Abstract
The aim of this study was to investigate the diphtheria-tetanus-pertussis antibody titers after antineoplastic treatment and to suggest an appropriate vaccination approach for pediatric hemato-oncologic patients. A total of 146 children with either malignancy in remission after cessation of therapy or bone marrow failure were recruited. All children had received routine immunization including diphtheria-tetanus-acellular pertussis vaccination before diagnosis of cancer. The serologic immunity to diphtheria, tetanus and pertussis was classified as: completely protective, partially protective, or non-protective. Non-protective serum antibody titer for diphtheria, tetanus and pertussis was detected in 6.2%, 11.6%, and 62.3% of patients, respectively, and partial protective serum antibody titer for diphtheria, tetanus and pertussis was seen in 37%, 28.1%, and 8.9% of patients. There was no significant correlation between the severity of immune defect and age, gender or underlying disease. Revaccination after antineoplastic therapy showed significantly higher levels of antibody for each vaccine antigen. Our data indicates that a large proportion of children lacked protective serum concentrations of antibodies against diphtheria, tetanus, and pertussis. This suggests that reimmunization of these patients is necessary after completion of antineoplastic treatment. Also, prospective studies should be undertaken with the aim of devising a common strategy of revaccination.
Outcome and long-term survival of pediatric patients with malignancies have improved markedly, enabling children to lead a normal life (1). The threat of infectious diseases, however, remains imminent. This increased risk is due to secondary immunodeficiency caused by malignancy and its treatment, which may include the loss of vaccine-induced antibodies and immunological memory (2-4). The resulting susceptibility to infectious diseases increases morbidity and mortality in pediatric hematology and oncology patients. Unfortunately, it is unclear to date whether and to what extent the host defense against vaccine-preventable disease after the end of treatment is effective, which, in turn, has an important impact on preventive strategies. Nevertheless, these studies in patients with malignancies have not been conducted in Korea before.
With awareness of the emerging presence of vaccine-preventable diseases in the general population in recent years, we believed it was necessary to ascertain the level of protection against these diseases in our patients. We focused on the assessment of serologic immunity against diphtheria, tetanus and pertussis to determine whether these patients are in danger of acquiring these infections when naturally exposed. We further sought to investigate the level to which the generally proposed catch-up vaccination schedules were completed in our patients after treatment and determine the factors in patient history that may have affected serologic protection.
We conducted a retrospective trial to assess the immunity of diphtheria, tetatnus and pertussis. To determine the influence of the antineoplastic treatment, we compared antibody status to the previously published data on immunocompetent Korean children (5). For further evaluation patients were divided according to age, sex, underlying disease, treatment regimen, revaccination history after treatment, and then the antibody levels were compared.
A total of 146 patients aged 1-17 yr old who had been treated successfully for pediatric hematologic malignancies, solid tumors, and bone marrow failure were recruited. They had all been diagnosed and received treatment at the Department of Pediatrics, Seoul St. Mary's hospital, which is a tertiary referral center for pediatric cancers in Seoul. All patients were in remission at the time of study. Before the primary diagnosis, all the children had been immunized against diphtheria, tetanus and pertussis according to the Korean national immunization program, with at least three doses of DTaP vaccines within the first year of life. Exclusion criteria included: 1) patients who developed relapse of primary disease or secondary malignancies during the study period; 2) patients who were still receiving systemic steroid for their primary disease or other conditions; and 3) patients with a past history of those listed vaccine-preventable diseases.
Serum antibody concentrations were measured for the following antigens: diphtheria toxoid (DT); tetanus toxoid (TT) and pertussis toxin (PT). Commercially available kits were used for the determination of antibody titers. Serum levels of specific antibodies to diphtheria, tetanus and anti-PT antibody were measured by enzyme-linked immunosorbent assay (ELISA) (IBL, Hamburg, Germany). The thresholds for complete, partial and non protection were taken from national recommendations, literature and manufacturer's guidelines. Levels less than 0.01 IU/mL for anti-DT and anti-TT were interpreted as non-protective level, and levels less than 16 EU/mL for anti-PT as non-protective level. For diphtheria and tetanus, titers of 0.01 to less than 0.1 IU/mL were considered to produce a partial protection, and titers 0.1 IU/mL or greater were deemed to provide complete protection. For pertussis, antibody levels 24 EU/mL or greater were considered as completely protective, and 16 to less than 24 EU/mL as partially protective.
Antibody titers of patient groups and controls were compared with Student's t-test. The methods of chi-square test and Fisher's exact test were applied for comparing seropositive proportions between the groups. Data were analyzed using SPSS statistical software, version 13.0 for Windows (Chicago, IL, USA). P values less than 0.05 were considered statistically significant throughout analysis.
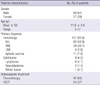
A total 146 patients were recruited in the study. The demographic and clinical characteristics of the patients are shown in Table 1. The current study included 89 males and 57 females with a median age at enrollment of 11.6 ± 3.6 yr old (range, 3-17 yr). One hundred thirty-seven patients (93.8%) had hematologic diseases, including acute lymphoblastic leukemia (ALL) in 83 patients, acute myeloid leukemia (AML) in 39 patients, aplastic anemia in 11 patients and chronic myeloid leukemia (CML) in 4 patients. Nine patients (6.2%) had been treated for solid tumors including 6 for Hodgkin lymphoma, 2 for neuroblastoma, 1 for Wilms' tumor. Amongst all patients, 92 patients had received chemotherapy alone, while 54 patients had also undergone hematopoietic stem cell transplantation (HSCT). Antibody titers for diphtheria, tetanus, and pertussis were measured 3-138 months after the end of treatment.
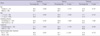
Only 56.8% of the patients had completely protective levels of diphtheria antibody. The percentage of patients with non-protective antibody to diphtheria was 6.2%; and 37% of participants were partially protectective. In comparison with the previous published data in age-matched, healthy Korean children (Group B), the seroprotective rate against diphtheria in our cohort (Group A) was significantly lower (Fig. 1, P < 0.001).
The percentage of seropositivity against diphtheria according to patient characteristics is shown in Table 2. When antibody levels were examined by sex, no differences were observed. Among patients aged 7 yr or older, the proportion of patients with protective antibody levels remained similar to patients younger than 7 yr of age (P = 0.084). The detected antibody levels were not significantly different according to underlying disease of the patient. Analysis of patients who had received chemotherapy only compared with those who had received HSCT again showed no significant differences. The patients who had received DTaP or diphtheria-tetanus (Td) vaccines after completion of therapy were significantly more likely than patients lacking post-treatment reimmunization to have higher protective concentration of diphtheria antibody (P = 0.001).
Sixty percent of the patients had protective levels of antibody to tetanus. The percentage of patients with non-protective antibody to tetanus was 11.6%; and 28.1% of participants were partially protective. A comparative analysis with the immunocompetent group revealed a significant decline in seropositive rate against tetanus in our cohort (Fig. 1).
As was seen with diphtheria antibody, protective levels of antibody to tetanus did not differ according to sex and age. Underlying disease did not significantly influence antibody levels. There were no significant differences between patients treated with chemotherapy alone and those treated by HSCT with regards to antibody levels to tetanus. On comparing the reimmunization group with the non-reimmunization group after treatment, we found a significantly higher number of patients presenting with complete protection to tetanus in the reimmunization group (P < 0.001). Among patients in the reimmunization group, the proportion of those with protective levels of antibody remained stable at approximately 80% (Table 2).
Only twenty-eight percent of the patients had protective levels of anti-PT antibody to pertussis. The percentage of patients with non-protective antibody to pertussis was 62.3%; and 8.9% of participants were partially protectective. The previous data for healthy children revealed that the seroprotection rate against pertussis accounted for 72.4%, whereas the percentage of protective levels significantly dropped to 28.8% in our patients (Fig. 1, P < 0.001).
There was no statistically significant difference in antibody levels with respect to sex and age. The seropositivity of pertussis also did not differ according to underlying disease. The patients who completed chemotherapy only had a lower protective antibody levels than HSCT patients had (P = 0.039).
The disparity in levels of protective antibody between the reimmunization group and non-reimmunization group that had been evident for diphtheria and tetanus was not shown for pertussis. The proportion of patients in recipients of DTaP or Td after completion of therapy with protective levels of antibody to pertussis was not different from the patients in non-reimmunization group (Table 2).
Although survival of children with malignancies has improved, both aggressive antineoplastic treatment and the underlying disease may result in secondary immunodeficiency (6, 7). Owing to the reconstituting immune system, these patients are at risk of acquiring a variety of infectious diseases (8, 9). The recent outbreaks of vaccine preventable disease as well as the increase of pertussis in immunocompetent individuals further address the need for protective strategy in children with hemato-oncologic illnesses (10-15). We therefore assessed the serologic immunity against diphtheria, tetanus and pertussis antigens in a total of 146 children treated for malignancy. In a previous study that we performed at St. Mary's hospital and published in 2008, we have demonstrated the seroprotective rate of diphtheria, tetanus and pertussis in healthy Korean children (5). In this study, we compared the antibody levels in our patient group to those of a healthy historical cohort in order to assess the immunity created by previous vaccinations after therapy. Notably, in the majority of patients these antibody levels were below the presumed threshold of protection for each antigen. Compared with previous data from age-matched normal populations in Korea who had been immunized according to the same schedule, rates of completely protective immunity in our cohort were decreased by 31.5% for diphtheria, 24.9% for tetanus and 43.6% for pertussis, respectively. These data suggest that pediatric patients who had undergone treatment for cancer are highly susceptible to these infections when naturally exposed. Our findings are consistent with other published data. In the report by van der Hardt et al. (16), more than 50% of patients lacked protective immunity against diphtheria and tetanus after antineoplastic therapy. Ek et al. (17) found that only 17% of ALL patients had complete protection against diphtheria and 33% against tetanus after treatment. Small et al. (18) reported that more than 30% of autologous peripheral blood stem cell transplantation recipients lacked pertussis immunity.
We further tried to determine factors influencing the low serologic immunity of our patients. Some studies have demonstrated that young age is associated with more profound immune abnormalities, including loss of antibodies to vaccine antigens (19-21). In our study, however, age did not have any effect on serologic immunity to each antigen. Patient gender and the type of malignancy also did not appear to influence immunity to the vaccine antigens studied.
This study also emphasizes comparisons of immunity between the chemotherapy group and the HSCT group. It is worth noting that immunity to diphtheria and tetanus in patients who had completed chemotherapy only showed no significant differences when compared to that of HSCT recipients. In addition, pertussis immunity decreased significantly more in the chemotherapy group than in the HSCT group. This latter finding may be attributable to widespread use of reimmunization after HSCT. There are well-established recommendations for reimmunizations after HSCT, but no consensus still exists regarding whether reimmunizations are necessary after standard chemotherapy, and when such reimmunizations should take place (22, 23). A few cohort studies were published to address changes of antibody titers and response to booster vaccine after chemotherapy (24-26). On the basis of our data, we agree with the strategy of reimmunizing each patient who completed chemotherapy only, as well as HSCT recipients. Underestimation of the need for reimmunization may contribute to the spread of vaccine preventable diseases such as pertussis in society. Important questions that remain unanswered include the best strategy for managing children who have completed chemotherapy. Zignol et al. who studied humoral immunity against tetanus, measles, polio, hepatitis B, mumps, rubella in pediatric cancer patients recommended a booster dose 12 months after completion of chemotherapy (19). Patel et al. suggested a simple schedule of one booster dose at 6 months after completion of leukemia therapy (25). The proposal by Fioredda et al. was to continue the regular vaccination schedule according to age (27). Efforts to find a common strategy should form the core of future studies.
On comparing the reimmunization group and the non-reimmunization group after treatment, the proportion of patients with protective immunity remained significantly higher in the reimmunization group both for diphtheria (72.9%) and for tetanus (79.7%). However, this difference was not observed for pertussis antibody. This finding reflects the high level of coverage made possible by reimmunization and the requirement that a booster dose of vaccine be given after completion of treatment. Although some of patients were administered reimmunization using DTaP according to age, this finding also suggests that coverage with only Td can be incomplete with regards to pertussis. There are few studies on pertussis immunity following antineoplastic therapy and on the immunogenicity of Tdap in such patients; one study showed that HSCT recipients have lower levels of pertussis antibody and an inadequate response of Tdap vaccination (18). Ongoing prospective study will assist in answering whether observed differences in pertussis immunity can be affected by reimmunization using the newly approved Tdap.
Some limitations of our study must be considered. First, our study has a cross-sectional design, which does not allow us to draw causal relationships. The weak seropositivity in the chemotherapy only group may also be attributable to other factors, including the interval between cessation of treatment and antibody assessment, as is suggested for children who received transplants. We did not have information about antibody levels before treatment to strongly support the idea that the low seropositivity to various vaccine antigens was due only to immunosuppressive effect of therapy. Second, we did not universally test for hypogammaglobulinemia, which may have affected responses. Third, chemotherapy was not classified according to intensity of regimen, a variable which has a significant effect on immune reconstitution. These limitations need to be addressed in future studies.
In summary, we have shown that a substantial proportion of pediatric patients with malignancies who had completed treatment did not have antibody levels that are protective against diphtheria, tetanus and pertussis. The current recommendations by the Korean national immunization program suggest reimmunization of HSCT recipients. Our findings support this reimmunization practice. In addition, although the principle of reimmunization of patients after chemotherapy for malignancy is not universally accepted, these patients also lacked protective serum levels in a manner similar to those who had undergone HSCT, especially against pertussis. Children who demonstrate a defective response to common pediatric vaccines should be evaluated, and revaccinated if indicated, to ensure that these children maintain protective antibody responses. For example, the use of Tdap by a booster vaccine may be one alternative that could be studied further. Future prospective studies should aim towards creating a consensus for modified dosing and reimmunization schedules after treatment for malignancies.
Figures and Tables
Fig. 1
Comparison of seroprotection rates against diphtheria, tetanus, and pertussis between group A (our cohort) and group B (healthy children in previous data).

References
1. Pui CH, Gajjar AJ, Kane JR, Qaddoumi IA, Pappo AS. Medscape. Challenging issues in pediatric oncology. Nat Rev Clin Oncol. 2011. 8:540–549.
2. Alanko S, Pelliniemi TT, Salmi TT. Recovery of blood B-lymphocytes and serum immunoglobulins after chemotherapy for childhood acute lymphoblastic leukemia. Cancer. 1992. 69:1481–1486.
3. Smith S, Schiffman G, Karayalcin G, Bonagura V. Immunodeficiency in long-term survivors of acute lymphoblastic leukemia treated with Berlin-Frankfurt-Münster therapy. J Pediatr. 1995. 127:68–75.
4. Lehrnbecher T, Foster C, Vázquez N, Mackall CL, Chanock SJ. Therapy-induced alterations in host defense in children receiving therapy for cancer. J Pediatr Hematol Oncol. 1997. 19:399–417.
5. Kang JH. The assessment of DTaP vaccine; age related seroepidemiology of diphtheria, tetanus and pertussis in Korea. The annual report of KFDA. 2008. Korea Food & Drug Administration;783–784.
6. Chessells JM, Richards SM, Bailey CC, Lilleyman JS, Eden OB. Gender and treatment outcome in childhood lymphoblastic leukaemia: report from the MRC UKALL trials. Br J Haematol. 1995. 89:364–372.
7. Pui CH, Evans WE. Treatment of acute lymphoblastic leukemia. N Engl J Med. 2006. 354:166–178.
8. Kosmidis S, Baka M, Bouhoutsou D, Doganis D, Kallergi C, Douladiris N, Pourtsidis A, Varvoutsi M, Saxoni-Papageorgiou F, Vasilatou-Kosmidis H. Longitudinal assessment of immunological status and rate of immune recovery following treatment in children with ALL. Pediatr Blood Cancer. 2008. 50:528–532.
9. Kristinsson VH, Kristinsson JR, Jonmundsson GK, Jonsson OG, Thorsson AV, Haraldsson A. Immunoglobulin class and subclass concentrations after treatment of childhood leukemia. Pediatr Hematol Oncol. 2001. 18:167–172.
10. Crespo I, Cardeñosa N, Godoy P, Carmona G, Sala MR, Barrabeig I, Alvarez J, Minguel S, Camps N, Caylà J, Batalla J, Codina G, Domínguez A. Epidemiology of pertussis in a country with high vaccination coverage. Vaccine. 2011. 29:4244–4248.
11. Bell GC, Foster SL. 2010 pertussis outbreak and updated Tdap recommendations. J Am Pharm Assoc (2003). 2011. 51:118–120.
12. Saikia L, Nath R, Saikia NJ, Choudhury G, Sarkar M. A diphtheria outbreak in Assam, India. Southeast Asian J Trop Med Public Health. 2010. 41:647–652.
13. Morrison C, Maurtua-Neumann P, Myint MT, Drury SS, Bégué RE. Pandemic (H1N1) 2009 outbreak at camp for children with hematologic and oncologic conditions. Emerg Infect Dis. 2011. 17:87–89.
14. Buchbinder N, Dumesnil C, Pinquier D, Merle V, Filhon B, Schneider P, Vannier JP. Pandemic A/H1N1/2009 influenza in a paediatric haematology and oncology unit: successful management of a sudden outbreak. J Hosp Infect. 2011. 79:155–160.
15. So JS, Go UY, Lee DH, Park KS, Lee JK. Epidemiological investigation of a measles outbreak in a preschool in Incheon, Korea, 2006. J Prev Med Public Health. 2008. 41:153–158.
16. von der Hardt K, Jüngert J, Beck JD, Heininger U. Humoral immunity against diphtheria, tetanus and poliomyelitis after antineoplastic therapy in children and adolescents: a retrospective analysis. Vaccine. 2000. 18:2999–3004.
17. Ek T, Mellander L, Hahn-Zoric M, Abrahamsson J. Intensive treatment for childhood acute lymphoblastic leukemia reduces immune responses to diphtheria, tetanus, and Haemophilus influenzae type b. J Pediatr Hematol Oncol. 2004. 26:727–734.
18. Small TN, Zelenetz AD, Noy A, Rice RD, Trippett TM, Abrey L, Portlock CS, McCullagh EJ, Vanak JM, Mulligan AM, Moskowitz CH. Pertussis immunity and response to tetanus-reduced diphtheria-reduced pertussis vaccine (Tdap) after autologous peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 2009. 15:1538–1542.
19. Zignol M, Peracchi M, Tridello G, Pillon M, Fregonese F, D'Elia R, Zanesco L, Cesaro S. Assessment of humoral immunity to poliomyelitis, tetanus, hepatitis B, measles, rubella, and mumps in children after chemotherapy. Cancer. 2004. 101:635–641.
20. Nilsson A, De Milito A, Engström P, Nordin M, Narita M, Grillner L, Chiodi F, Björk O. Current chemotherapy protocols for childhood acute lymphoblastic leukemia induce loss of humoral immunity to viral vaccination antigens. Pediatrics. 2002. 109:e91.
21. Urschel S, Cremer S, Birnbaum J, Dallapozza R, Fuchs A, Jager G, Schmitz C, Belohradsky BH, Netz H. Lack of serologic immunity against vaccine-preventable diseases in children after thoracic transplantation. Transpl Int. 2010. 23:619–627.
22. Ljungman P, Engelhard D, de la Cámara R, Einsele H, Locasciulli A, Martino R, Ribaud P, Ward K, Cordonnier C. Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Vaccination of stem cell transplant recipients: recommendations of the Infectious Diseases Working Party of the EBMT. Bone Marrow Transplant. 2005. 35:737–746.
23. Center for Disease Control and Prevention. Infectious Diseases Society of America. American Society of Blood and Marrow Transplantation. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients. Biol Blood Marrow Transplant. 2000. 6:659–713. 715717–727.
24. Yu J, Chou AJ, Lennox A, Kleiman P, Wexler LH, Meyers PA, Gorlick R. Loss of antibody titers and effectiveness of revaccination in post-chemotherapy pediatric sarcoma patients. Pediatr Blood Cancer. 2007. 49:656–660.
25. Patel SR, Ortin M, Cohen BJ, Borrow R, Irving D, Sheldon J, Heath PT. Revaccination of children after completion of standard chemotherapy for acute leukemia. Clin Infect Dis. 2007. 44:635–642.
26. Ercan TE, Soycan LY, Apak H, Celkan T, Ozkan A, Akdenizli E, Kasapçopur O, Yildiz I. Antibody titers and immune response to diphtheria-tetanus-pertussis and measles-mumps-rubella vaccination in children treated for acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2005. 27:273–277.
27. Fioredda F, Plebani A, Hanau G, Haupt R, Giacchino M, Barisone E, Balbo L, Castagnola E. Re-immunisation schedule in leukaemic children after intensive chemotherapy: a possible strategy. Eur J Haematol. 2005. 74:20–23.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download