a previous report, a relatively high rate (6.0%) of AT/AU individuals had thyroid diseases in this study, but no differences were seen in the two groups. It has been known that AT/AU is less favorable than patch AA and fewer than 10% of AT/AU patients recover spontaneously (16), which was consistent with our result that 16.9% of AT patients and 5.6% of AU patients showed > 75% improvement.
The most common therapy used in AA is intralesional injection of corticosteroids and 64%-97% of AA sites exhibit hair growth (17, 18). In this study, topical application and oral administration of steroid were the most frequently used treatment modalities for AT/AU. However, all treatment modalities including steroid failed to show any association with the present hair condition of patients in this study, which suggested that they cannot alter the long-term clinical course of the disease. In previous studies, several poor prognostic factors were reported, including the extent of hair loss, long duration of hair loss, atopy, a positive family history, the presence of other autoimmune diseases, nail involvement, and young age of onset (1). However, in the cases of AT/AU, the present state of disease was associated with the type of AA and a family history of AA only in the early-onset group, while no associated factors with disease progress were found in the late-onset group. The earlier age of onset and family history suggest a relationship with personal genetic susceptibility as previously reported (19-21).
Our study has certain limitations. First, this study was retrospectively performed and recall bias might be involved because some clinical data were obtained by telephone interview. Secondly, a larger number of subjects would be helpful to statistically confirm the association between age at onset and clinical characteristics of AT/AU. For example, early-onset patients with AT seemed to be more associated with family history of AA, nail dystrophy, and history of atopic dermatitis than late-onset patients with AT, but this finding was not statistically significant. Data from more patients may be useful to demonstrate statistical significance. Thirdly, in the chart review we checked the presence of any comorbid disorders when diagnosed by primary physicians of the patients. Therefore, the some patients would not be included in rhinitis or asthma group even though they developed any suggestive symptom of rhinitis or asthma. Finally, this study was cross-sectional study and reviewed non-standardized treatment method. Therefore, prospective standardized study would be executed to investigate progress of the disease or treatment efficacy.
In summary, early-onset of AU was associated with family history of AA, atopic disorders, and nail changes. Comorbid disorders, especially allergic disorders, were also more common with early-onset AT/AU than with late-onset disease. Assessment of the present hair state suggests that patients with AU or family history of AA make worse progress in the early-onset group than in the late-onset group.
Figures and Tables
References
1. Chua-Ty G, Goh CL, Koh SL. Pattern of skin diseases at the National Skin Centre (Singapore) from 1989-1990. Int J Dermatol. 1992. 31:555–559.
2. Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part I. Clinical picture, histopathology, and pathogenesis. J Am Acad Dermatol. 2010. 62:177–188.
3. MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Brithsh Association of Dermatologists. Guidelines for the management of alopecia areata. Br J Dermatol. 2003. 149:692–699.
4. Walker SA, Rothman S. A statistical study and consideration of endocrine influences. J Invest Dermatol. 1950. 14:403–413.
5. De Waard-van der Spek FB, Oranje AP, De Raeymaecker DM, Peereboom-Wynia JD. Juvenile versus maturity-onset alopecia areata: a comparative retrospective clinical study. Clin Exp Dermatol. 1989. 14:429–433.
6. Goh C, Finkel M, Christos PJ, Sinha AA. Profile of 513 patients with alopecia areata: associations of disease subtypes with atopy, autoimmune disease and positive family history. J Eur Acad Dermatol Venereol. 2006. 20:1055–1060.
7. Tosti A, Bellavista S, Iorizzo M. Alopecia areata: a long term follow-up study of 191 patients. J Am Acad Dermatol. 2006. 55:438–441.
8. Kavak A, Yeşildal N, Parlak AH, Gökdemir G, Aydoğan I, Anul H, Baykal C. Alopecia areata in Turkey: demographic and clinical features. J Eur Acad Dermatol Venereol. 2008. 22:977–981.
9. Green J, Sinclair RD. Genetics of alopecia areata. Australas J Dermatol. 2000. 41:213–218.
10. McDonagh AJ, Tazi-Ahnini R. Epidemiology and genetics of alopecia areata. Clin Exp Dermatol. 2002. 27:405–409.
11. Shellow WV, Edwards JE, Koo JY. Profile of alopecia areata: a questionnaire analysis of patient and family. Int J Dermatol. 1992. 31:186–189.
12. Shin N, Kim SH, Cho S, Whang KK, Hahm JH. The impact of childhood atopic dermatitis on their families. Korean J Dermatol. 2000. 38:494–499.
13. Kliegman RM. Behrman RE, Kliegman R, Nelson WE, editors. Adolescent development. Nelson textbook of pediatrics. 2011. 19th ed. Philadelphia: W.B. Saunders;1778–1780.
14. Sharma VK, Muralidhar S, Kumar B. Reappraisal of Ikeda's classification of alopecia areata: analysis of 356 cases from Chandigarh, India. J Dermatol. 1998. 25:108–111.
15. Kim YJ, Kim BJ, Ro BI. A clinical and psychological study for alopecia areata in children. Korean J Dermatol. 2003. 41:179–186.
16. Paus R, Olsen EA, Messenger AG. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Hair growth disorder. Fitzpatrick's dermatology In general medicine. 2008. 7th ed. New York: McGrow Hill;753–777.
17. Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010. 62:191–202.
18. Porter D, Burton JL. A comparison of intra-lesional triamcinolone hexacetonide and triamcinolone acetonide in alopecia areata. Br J Dermatol. 1971. 85:272–273.
19. Akar A, Arca E, Erbil H, Akay C, Sayal A, Gür AR. Antioxidant enzymes and lipid peroxidation in the scalp of patients with alopecia areata. J Dermatol Sci. 2002. 29:85–90.
20. Colombe BW, Lou CD, Price VH. The genetic basis of alopecia areata: HLA associations with patchy alopecia areata versus alopecia totalis and alopecia universalis. J Investig Dermatol Symp Proc. 1999. 4:216–219.
21. Lu W, Shapiro J, Yu M, Barekatain A, Lo B, Finner A, McElwee K. Alopecia areata: pathogenesis and potential for therapy. Expert Rev Mol Med. 2006. 8:1–19.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download