Abstract
The serial transverse enteroplasty (STEP) procedure is a novel technique to lengthen and taper the bowel in patients with short bowel syndrome. The advantages of STEP include not only technical ease and simplicity, but also the ability to repeat the procedure. Herein, we report a case of extreme short bowel syndrome that was successfully treated by the second STEP procedure. A 3-day old newborn girl underwent STEP because of jejunal atresia with the small bowel length of 15 cm, but her bowel elongation was not enough to escape from short bowel syndrome. At the age of 6 months, she underwent a second STEP procedure. The bowel lengthening by the second STEP made her tolerable to enteral feeding with body weight gain and rescued her from short bowel syndrome. This case showed that second STEP is very helpful in treatment of extreme short bowel syndrome.
Since the introduction of serial transverse enteroplasty (STEP) in 2003 (1), this procedure has become popular in the surgical management of short bowel syndrome because of its easy and simple operative technique (2, 3). However, in cases of extreme short bowel, the lengthening of the bowel from one STEP is not enough to escape from short bowel syndrome. Recent studies have reported that STEP could be performed again as a second procedure after primary STEP (4-7).
Herein, we present a case of extreme short bowel syndrome that was successfully treated by the second STEP procedure.
A 2.63-kg, 36-week gestation female neonate was born by elective cesarean delivery. At the third day of life, she underwent laparotomy and high jejunal atresia was found (Fig. 1). The proximal bowel was only 10 cm in length from the Treitz ligament with dilatation, and the distal bowel was 5 cm in length from the ileocecal valve. STEP was performed using 6 Endo GIA staplers on the proximal small bowel that resulted in an increase in intestinal length from 10 cm to 15 cm. The entire small bowel length was 20 cm after primary anastomosis with the distal small bowel (Fig. 2). Postoperatively, parenteral nutrition was discontinued because of cholestatic jaundice, but she was able to gain weight very slowly by enteral feeding, even though she needed intravenous electrolyte solution to prevent dehydration. By 6 months of age, the patient's body weight had increased to 3.71 kg, but she still required intravenous electrolyte solution and her small bowel was dilated again. As a result, we decided to perform the second STEP. The patient had relatively even dilatation of the small bowel with 4-5 cm in width. The previous proximal small bowel had gained length, from 15 cm to 30 cm, and the distal small bowel had grown from 5 cm to 12 cm. The second STEP was performed using 5 Endo GIA staplers on the previous proximal small bowel that resulted in an increase in intestinal length from 30 cm to 45 cm. The entire small bowel length was 57 cm (Fig. 3). After the second STEP procedure, the patient was tolerable to enteral feeding with body weight gain. At 8 months of age (2 months after the second STEP), her body weight was 4.41 kg after weaning the intravenous fluid, and she was discharged from the hospital. At the age of 2 yr, she has shown good growth and her body weight has increased to 9.8 kg, although her body weight is still in the low percentile of the growth chart (4th percentile) and she has developed vitamin D deficiency.
In the management of short bowel syndrome, the length of the small intestine is one of the important treatment factors (8). Although few reports have shown successful results in the short segment of the intestine, favorable outcomes are usually seen in cases of relatively long segments of intestine (9). For this reason, various types of intestinal lengthening procedures have been developed (10-12). STEP, the most recently developed method, is favored for its simple technical feasibility (3). Originally this procedure was designed for longstanding short bowel syndrome patients with a dilated small bowel, and it could easily be adapted to newborn patients who have proximal jejunal atresia with short dilated residual small bowel (6, 13), such as our case.
However, in cases of extreme short bowel, bowel lengthening by STEP has not been enough to escape from short bowel syndrome, and subsequent TPN and its complication would still bes a major risk factor of survival. In such cases, the second STEP is a very helpful procedure. After animal studies of second STEP (7), several reports revealed and supported its advantages (4-6). This procedure offers not only the original advantages of technical ease and simplicity, but it also apparently has the benefit of additional intestinal length. The intestinal elongation produced by second STEP could be a critical length of intestine in treating short bowel syndrome. Our case also supports the utility of second STEP. In our study, the patient was able to survive without TPN after the first STEP, but her bowel length was not enough to escape from short bowel syndrome. Although natural growth of the small bowel would be helpful in managing short bowel syndrome, elongation of the small bowel length by the second STEP would be critical lengthening to rescue the patient from short bowel syndrome.
While our second STEP was performed without major difficulties, several points of caution must be noted. First, application of the stapler should be safe from ischemic bowel changes. Deformed mesenteric blood supply and uneven dilatation of the bowel, which had happened after the first STEP in our case, are problematic to staple firing. The surgeon has to ensure that the blood supply between each staple line is not injured by the staples. Second, there are few options for placing the staple lines to make a uniform diameter of bowel and reduce the blind ends (4-7). We adopted a simple addition of staple line between previous staple lines without further modification. Because of limitations of previous studies, it is difficult to recommend the best method of making staple lines, but it should be tailored to individual cases. In addition to these concerns, unquestionably, abdominal exploration should be performed very carefully to avoid unexpected injury to the bowel.
Our case was successful in weaning the patient off the TPN and freeing her from intravenous fluid by the second STEP. However, the patient is still in a very low percentile in body weight and height. She also has vitamin D deficiency, which probably originated from the short length of her bowel. This indicates that nutritional evaluation and support should be an essential part of management, even when the second STEP is successful.
Figures and Tables
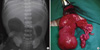
Fig. 1
High jejunal atresia. (A) Abdominal radiography showing distension of the proximal jejunum and (B) an intraoperative photograph showing the proximal jejunum and the distal ileum.
References
1. Kim HB, Fauza D, Garza J, Oh JT, Nurko S, Jaksic T. Serial transverse enteroplasty (STEP): a novel bowel lengthening procedure. J Pediatr Surg. 2003. 38:425–429.
2. Modi BP, Javid PJ, Jaksic T, Piper H, Langer M, Duggan C, Kamin D, Kim HB;. First report of the international serial transverse enteroplasty data registry: indications, efficacy, and complications. J Am Coll Surg. 2007. 204:365–371.
3. Javid PJ, Kim HB, Duggan CP, Jaksic T. Serial transverse enteroplasty is associated with successful short-term outcomes in infants with short bowel syndrome. J Pediatr Surg. 2005. 40:1019–1023.
4. Morikawa N, Kuroda T, Kitano Y, Tanaka H, Takayasu H, Fujino A, Shibata Y, Tanemura H, Muto M, Honna T. Repeat STEP procedure to establish enteral nutrition in an infant with short bowel syndrome. Pediatr Surg Int. 2009. 25:1007–1011.
5. Andres AM, Thompson J, Grant W, Botha J, Sunderman B, Antonson D, Langnas A, Sudan D. Repeat surgical bowel lengthening with the STEP procedure. Transplantation. 2008. 85:1294–1299.
6. Ehrlich PF, Mychaliska GB, Teitelbaum DH. The 2 STEP: an approach to repeating a serial transverse enteroplasty. J Pediatr Surg. 2007. 42:819–822.
7. Piper H, Modi BP, Kim HB, Fauza D, Glickman J, Jaksic T. The second STEP: the feasibility of repeat serial transverse enteroplasty. J Pediatr Surg. 2006. 41:1951–1956.
8. Spencer AU, Neaga A, West B, Safran J, Brown P, Btaiche I, Kuzma-O'Reilly B, Teitelbaum DH. Pediatric short bowel syndrome: redefining predictors of success. Ann Surg. 2005. 242:403–409.
9. Sigalet DL. Short bowel syndrome in infants and children: an overview. Semin Pediatr Surg. 2001. 10:49–55.
10. Bianchi A. Intestinal loop lengthening: a technique for increasing small intestinal length. J Pediatr Surg. 1980. 15:145–151.
11. Kimura K, Soper RT. A new bowel elongation technique for the short-bowel syndrome using the isolated bowel segment Iowa models. J Pediatr Surg. 1993. 28:792–794.
12. Georgeson K, Halpin D, Figueroa R, Vincente Y, Hardin W Jr. Sequential intestinal lengthening procedures for refractory short bowel syndrome. J Pediatr Surg. 1994. 29:316–320.
13. Wales PW, Dutta S. Serial transverse enteroplasty as primary therapy for neonates with proximal jejunal atresia. J Pediatr Surg. 2005. 40:E31–E34.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download