Abstract
The Korean national health security system covers the entire population and all medical facilities. We aimed to estimate epilepsy prevalence, anticonvulsant utilization pattern and the cost. We identified prevalent epilepsy patients by the prescription of anticonvulsants under the diagnostic codes suggesting seizure or epilepsy from 2007 Korean National Health Insurance databases. The information of demography, residential area, the kind of medical security service reflecting economic status, anticonvulsants, and the costs was extracted. The overall prevalence of treated epilepsy patients was 2.41/1,000, and higher for men than women. The age-specific prevalence was the lowest in those in their thirties and forties. Epilepsy was more prevalent among lower-income individuals receiving medical aid. The regional prevalence was the highest in Jeju Island and lowest in Ulsan city. New anticonvulsants were more frequently used than old anticonvulsants in the younger age group. The total annual cost of epilepsy or seizure reached 0.46% of total medical expenditure and 0.27% of total expenditure on health. This is the first nationwide epidemiological report issued on epilepsy in Korea. Epilepsy prevalence in Korea is comparable to those in developed countries. Economic status and geography affect the prevalence of epilepsy.
The prevalence of epilepsy has been reported to be 2.2-41.0/1,000 in diverse populations and to be affected by ethnicity and socioeconomic status (1). In Korea, no epidemiological data for epilepsy exist despite the presence of all state-of-the-art medical technologies required for the diagnosis and treatment of epilepsy, such as high resolution neuroimaging studies, the newest anticonvulsants, and various neurostimulation methods, are available.
Korea has a unique health security system, which is run by the government and based on a health insurance scheme that encompasses the entire population and all medical facilities. The scheme covers medical expenses approved for the control of most diseases, which include epilepsy, and Korean Health Insurance database contains details of all medications, medical services, and diagnoses for claims made.
Accordingly, the Korean National Health Insurance (NHI) database provides a useful and reliable source of epidemiologic data, and allows nationwide studies in unselected populations. A number of recent epidemiological reports based on NHI data have been issued on stroke (2), multiple sclerosis (3), psychiatric illness (4), hip fracture (5), asthma (6), and appendicitis (7) in Korea. National registration or health insurance databases have also been used for the epidemiologic study of epilepsy in the UK (8), Finland (9), Denmark (10), and in the US (11).
The aim of the study was to esimate the prevalence of treated epilepsy in Korea, and document anticonvulsant prescribing patterns and medical costs. This study represents the first phase of an epidemiology project initiated by the Korean Epilepsy Society.
Korea occupies the southern Korean peninsula in East Asia, and its population is almost completely composed of ethnic Koreans. In the present study, we used the 2007 databases of the Korean National Health Insurance Cooperation (NHIC) and the Health Insurance Review and Assessment Service (HIRA); both are governmental agencies that supervise all medical services in Korea.
The Korean health security system is based on an obligatory national health insurance scheme. Medical aid is provided through a social welfare fund for 3.73% (12) of the population unable to pay the insurance premium. All other citizens are obliged to join the national health insurance scheme. In 2007, the number of beneficiaries was 49,672,388 which closely approximates the total population based on 2005 census figures (47,041,434) and the population estimated for 2007 using the cohort component method (48,456,369) (13). A total of 1,943 hospitals, 26,141 private clinics, 3,445 public health centers, and 20,730 pharmacies were registered (12). Medical facilities claim costs from the NHIC, then HIRA assesses the claims based on diagnostic codes and medical records. All medical costs associated with epilepsy treatment, including laboratory examinations, medications, surgery, and hospitalization, are covered by the health security system and all related records are stored in the NHIC and HIRA databases.
Patients were considered to have epilepsy when both of the following criteria were fulfilled; 1) a diagnostic code for epilepsy or seizure, and 2) the prescription of anticonvulsants during 2007.
The diagnostic codes of the 10th version of the International Classification of Diseases and Related Health Problems (ICD-10) for epilepsy or seizure, namely, G40* (epilepsy), G41* (status epilepticus), F803 (Landau-Kleffner syndrome), and R56 (convulsion), were included in present study.
Anticonvulsants included carbamazepine, ethosuximide, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, phenobarbital, phenytoin, pregabalin, topiramate, vigabatrin, valproate, and zonisamide. Clonazepam was excluded because it is rarely used as monotherapy for epilepsy and is more frequently used for nonepileptic purposes. Other anticonvulsants including clobazam, primidone, felbamate, and tiagabine were not available in Korea in 2007. Anticonvulsants were divided into two groups; old-generation anticonvulsants, such as, carbamazepine, ethosuximide, phenobarbital, phenytoin, and valproate, and new-generation anticonvulsants, such as, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, topiramate, vigabatrin, and zonisamide.
The number of total health security system beneficiaries (49,672,388 persons) was used as the denominator for estimating prevalence. We estimated the one-year prevalence according to each age group in a 10-yr interval, by gender, economic status, and residential area. Economic status was classified according to the type of health security system received. Medical aid covered lower-income patients, and health insurance covered the remaining patients.
Korea comprises nine provinces and seven metropolitan cities. Provinces are composed of small cities and rural areas. Metropolitan cities are homogeneous urban areas that have a population of more than one million. Prevalence for each region was based on the diagnostic codes, irrespective of anticonvulsant prescription, because merging data for the residential areas and for the anticonvulsants was not permitted by privacy policy. Regional prevalence was age adjusted for the 2007 overall Korean population.
We assessed the annual medical costs incurred under the diagnosis of epilepsy or seizure for 2007 from data from health insurance reimbursements to hospitals, clinics, or pharmacies. Medical costs were relevant to direct medical costs, including the costs for outpatient clinics or hospital stays, laboratory tests, and drugs which were consumed due to epilepsy or seizure. We compared the costs with those of other developed countries. We selected comparable national studies which estimated the costs of general epilepsy, neither restricted to refractory epilepsy nor to specific institutions. We assessed the direct cost, in the form of total cost on epilepsy, the proportion of national expenditure on health, cost per patient, and the proportion of GDP per capita. For comparison, estimates from different countries were converted into US dollars using purchasing power parities (PPP) of survey year. National expenditure on health, GDP per capita and PPP were obtained from OECD health data, published in 2009 (14).
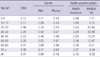
During 2007, 119,722 patients (2.41/1,000) were found to have received anticonvulsants under the diagnostic codes of seizure or epilepsy. Gender-specific prevalence was higher in men (2.66/1,000) than in women (2.16/1,000) in all age groups. Its prevalence was the lowest in those in their 30s and 40s, and increased from the 50s age group in men, whereas the prevalence was nearly constant from the 40s age group in women (Table 1).
The prevalence of epilepsy was higher among those with a lower economic status in all age groups. The patients receiving medical aid were 16,713 (14.0%) in the patients registered with epilepsy, in contrast to 3.73% in the overall population. The prevalence was 9.02/1,000 for those receiving medical aid, and 2.15/1,000 for those with health insurance. Even among those aged less than 20 yr, for whom health care is determined by their parents' economic and employment statuses, the prevalence of epilepsy was higher for those receiving medical aid (6.84/1,000 vs 2.80/1,000) (Table 1).
Age-standardized regional prevalence for diagnostic codes representing epilepsy or seizure was the highest in Jeju (7.41/1,000) and the lowest in Ulsan (4.02/1,000). Jeonnam, Jeonbuk, Gangwon, Chungnam, Gwangju, and Chungbuk followed Jeju in order of prevalence (Fig. 1). The prevalence was higher in provinces (5.04/1,000) than in metropolitan cities (4.55/1,000).
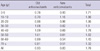
The mean number of AEDs prescribed per patient during 2007 was 1.76. New anticonvulsants were more frequently used in patients aged less than 20 yr (Table 2). In order of decreasing frequency, valproate, carbamazepine, and topiramate were the most commonly prescribed medications in all patients. In women, valproate was less frequently prescribed and topiramate and lamotrigine were more frequently prescribed (Fig. 2A). Valproate was prescribed most frequently those younger than 30 yr and older than 70 yr, whereas carbamazepine was prescribed most frequently prescribed in the other age groups (Fig. 2B).
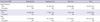
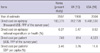
Total annual medical cost in 2007 was US$183,376,382 (adjusted to 2007 purchasing power parities), which equated to 0.46% of the total medical expenditure covered by the health security system (12) and 0.27% of total health expenditure (12, 14). The average annual cost per individual was US$759. Costs were higher for patients receiving medical aid than for those with health insurance, particularly hospitalization costs (Table 3). The cost on epilepsy or seizure as a percentage of national expenditure on health or GDP was lower than those of the UK (15) and the US (16), and the results are summarized in Table 4.
The prevalence of epilepsy found in the Korean population in the present study is comparable to those of population-based contemporary studies performed in developed countries. Record-based studies (2.7-17.6/1,000) generally estimate a prevalence lower than a door-to-door survey (2.2-41.0/1,000) (1). Our criteria for defining the epilepsy patient as a person who was prescribed anticonvulsant under a diagnosis suggestive of seizure or epilepsy are the most reasonable criteria for selecting epilepsy patients from the administrative database. We included R56 (convulsion) because many clinicians use this code even for longstanding epilepsy because of stigma. Fisher et al. (17) on behalf of International League Against Epilepsy (ILAE) and International Bureau for Epilepsy (IBE) proposed the definition of epilepsy as at least single seizure with predisposition to generate epileptic seizures. Even if the patient with diagnostic code of R56 had a single seizure, the prescription of anticonvulsant can be interpreted that clinicians judged that the patient was predisposed to have further epileptic seizure, although acute symptomatic seizures which needed short term anticonvulsants cannot be excluded.
However, this statistics can miss the patients who are not reimbursed from NHI. The patients with posttraumatic epilepsy which are reimbursed from automobile insurance, industrial accident compensation insurance or the Ministry of Patriots and Veterans Affairs, those who take anticonvulsants from volunteer organization such as Rose club, and those who chose to use alternative medicine are the cases. In addition, the prevalence measured in this study is for the treated epilepsy. For the prevalence of entire epilepsy, the treatment gap should be obtained. Overall, the prevalence in this study could be underestimated, but the margin of difference is likely to be small, because medical facilities are readily accessible and 70%-100% of anticonvulsant costs are covered by the health security system.
Men predominated in all age groups in the present study. The effect of concealment by women may be minimal, because this study was not based on self-reports but on medical records. This higher prevalence in men has also been found in the majority of European and North American studies (1), and has been reported in India (18) and Vietnam (19). On the other hand, a female predominance has been reported by many African and South American studies (1, 20).
In the present study, the prevalence of epilepsy was lowest in those in their thirties and forties. The pattern of age-specific prevalence may be because childhood epilepsies are prevalent at younger ages and various brain injuries accompanying epilepsy increase in older age. Furthermore, prevalence increased in men from age 50 yr, whereas it remained nearly constant in women. The similar pattern was shown in a Finland study (21). A greater male dominance after the age of 50 may be due to a greater exposure to brain injury. The prevalence of epilepsy due to organic cause was higher in men than women, whereas the prevalence of epilepsy due to unknown cause seems to be of the same in both genders (21, 22).
Epilepsy was more prevalent in those with a low economic status. For working-age people, a low economic status may be the result of epilepsy, which can deprive individuals of employment opportunities. However, the higher prevalence in low economic status, even in people younger than 20 who were economically inactive, suggests that low economic status increases the risk of epilepsy. This is consistent with the results of an incidence study performed in UK (23). However, an Icelandic study showed that socioeconomic status was a risk factor for adults but not for children (24). A low economic status could affect the development of epilepsy due to perinatal problems, poor nutrition and hygiene, infection, trauma, or genetic factors.
Regional differences in prevalence can be attributed to geographic and economic factors. The region with the highest prevalence was Jeju. Jeju is the largest island located 59 km from the mainland and is unique in terms of its gene pool, environment and culture. In addition, it is a representative endemic area of cysticercosis (25), which has been attributed to the local method of breeding pigs. In the southwestern region of the mainland, prevalence reduced with distance from Jeju. Gangwon, one of the regions with high prevalence, is also isolated and a relatively underdeveloped area because it is mountainous. The area with the lowest prevalence, Ulsan, is the richest area in Korea (26). Among the areas with low prevalence, the northwestern area is the capital region, and the southeastern area also developed earlier and is separated from the southwestern area by the Sobaek Mountains. The higher prevalence of epilepsy in provinces than in metropolitan cities can be similarly interpreted. It is uncertain whether economic factors have been a cause or a confounding factor, because disabled persons tend to stay in rural areas, whereas healthy persons tend to move to urban areas. Prevalence for each region could be overestimated because it was based on the diagnostic codes, irrespective of anticonvulsant prescription.
The prescribing pattern was generally reasonable considering the profiles of anticonvulsant characteristics. Valproate is not readily recommended for women of reproductive age because of teratogenic and hormonal adverse effects, whereas lamotrigine has been reported to have little effect on reproduction, at dose of less than 200 mg (27, 28). Topiramate could be more preferred by women because of its weight-reducing effect (29). The more frequent use of valproate among younger age groups is probably explained by their higher proportion of generalized epilepsy. The use of new anticonvulsants was much higher than that of old anticonvulsants in younger age groups. The use of new anticonvulsants was also quite prevalent among older age groups, considering that many patients had been taking anticonvulsants before the introduction of new anticonvulsants.
The cost that we calculated is relevant to direct medical costs. It did not include the costs for nonmedical items and unemployment, which range between 12% and 85% of total annual costs (30). Therefore, the economic burden of epilepsy would be higher than the above results.
The higher cost for patients who receive medical aid suggests that there may be a higher prevalence of more severe cases or possible overuse of medical services by individuals in this group. The direct costs on epilepsy were lower than those of the UK (15) and the US (16), although there are some differences in the inclusion criteria for the costings.
There is a potential bias and limitation in present study. The diagnostic codes can be missed, uncertain or manipulated for reimbursement. However, we believe that the level of false registration was negligible because of stigma following registration and no reimbursement in case of missing registration. The accuracy of the case ascertainment method with anticonvulsant prescription and diagnostic codes from NHI data should be validated in further studies. In spite of several limitations, this study is meaningful because it is the first epidemiologic study to be conducted on epilepsy in Korea, and one of few nationwide studies on an unselected population.
In conclusion, epilepsy prevalence in Korea is comparable to that in developed countries. Economic status and geography affect the prevalence of epilepsy.
Figures and Tables
Fig. 1
Regional prevalence in Korea. Note that the prevalence for each region was based on the diagnostic codes, irrespective of anticonvulsant prescription, because merging data for the residential areas and for the anticonvulsants was not permitted by privacy policy. Darker shades indicate higher prevalence. Numbers are the age-standardized prevalences per 1,000 of the population in each region.

Fig. 2
Anticonvulsant prescribing pattern according to gender (A) and age (B). (A) The vertical axis indicates the frequency of prescription (the number of patients who were prescribed the anticonvulsant divided by the number of entire patients who were prescribed any anticonvulsants under the diagnosis of epilepsy or seizure). (B) The length of horizontal axis was proportionated with the number of patients who took the anticonvulsant. The anticonvulsants were arranged in order of decreasing use from left to right. VPA, valproate; CBZ, carbamazepine; TPM, topiramate; LMT, lamotrigine; OCZ, oxcarbazepine; DPH, phenytoin; Pb, phenobarbital; GBP, gabapentin; ZNS, zonisamide; LVT= levetiracetam; VGB, vigabatrin; PGB, pregabalin; ETX, ethosuximide.

ACKNOWLEDGMENTS
We wish to acknowledge assistance received from Kun-Sei Lee, Director of Research and Development Center, Health Insurance Review of Assessment Service, and Mi-Kyeong Cho, Statistics Department, National Health Insurance Cooperation, Korea.
References
1. Banerjee PN, Filippi D, Allen Hauser W. The descriptive epidemiology of epilepsy: a review. Epilepsy Res. 2009. 85:31–45.
2. Lim SJ, Kim HJ, Nam CM, Chang HS, Jang YH, Kim S, Kang HY. Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database. J Prev Med Public Health. 2009. 42:251–260.
3. Kim NH, Kim HJ, Cheong HK, Kim BJ, Lee KH, Kim EH, Kim EA, Kim S, Park MS, Yoon WT. Korean Multiple Sclerosis Study Group. Prevalence of multiple sclerosis in Korea. Neurology. 2010. 75:1432–1438.
4. Chung W, Oh SM, Suh T, Lee YM, Oh BH, Yoon CW. Determinants of length of stay for psychiatric inpatients: analysis of a national database covering the entire Korean elderly population. Health Policy. 2010. 94:120–128.
5. Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, Park SE. Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health. 2010. 10:230.
6. Park CS, Kang HY, Kwon I, Kang DR, Jung HY. Cost-of-illness study of asthma in Korea: estimated from the Korea National Health insurance claims database. J Prev Med Public Health. 2006. 39:397–403.
7. Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010. 20:97–105.
8. Wallace H, Shorvon S, Tallis R. Age-specific incidence and prevalence rates of treated epilepsy in an unselected population of 2,052,922 and age-specific fertility rates of women with epilepsy. Lancet. 1998. 352:1970–1973.
9. Sillanpää M, Kälviäinen R, Klaukka T, Helenius H, Shinnar S. Temporal changes in the incidence of epilepsy in Finland: nationwide study. Epilepsy Res. 2006. 71:206–215.
10. Christensen J, Vestergaard M, Pedersen MG, Pedersen CB, Olsen J, Sidenius P. Incidence and prevalence of epilepsy in Denmark. Epilepsy Res. 2007. 76:60–65.
11. Kurth T, Lewis BE, Walker AM. Health care resource utilization in patients with active epilepsy. Epilepsia. 2010. 51:874–882.
12. Korean National Health Insurance Cooperation. Annual report of national health insurance statistics, 2007. 2007. Seoul: Division of statistical analysis, Korean National Health Insurance Cooperation.
13. Statistics Korea. Population trends. 2007. Office for Social Statistics, Statistics Korea.
14. OECD. OECD Health Data 2009. 2009. Paris: OECD.
15. Cockerell OC, Hart YM, Sander JW, Shorvon SD. The cost of epilepsy in the United Kingdom: an estimation based on the results of two population-based studies. Epilepsy Res. 1994. 18:249–260.
16. Yoon D, Frick KD, Carr DA, Austin JK. Economic impact of epilepsy in the United States. Epilepsia. 2009. 50:2186–2191.
17. Fisher RS, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, Engel J Jr. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005. 46:470–472.
18. Sridharan R, Murthy BN. Prevalence and pattern of epilepsy in India. Epilepsia. 1999. 40:631–636.
19. Tuan NA, Cuong le Q, Allebeck P, Chuc NT, Persson HE, Tomson T. The prevalence of epilepsy in a rural district of Vietnam: a population-based study from the EPIBAVI project. Epilepsia. 2008. 49:1634–1637.
20. Forsgren L, Beghi E, Oun A, Sillanpää M. The epidemiology of epilepsy in Europe: a systematic review. Eur J Neurol. 2005. 12:245–253.
21. Keränen T, Riekkinen PJ, Sillanpää M. Incidence and prevalence of epilepsy in adults in eastern Finland. Epilepsia. 1989. 30:413–421.
22. Haerer AF, Anderson DW, Schoenberg BS. Prevalence and clinical features of epilepsy in a biracial United States population. Epilepsia. 1986. 27:66–75.
23. Heaney DC, MacDonald BK, Everitt A, Stevenson S, Leonardi GS, Wilkinson P, Sander JW. Socioeconomic variation in incidence of epilepsy: prospective community based study in south east England. BMJ. 2002. 325:1013–1016.
24. Hesdorffer DC, Tian H, Anand K, Hauser WA, Ludvigsson P, Olafsson E, Kjartansson O. Socioeconomic status is a risk factor for epilepsy in Icelandic adults but not in children. Epilepsia. 2005. 46:1297–1303.
25. Kong Y, Cho SY, Cho MS, Kwon OS, Kang WS. Seroepidemiological observation of Taenia solium cysticercosis in epileptic patients in Korea. J Korean Med Sci. 1993. 8:145–152.
26. Statistics Korea. Local income. 2007. Office for Economic Statistics, Statistics Korea.
27. Harden CL, Meador KJ, Pennell PB, Hauser WA, Gronseth GS, French JA, Wiebe S, Thurman D, Koppel BS, Kaplan PW, Robinson JN, Hopp J, Ting TY, Gidal B, Hovinga CA, Wilner AN, Vazquez B, Holmes L, Krumholz A, Finnell R, Hirtz D, Le Guen C. American Academy of Neurology, American Epilepsy Society. Management issues for women with epilepsy-Focus on pregnancy (an evidence-based review): II. Teratogenesis and perinatal outcomes: report of the Quality Standards Subcommittee and Therapeutics and Technology Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2009. 50:1237–1246.
28. Morrow J, Russell A, Guthrie E, Parsons L, Robertson I, Waddell R, Irwin B, McGivern RC, Morrison PJ, Craig J. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry. 2006. 77:193–198.
29. French JA, Kanner AM, Bautista J, Abou-Khalil B, Browne T, Harden CL, Theodore WH, Bazil C, Stern J, Schachter SC, Bergen D, Hirtz D, Montouris GD, Nespeca M, Gidal B, Marks WJ Jr, Turk WR, Fischer JH, Bourgeois B, Wilner A, Faught RE Jr, Sachdeo RC, Beydoun A, Glauser TA. American Academy of Neurology Therapeutics and Technology Assessment Subcommittee. American Academy of Neurology Quality Standards Subcommittee. American Epilepsy Society Quality Standards Subcommittee. American Epilepsy Society Therapeutics and Technology Assessment Subcommittee. Efficacy and tolerability of the new antiepileptic drugs. I: Treatment of new-onset epilepsy: report of the TTA and QSS Subcommittees of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2004. 45:401–409.
30. Strzelczyk A, Reese JP, Dodel R, Hamer HM. Cost of epilepsy: a systematic review. Pharmacoeconomics. 2008. 26:463–476.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download