Abstract
Multiple RBC transfusions inevitably lead to a state of iron overload before and after high-dose chemotherapy and autologous stem cell transplantation (HDCT/autoSCT). Nonetheless, iron status during post-SCT follow-up remains unknown. Therefore, we investigated post-SCT ferritin levels, factors contributing to its sustained levels, and organ functions affected by iron overload in 49 children with high-risk neuroblastoma who underwent tandem HDCT/autoSCT. Although serum ferritin levels gradually decreased during post-SCT follow-up, 47.7% of the patients maintained ferritin levels above 1,000 ng/mL at 1 yr after the second HDCT/autoSCT. These patients had higher serum creatinine (0.62 vs 0.47 mg/mL, P = 0.007) than their counterparts (< 1,000 ng/mL). Post-SCT transfusion amount corresponded to increased ferritin levels at 1 yr after the second HDCT/autoSCT (P < 0.001). A lower CD34+ cell count was associated with a greater need of RBC transfusion, which in turn led to a higher serum ferritin level at 1 yr after HDCT/autoSCT. The number of CD34+ cells transplanted was an independent factor for ferritin levels at 1 yr after the second HDCT/autoSCT (P = 0.019). Consequently, CD34+ cells should be transplanted as many as possible to prevent the sustained iron overload after tandem HDCT/autoSCT and consequent adverse effects.
The use of high-dose chemotherapy in conjunction with autologous stem cell transplantation (HDCT/autoSCT) has been demonstrated to increase the survival rate of children with high-risk solid tumors (1). Several researchers have recently shown that tandem HDCT/autoSCT may also be a feasible method of improving the treatment outcome (2-5). This approach is based on the underlying hypothesis that additional dose escalation is likely to further enhance the survival of children with high-risk solid tumors. Patients who undergo HDCT/autoSCT generally require frequent RBC transfusions not only during induction chemotherapy but also during post-SCT period until engraftment. Consequently, high-risk solid tumor patients who have received tandem HDCT/autoSCT generally experience iron overload. Dose escalation during tandem HDCT/autoSCT may also be associated with higher frequencies of acute and chronic toxicities, including toxicities from iron overload.
Much attention has been given to acute adverse effects of early post-SCT iron overload including hepatic veno-occlusive disease, infections, and idiopathic pneumonia syndrome (3, 4). Elevated serum ferritin level has also corresponded to increased SCT-related mortality and decreased overall survival rate (4-8). However, late adverse effects of post-SCT iron overload remain inconclusive. While detrimental effects of transfusional iron overload including abnormal liver function test, hepatic fibrosis/cirrhosis, cardiac dysfunction, and susceptibility to infection have been suggested in patients with chronic acquired anemias (9, 10), the effects of transfusional iron overload during post-SCT follow-up period remain unclear.
As SCT recipients do not require RBC transfusion after engraftment, their iron levels are expected to decrease over time, particularly in growing children, unlike chronic anemia patients who require life-long transfusion and thus have sustained iron overload. Nevertheless, when iron overload is sustained in SCT recipients, its adverse effects may be more pronounced than in chronic anemia patients, either in onset or severity, due to previous cytotoxic chemoradiotherapy. However, iron status in children during follow-up after tandem HDCT/autoSCT and its adverse effects are, to our knowledge, unknown. Therefore, the present study investigated the trend of iron levels at various time points during follow-up for more than 3 yr after tandem HDCT/autoSCT in children with high-risk neuroblastoma and factors contributing to its sustained levels, as well as major organ functions affected by iron overload.
Children with high-risk neuroblastoma who underwent tandem HDCT/autoSCT between January 2006 and June 2010 were eligible for the present retrospective analysis. Intermediate-risk patients with relapsed tumor or intermediate-risk patients showing inadequate response to conventional chemoradiotherapy also underwent tandem HDCT/autoSCT and were eligible for the study.
Patients received nine cycles of induction chemotherapy prior to tandem HDCT/autoSCT. The CEDC and ICE regimens were used in an alternating manner (Table 1). Definitive surgery was performed after the sixth chemotherapy cycle except for those patients who had undergone a surgical resection before the administration of induction chemotherapy. Each chemotherapy cycle was scheduled to be 28 days apart, but delays less than 2 weeks were permitted to allow the absolute neutrophil count (ANC) and platelet count to recover to 1,000/µL and 100,000/µL, respectively. If chemotherapy was delayed for more than 2 weeks, doses were reduced by 25% of the calculated dose.
After the completion of induction therapy, patients underwent tandem HDCT/autoSCT. Table 1 lists the HDCT regimens. Briefly, CEC regimen was employed for the first HDCT. The regimens for the second HDCT were TM-TBI or TM in the early period (until December 2009) and high-dose 131I-MIBG (metaiodobenzylguanidine)-TM or TM in the late period (from January 2010). TBI or high-dose 131I-MIBG treatment was included in the second HDCT only for stage 4 patients. There was a 12-week interval between the first and second HDCT/autoSCT. Approximately half of the collected peripheral blood stem cells were infused for marrow rescue at each HDCT session.
Generally, irradiated, packed RBCs were transfused when hemoglobin level fell below 8.0 g/dL. Nevertheless, we tried to maintain a hemoglobin level over 10.0 g/dL if the patient underwent surgery, suffered from high fever, or required oxygen supply for any reason. Normally, 10 mL/kg of RBCs were transfused each time. No patient received iron chelation treatment during or after tandem HDCT/autoSCT in the present study.
Serum ferritin was measured before each HDCT/autoSCT and at 1, 3, 6, 9, 12, 16, 20, 24, 30, and 36 months after the second HDCT/autoSCT. Serum ferritin levels in patients with relapsed tumor during follow-up after tandem HDCT/autoSCT were excluded from analysis because tumor relapse and treatment after relapse can affect serum ferritin level.
Major organ functions were evaluated at 1 yr after the second HDCT/autoSCT. Chest X-ray, electrocardiogram, and echocardiogram were performed to determine cardiac and pulmonary functions. Renal glomerular and tubular functions were also evaluated. Growth hormone, thyroid hormone, cortisol, and sex hormone levels were measured to assess endocrine function. Ophthalmological and auditory functions were also examined. Patients who had a relapsed tumor within 1 yr after tandem HDCT/autoSCT were excluded from organ function analysis since they received salvage treatment after relapse, which can deteriorate organ function. Organ dysfunction was assessed using the Common Toxicity Criteria of National Cancer Institute of the USA. Major organ functions at 1 yr after the second HDCT/autoSCT were compared according to the ferritin level (> 1,000 vs < 1,000 ng/mL) at 1 yr after the second HDCT/autoSCT.
Differences in the frequencies of various toxicities between the two groups according to the ferritin level were analyzed using the Pearson chi-square test. Spearman test was performed to evaluate the correlation between the two continuous variables. Differences in the continuous variables between the two groups were compared using the Mann-Whitney U-test. Multivariate analysis was also performed using linear regression analysis to examine the factors associated with ferritin levels at 1 yr after the second HDCT/autoSCT. P values < 0.05 were considered significant.
During study period, 49 neuroblastoma patients underwent tandem HDCT/autoSCT. Forty-one of them had high-risk neuroblastoma, 5 had intermediate-risk neuroblastoma showing inadequate response to induction treatment, and the remaining 3 had relapsed neuroblastoma. The age at diagnosis or relapse was a median of 31 (range 1-120) months. Thirty-five patients had a stage 4 tumor, 17 had a MYCN amplified tumor, and 25 had a tumor with unfavorable histology.
The cumulative RBC transfusion amount prior to the first HDCT/autoSCT was a median of 166 (range 77-251) mL/kg. RBC transfusion amount between the first and second HDCT/autoSCT was a median of 38 (range 16-190) mL/kg with the cumulative RBC transfusion amount prior to the second HDCT/autoSCT being a median of 213 (range 94-352) mL/kg. RBC transfusion amount for 1 yr after the second HDCT/autoSCT was a median of 65 (range 0-580) mL/kg with the cumulative RBC transfusion amount until 1 yr after the second HDCT/autoSCT being a median of 286 (range 91-895) mL/kg.
Median serum ferritin levels prior to the first and second HDCT/autoSCT were 1,389 (range 226-2,629) ng/mL and 1,205 (range 129-3,040) ng/mL, respectively. Serum ferritin level peaked at one month after the second HDCT/autoSCT (median 2,297 ng/mL) and steadily decreased to a median of 285 ng/mL at 36 months after the second HDCT/autoSCT without iron chelation. However, ferritin level at 1 yr after the second HDCT/autoSCT remained high at a median of 792 (range 52-4,652) ng/mL and 47.7% of the patients had ferritin levels greater than 1,000 ng/mL (Fig. 1A, B). Serum ferritin level at 1 yr after the second HDCT/autoSCT had a positive correlation with RBC transfusion amount during 1 yr after the second HDCT/autoSCT (P < 0.001, Fig. 1C).
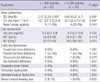
Table 2 lists grade 3/4 organ dysfunction at 1 yr after the second HDCT/autoSCT according to ferritin levels at 1 yr after the second HDCT/autoSCT (< 1,000 vs > 1,000 ng/mL). There was no difference in serum creatinine and creatinine clearance levels prior to the second HDCT/autoSCT between the two groups. However, serum creatinine level was significantly higher in patients with high ferritin levels than their counterparts (median 0.62 vs 0.47 mg/mL, P = 0.007), and similarly, creatinine clearance was lower than their counterparts with borderline significance (52.2 vs 70.1 mL/min/1.73m2, P = 0.087) (Fig. 2A). There was no difference in the frequency of renal tubular dysfunction. Alanine aminotransferase level was also higher in patients with high ferritin levels (P = 0.011, Fig. 2B), even though its clinical significance might not be significant. Otherwise, there was no difference in the frequencies of organ dysfunctions between the two groups.
A median of 2.3 (range 0.6-15.6) × 106 CD34+ cells/kg were infused for the first HDCT/autoSCT, and the median times required to reach an ANC of 500/µL and a platelet count of 20,000/µL without transfusion for the previous 7 days were 11 days (range 8-35) and 25 days (range 15-68), respectively. A median of 2.4 (range 1.0-16.0) × 106 CD34+ cells/kg were infused for the second HDCT/autoSCT and the median times required to reach an ANC of 500/µL and a platelet count of 20,000/µL were 11 days (range 7-16) and 36.5 days (range 14-322), respectively.
A less number of CD34+ cells (< 2 × 106/kg) in the second HDCT/autoSCT was associated with a slower recovery of neutrophil and platelet (median 12 vs 10 days, P < 0.001; median 115 vs 21.5 days, P < 0.001). In addition, it was associated with a greater amount of RBC transfusion for 1 yr after the second HDCT/autoSCT (P = 0.003, Fig. 3A) and accordingly, a higher ferritin level at 1 yr after the second HDCT/autoSCT (P = 0.005, Fig. 3B).
Age older than 3 yr at the second HDCT/autoSCT, inclusion of TBI in the second HDCT/autoSCT, and transplantation with low number of CD34+ cells (< 2 × 106/kg) were associated with greater RBC transfusion amount for 1 yr after the second HDCT/autoSCT and higher ferritin levels at 1 yr after the second HDCT/autoSCT in the univariate analysis (Table 3). In the multivariate analysis, low number of CD34+ cells (< 2 × 106/kg) in the second HDCT/autoSCT was the only independent factor for greater RBC transfusion amount for 1 yr after the second HDCT/autoSCT and higher ferritin levels at 1 yr after the second HDCT/autoSCT (P = 0.026 and P = 0.019, respectively).
In the past, much research had been focused on iron overload and its adverse effects caused solely by multiple blood transfusions in diseases such as beta-thalassemia major and other chronic anemia (11-13). Recently, as the number of survivors with high-risk malignancy increases, particularly after SCT which requires multiple transfusions during pre- and post-SCT period, iron overload has become an increasingly important risk factor for outcome in these patients (14). Iron overload in SCT recipients may have different, more severe manifestations and must therefore be evaluated differently from that in chronic anemia patients who do not receive chemoradiotherapy. It is well established that a higher pre-SCT iron level is associated with more frequent various toxicities during SCT and a higher toxic death rate (15-17). However, studies for iron status and its late adverse effects during post-SCT follow-up are very limited (18). Thus, our primary objective was to demonstrate the trend of iron levels during follow-up at various time points after tandem HDCT/autoSCT in children with high-risk neuroblastoma and factors contributing to its sustained levels, as well as major organ functions affected by iron overload.
Because HDCT/autoSCT recipients do not need RBC transfusion after engraftment, iron levels are expected to decrease over time, particularly in growing children. Indeed, ferritin levels steadily decreased without iron chelation after HDCT/autoSCT in the present study. Nevertheless, when the number of CD34+ cells transplanted was low, patients required prolonged RBC transfusion after HDCT/autoSCT, and accordingly, their ferritin levels at 1 yr after tandem HDCT/autoSCT were high. There was a strong correlation between the number of CD34+ cells and RBC transfusion amount during the post-SCT period. A lower CD34+ cell number was associated with a greater need of RBC transfusion, which in turn led to higher serum ferritin levels at 1 yr after tandem HDCT/autoSCT. The number of CD34+ cells was an independent factor affecting the ferritin level at 1 yr after tandem HDCT/autoSCT. Most clinical reports concerning SCT have used neutrophil and platelet recovery as parameters for hematologic recovery after SCT. However, findings in the present study suggest that RBC recovery should also be considered as a significant parameter assessing the hematologic recovery and outcome after SCT.
About half of the patients in the present study maintained ferritin levels > 1,000 ng/mL at 1 yr after the tandem HDCT/autoSCT. In these patients, renal glomerular function was significantly worse than their counterparts (ferritin levels < 1,000 ng/mL) at 1 yr after tandem HDCT/autoSCT. There was no difference in glomerular function prior to HDCT/autoSCT between the two groups. These findings suggest a possible correlation between high ferritin levels and impairment of glomerular function during post-SCT follow-up. However, at present, it is not clear if hyperferritinemia is directly responsible for impaired glomerular function during post-SCT follow-up because all of our patients had received intensive induction and HDCT with various nephrotoxic agents, and therefore might already have subclinical renal dysfunction after tandem HDCT/autoSCT. Longer follow-up and a larger cohort of patients may be needed to elucidate if heperferritinemia is responsible for impairment of glomerular function during post-SCT follow-up.
We previously showed that deferasirox treatment prior to tandem HDCT/autoSCT is effective at lowering pre-SCT serum ferritin levels, thereby lowering the frequency of hepatic veno-occlusive disease and infection during tandem HDCT/autoSCT in children with neuroblastoma and brain tumors (19). However, at present, experience of iron chelation treatment after SCT, particularly with deferasirox, is very limited. Elevation of serum creatinine levels during deferasirox treatment has frequently been reported (19, 20), and the US Food and Drug Administration (FDA) black box warning for deferasirox includes renal failure (21). This poses as a challenge in using deferasirox to treat iron overload in HDCT/autoSCT recipients, as they may be more susceptible to possible adverse effects of iron chelation treatment than chronic anemia patients due to previous chemoradiotherapy. Furthermore, the present study showed that renal glomerular function at 1 yr after tandem HDCT/autoSCT was already lower in patients with high ferritin levels. Taken together, findings in the present study suggest that the use of iron chelators such as deferasirox should be approached with caution in patients who underwent HDCT/autoSCT.
We used serum ferritin as a measure of iron overload in the present study because repeated measurements can be performed without difficulty to establish trends in iron burden over time. However, previous publications have suggested that this may not be a reliable indicator of iron overload (22). Serum ferritin may be increased due to liver dysfunction, may act as an acute phase reactant of infectious complications, and may be increased in other SCT-related complications. More specific measures of iron overload include liver MRI and liver biopsy. Therefore, it may be important in further testing our hypothesis to use liver biopsy or MRI to better quantify iron overload.
In summary, we demonstrated for the first time that ferritin levels sustained high even at 1 yr after tandem HDCT/autoSCT when the number of CD34+ cells transplanted was low, and accordingly, patients required prolonged RBC transfusion after HDCT/autoSCT. We acknowledge the limitations present in our small single-institution study and believe that further validation in patients with other solid tumors and a longer follow-up period for assessing organ function are necessary. Nonetheless, our results strongly support the notion that further modalities of collecting more CD34+ cells must be researched in order to reduce RBC transfusion amount, lower ferritin level, and possibly decrease organ dysfunction related to iron overload in patients with high-risk solid tumors.
Figures and Tables
Fig. 1
Serum ferritin during post-SCT follow-up. (A) Serum ferritin level peaks at one month after the second HDCT/autoSCT and steadily decreases without iron chelation. (B) Ferritin level at 1 yr after the second HDCT/autoSCT remaines high and 47.7% of the patients had ferritin levels greater than 1,000 ng/mL. (C) Serum ferritin level at 1 yr after the second HDCT/autoSCT has a positive correlation with RBC transfusion amount during 1 yr after the second HDCT/autoSCT.

Fig. 2
Organ dysfunction at 1 yr after the second HDCT/autoSCT. There was no difference in major organ function prior to the second HDCT/autoSCT between the two groups. However, serum creatinine level (A) and alanine aminotransferase level (B) are significantly higher in patients with high ferritin levels at 1 yr after the second HDCT/autoSCT.

Fig. 3
Transfusion amount and serum ferritin according to the number of CD34+ cells. A less number of CD34+ cells (< 2 × 106/kg) in the second HDCT/autoSCT is associated with a greater amount of RBC transfusion for 1 yr after the second HDCT/autoSCT (A), and accordingly, a higher ferritin level at 1 yr after the second HDCT/autoSCT (B).

References
1. Gilman AL, Jacobsen C, Bunin N, Levine J, Goldman F, Bendel A, Joyce M, Anderson P, Rozans M, Wall DA, Macdonald TJ, Simon S, Kadota RP. Phase I study of tandem high-dose chemotherapy with autologous peripheral blood stem cell rescue for children with recurrent brain tumors: a Pediatric Blood and Marrow Consortium study. Pediatr Blood Cancer. 2011. 57:506–513.
2. Chen AR, Civin CI. Blume KJ, Forman SJ, Appelbaum FR, editors. Hematopoietic cell transplantation for pediatric patients with solid tumors. Thomas' hematopoietic cell transplantation. 2004. Massachusetts: Blackwell;1354–1368.
3. Koreth J, Antin JH. Iron overload in hematologic malignancies and outcome of allogeneic hematopoietic stem cell transplantation. Haematologica. 2010. 95:364–366.
4. Lee SH, Yoo KH, Sung KW, Koo HH, Kwon YJ, Kwon MM, Park HJ, Park BK, Kim YY, Park JA, Im HJ, Seo JJ, Kang HJ, Shin HY, Ahn HS. Hepatic veno-occlusive disease in children after hematopoietic stem cell transplantation: incidence, risk factors, and outcome. Bone Marrow Transplant. 2009. 45:1287–1293.
5. de Witte T. The role of iron in patients after bone marrow transplantation. Blood Rev. 2008. 22:S22–S28.
6. Altès A, Remacha AF, Sureda A, Martino R, Briones J, Canals C, Brunet S, Sierra J, Gimferrer E. Iron overload might increase transplant-related mortality in haematopoietic stem cell transplantation. Bone Marrow Transplant. 2002. 29:987–989.
7. Carmine TC, Evans P, Bruchelt G, Evans R, Handgretinger R, Niethammer D, Halliwell B. Presence of iron catalytic for free radical reactions in patients undergoing chemotherapy: implications for therapeutic management. Cancer Lett. 1995. 94:219–226.
8. Halliwell B, Gutteridge JM, Cross CE. Free radicals, antitoxidants, and human disease: where are we now? J Lab Clin Med. 1992. 119:598–620.
9. Jensen PD, Jensen FT, Christensen T, Nielsen JL, Ellegaard J. Relationship between hepatocellular injury and transfusional iron overload prior to and during iron chelation with desferrioxamine: a study in adult patients with acquired anemias. Blood. 2003. 101:91–96.
10. Malcovati L, Porta MG, Pascutto C, Invernizzi R, Boni M, Travaglino E, Passamonti F, Arcaini L, Maffioli M, Bernasconi P, Lazzarino M, Cazzola M. Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J Clin Oncol. 2005. 23:7594–7603.
11. Flanagan JM, Steward S, Hankins JS, Howard TM, Neale G, Ware RE. Microarray analysis of liver gene expression in iron overloaded patients with sickle cell anemia and beta-thalassemia. Am J Hematol. 2009. 84:328–334.
12. Harmatz P, Butensky E, Quirolo K, Williams R, Ferrell L, Moyer T, Golden D, Neumayr L, Vichinsky E. Severity of iron overload in patients with sickle cell disease receiving chronic red blood cell transfusion therapy. Blood. 2000. 96:76–79.
13. Files B, Brambilla D, Kutlar A, Miller S, Vichinsky E, Wang W, Granger S, Adams RJ. Longitudinal changes in ferritin during chronic transfusion: a report from the Stroke Prevention Trial in Sickle Cell Anemia (STOP). J Pediatr Hematol Oncol. 2002. 24:284–290.
14. Majhail NS, Lazarus HM, Burns LJ. Iron overload in hematopoietic cell transplantation. Bone Marrow Transplant. 2008. 41:997–1003.
15. Koreth J, Antin JH. Iron overload in hematologic malignancies and outcome of allogeneic hematopoietic stem cell transplantation. Haematologica. 2010. 95:364–366.
16. Strasser SI, Kowdley KV, Sale GE, McDonald GB. Iron overload in bone marrow transplant recipients. Bone Marrow Transplant. 1998. 22:167–173.
17. Bazuave GN, Buser A, Gerull S, Tichelli A, Stern M. Prognostic impact of iron parameters in patients undergoing allo-SCT. Bone Marrow Transplant. 2012. 47:60–64.
18. Butt NM, Clark RE. Autografting as a risk factor for persisting iron overload in long-term survivors of acute myeloid leukaemia. Bone Marrow Transplant. 2003. 32:909–913.
19. Chueh HW, Sung KW, Lee SH, Yoo KH, Koo HH, Kim JY, Cho EJ. Iron chelation treatment with deferasirox prior to high-dose chemotherapy and autologous stem cell transplantation may reduce the risk of hepatic veno-occlusive disease in children with high-risk solid tumors. Pediatr Blood Cancer. 2012. 58:441–447.
20. Delforge M, Selleslag D, Triffet A, Mineur P, Bries G, Graux C, Trullemans F, MacDonald K, Abraham I, Pluymers W, Ravoet C. Iron status and treatment modalities in transfusion-dependent patients with myelodysplastic syndromes. Ann Hematol. 2011. 90:655–666.
21. Cappellini MD, Cohen A, Piga A, Bejaoui M, Perrotta S, Agaoglu L, Aydinok Y, Kattamis A, Kilinc Y, Porter J, Capra M, Galanello R, Fattoum S, Drelichman G, Magnano C, Verissimo M, Athanassiou-Metaxa M, Giardina P, Kourakli-Symeonidis A, Janka-Schaub G, Coates T, Vermylen C, Olivieri N, Thuret I, Opitz H, Ressayre-Djaffer C, Marks P, Alberti D. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator in patients with beta-thalassemia. Blood. 2006. 107:3455–3462.
22. Kwiatkowski JL. Oral iron chelators. Hematol Oncol Clin N Am. 2010. 24:229–248.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download