Abstract
Since laparoscopic liver resection was first introduced in 2001, Korean surgeons have chosen a laparoscopic procedure as one of the treatment options for benign or malignant liver disease. We distributed and analyzed a nationwide questionnaire to members of the Korean Laparoscopic Liver Surgery Study Group (KLLSG) in order to evaluate the current status of laparoscopic liver resection in Korea. Questionnaires were sent to 24 centers of KLLSG. The questionnaire consisted of operative procedure, histological diagnosis of liver lesions, indications for resection, causes of conversion to open surgery, and postoperative outcomes. A laparoscopic liver resection was performed in 416 patients from 2001 to 2008. Of 416 patients, 59.6% had malignant tumors, and 40.4% had benign diseases. A total laparoscopic approach was performed in 88.7%. Anatomical laparoscopic liver resection was more commonly performed than non-anatomical resection (59.9% vs 40.1%). The anatomical laparoscopic liver resection procedures consisted of a left lateral sectionectomy (29.3%), left hemihepatectomy (19.2%), right hemihepatectomy (6%), right posterior sectionectomy (4.3%), central bisectionectomy (0.5%), and caudate lobectomy (0.5%). Laparoscopy-related serious complications occurred in 12 (2.8%) patients. The present study findings provide data in terms of indication, type and method of liver resection, and current status of laparoscopic liver resection in Korea.
Since laparoscopic liver resection was first reported by Reich et al. (1) in 1991, many reports about laparoscopic liver resection have been published. However, laparoscopic liver resection was performed only at a limited number of institutions because of the technical difficulty associated with the procedure.
In Korea, laparoscopic liver resection has been introduced and demonstrated to be safe and effective in selected patients (2). More recently, advances in laparoscopic instruments and increased experience with liver surgery have encouraged Korean surgeons to choose a laparoscopic procedure as one of the treatment options for benign or malignant liver diseases.
Inspired by the encouraging outcomes with this procedure, Korean surgeons who are interested in laparoscopic liver surgery have formed the Korean Laparoscopic Liver Surgery Study Group (KLLSG). This study is a nationwide survey from members of the KLLSG to report the current status of laparoscopic liver resection in Korea.
Despite the different and evolving techniques in each center, the current status of laparoscopic liver resection in Korea was evaluated.
A questionnaire was collected from the surgeons of the KLLSG in 24 centers. The questionnaire consists of operative procedure, histological diagnosis of liver lesions, causes of conversion to open surgery, and indications for laparoscopic liver resection. The surgeons of 19 centers who responded to questionnaires performed 416 laparoscopic liver resections in Korea from 2001 to 2008.
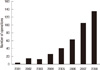
After the introduction of laparoscopic liver resection, there has been an exponential growth in the number of laparoscopic liver resections in Korea. Although there were few cases of laparoscopic liver resection in the early period, the number of cases performed in a year increased rapidly in the late period (Fig. 1).
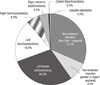
Laparoscopic liver resection including a robotic surgery was performed in 416 patients. The indications for laparoscopic liver resection included benign tumor, liver abscess, intrahepatic duct stones, hepatocellular carcinoma (HCC) and metastatic tumor (Fig. 2). Of the 416 cases, 59.6% were malignant tumors and 40.4% were benign diseases. The majority of the malignant lesions were HCC and metastatic carcinoma (38.0% and 18.5%, respectively). The remainders of the malignant lesions were cholangiocellular carcinoma and mucinous carcinoma. The majority of laparoscopic liver resection for benign diseases was performed for hepatolithiasis (27.4%) and benign tumor (12.0%).
The majority of laparoscopic liver sections were performed with a total laparoscopic approach in 369 patients (88.7%). The laparoscopic assisted procedures or hand assisted procedures were performed in 47 patients (11.3%). Total laparoscopic procedures included 5 robotic assisted liver resections.
The anatomical laparoscopic liver resection was more commonly performed than the non-anatomical resection (59.9% vs 40.1%). The anatomical laparoscopic liver resection procedure consisted of a left lateral sectionectomy in 122 (29.3%) cases, left hemihepatectomy in 80 (19.2%), right hemihepatectomy in 25 (6%), right posterior sectionectomy in 18 (4.3%), central bisectionectomy in 2 (0.5%), and caudate lobectomy in 2 (0.5%) (Fig. 3).
Conversion to open surgery occurred in 42 patients (10.1%): 25 patients due to uncontrolled bleeding, 7 due to inappropriate surgical margin or an obscure location of the lesion, 5 due to anatomic difficulties, 2 due to severe adhesion, 1 due to internal organ injury, and 2 due to tumor rupture and advanced carcinoma.
Serious complications occurred in 12 patients (2.8%). Endoscopic stapler malfunction occurred in 8 patients (1.9%). Myocardial infarction during pneumoperitoneum occurred in 1 (0.2%) patient, CO2 gas embolism in 1 (0.2%), trocar port site bleeding in 1 (0.2%), and cancer recurrence at the trocar site in 1 (0.4%). There were no mortalities.
Most surgeons reported that tumor size was an important indication for laparoscopic liver resection. Of the surgeons, 21% reported that they would perform a laparoscopic liver resection for tumors 3 cm or smaller and 37% for tumors 5 cm or smaller. However, 37% of surgeons reported that they would perform laparoscopic liver resection for HCC, irrespective of tumor size.
More than half of the surgeons (79%) reported that they would perform laparoscopic liver resection for tumors in the peripheral portion of the antero-lateral segments of the liver (segments II, III, V, and VI and the inferior part of IV). However, the others (21%) reported that they would perform laparoscopic liver resection for lesions in the posterior or superior part of the liver (segments I, VII, and VIII and the superior part of IV).
Although laparoscopic surgery has been widely practiced in the field of abdominal surgery, such as colon and gastric surgery, laparoscopic liver resection is still limited in specialized centers. Laparoscopic liver resections demand enough experience in both laparoscopic and open surgery. In addition, it requires advanced laparoscopic surgical techniques associated with parenchymal dissection and hemostasis. With the increased experience with laparoscopic surgery and development in laparoscopic instruments, it has been possible to apply laparoscopic liver resection to various kinds of liver diseases.
Since the introduction of laparoscopic liver resection in Korea (2, 3), there has been an exponential growth of the number of cases treated with the procedure in Korea. It is likely that the numbers of surgeons who apply laparoscopic liver resection will be increasing in the future. In early stages, this procedure was performed in benign disease of the liver. With increasing reports of good outcomes of laparoscopic surgery for malignancy, application of this surgery to malignant disease of the liver has been increased accordingly.
In this study, more than half of the patients (59.6%) underwent laparoscopic surgery for HCC and metastatic cancer. Several studies have shown that survival outcomes of laparoscopic procedures are comparable to those of open surgery. In our series, although there was one case of port site recurrence, there were no peritoneal seeding or perioperative mortality.
Since Azagra et al. (4) performed the first anatomical resection, laparoscopic left lateral sectionectomy has become the standard treatment in some centers (5). In this study, laparoscopic left lateral sectionectomy was the most common procedure of anatomical liver resection. In the near future, laparoscopic left lateral sectionectomy may become the routine procedure in most centers. However, laparoscopic major hepatectomy is not applied worldwide because of the complexity of procedures and fear of uncontrolled bleeding. This procedure is recommended to be performed by an experienced surgeon in the consensus meeting of laparoscopic liver surgery (6). In this study, 105 of the 416 liver resections (25.2%) were performed by major laparoscopic liver resection. This multicenter experience demonstrated that laparoscopic major hepatectomy was feasible and safe in selected patients. Although this study showed that laparoscopic major hepatectomy could be safely performed, this procedure should be reserved for centers with experience in laparoscopic liver resection.
With respect to the operative procedures, total laparoscopic procedures were performed in 88% of the patients, whereas hybrid or hand assisted laparoscopic procedures were performed in 12%, which was lower than reports from other countries (7). Since the introduction of total laparoscopic liver resection in Korea, this procedure has shown good results when compared to open surgery. These good results have encouraged many liver surgeons to follow the pioneer's operative methods (8). Hybrid or hand assisted laparoscopic procedures are easy to apply for surgeons who are accustomed to open surgery. Therefore, we think that hybrid or hand assisted laparoscopic procedures have a role as a bridge procedure of liver resection for a surgeon who is going to start a laparoscopic liver resection program.
Despite the different and evolving techniques in each center, bleeding was the most common reason for conversion. In this study, the conversion rate was 10%, which was similar to previously reported rates (7, 9-12). The incidence of serious complications, such as endoscopic stapler malfunction, ST depression during pneumoperitoneum, CO2 gas embolism, and cancer recurrence at the trocar site were 2.8%. In particular, the incidence of endostapler malfunction was 1.9%, which was comparable with the previously reported rate (13). Recently, many reports have shown that using the stapler device for hepatic resection helped to reduce operation time and bleeding amount during transection of the liver (14, 15). Although we rarely encountered stapler malfunction, the operator should use stapling devices properly and be cautious of abnormal feelings during the stapling manipulation.
In the early stage, laparoscopic liver resection applied only to lesions located in the left lateral or peripheral segments. Due to the difficulty of bleeding control and visualization of the surgical fields, lesions in the deep or posterior sections in the liver (segments I, VII, and VIII and the superior part of IV) were previously considered to be poor indications for laparoscopic liver resection (16-18). Moreover, it would be difficult to obtain a safety tumor margin for the inferior portion of the tumor when the tumor was located in the posterior and superior parts. However, recent reports have demonstrated the feasibility and safety of laparoscopic liver resection of the lesions in those locations (19, 20). In our study, over 20% of surgeons answered that they would apply the procedure even in segments I, VII, and VIII and the superior part of IV. We expect the lesions located in the posterior or superior part of the liver may be candidates for laparoscopic resection in the future.
In this study, we introduce a national survey about laparoscopic liver surgery in Korea. With the national survey, a large number of patients were included in this study, and a wide range of disease types and operation procedures could be evaluated. However, a limitation may arise. There were some centers that have not responded to this survey, and there might be a concern in terms of whether the data entirely represented the Korean status of laparoscopic liver resection. Despite the limitation, the results of this survey provide data in terms of indication, type and method of liver resection, and current status of laparoscopic liver resection. We believe that laparoscopic liver resection is a new treatment strategy for the treatment of liver tumors in many hospitals in Korea. The Korean Laparoscopic Liver Surgery Study Group plans to conduct further surveys to propose standardization of laparoscopic liver resection for HCC.
Figures and Tables
References
1. Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991. 78:956–958.
2. Min SK, Han HS, Kim YW, Choi YM. Laparoscopy-assited major liver resection. J Korean Soc Endosc Laparosc Surg. 2002. 5:75–79.
3. Hong TH, Lee SK, Park SC, Kim WW, Jeon HM, Kim EK. Laparoscopic liver resection: different methods. J Korean Soc Endosc Laparosc Surg. 2002. 5:37–43.
4. Azagra JS, Goergen M, Gilbart E, Jacobs D. Laparoscopic anatomical (hepatic) left lateral segmentectomy-technical aspects. Surg Endosc. 1996. 10:758–761.
5. Chang S, Laurent A, Tayar C, Karoui M, Cherqui D. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg. 2007. 94:58–63.
6. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009. 250:825–830.
7. Tsuchiya M, Otsuka Y, Tamura A, Nitta H, Sasaki A, Wakabayashi G, Kaneko H. Status of endoscopic liver surgery in Japan: a questionnaire survey conducted by the Japanese Endoscopic Liver Surgery Study Group. J Hepatobiliary Pancreat Surg. 2009. 16:405–409.
8. Min SK, Han HS, Lee HK, Jie S, Yu K, Yi NJ, Choi YM. Totally laparoscopic anatomic liver resection. J Korean Surg Soc. 2003. 64:390–395.
9. Koffron AJ, Auffenberg G, Kung R, Abecassis M. Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg. 2007. 246:385–392.
10. Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A. Laparoscopic versus open hepatic resections for benign and malignant neoplasms: a meta-analysis. Surgery. 2007. 141:203–211.
11. Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F. Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc. 2008. 22:2208–2213.
12. Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009. 16:410–421.
13. Chan D, Bishoff JT, Ratner L, Kavoussi LR, Jarrett TW. Endovascular gastrointestinal stapler device malfunction during laparoscopic nephrectomy: early recognition and management. J Urol. 2000. 164:319–321.
14. Gumbs AA, Gayet B, Gagner M. Laparoscopic liver resection: when to use the laparoscopic stapler device. HPB (Oxford). 2008. 10:296–303.
15. Rowe AJ, Meneghetti AT, Schumacher PA, Buczkowski AK, Scudamore CH, Panton ON, Chung SW. Perioperative analysis of laparoscopic versus open liver resection. Surg Endosc. 2009. 23:1198–1203.
16. Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000. 232:753–762.
17. Dulucq JL, Wintringer P, Stabilini C, Berticelli J, Mahajna A. Laparoscopic liver resections: a single center experience. Surg Endosc. 2005. 19:886–891.
18. Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003. 138:763–769.
19. Cho JY, Han HS, Yoon YS, Shin SH. Experiences of laparoscopic liver resection including lesions in the posterosuperior segments of the liver. Surg Endosc. 2008. 22:2344–2349.
20. Han HS, Cho JY, Yoon YS. Techniques for performing laparoscopic liver resection in various hepatic locations. J Hepatobiliary Pancreat Surg. 2009. 16:427–432.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download