Abstract
The purpose of this study was to investigate whether sperm selection by hyaluronic acid (HA) binding could improve fertilization rate and embryo quality in intracytoplasmic sperm injection (ICSI) cycles. Two hundred nineteen oocytes obtained from eighteen women were injected with either HA-bound (n = 107) or conventionally selected spermatozoa (n = 112) in a randomized way. All of the participants were infertile couples who had normal sperm parameters but low fertilization rate in previous in vitro fertilization (IVF) cycle (n = 5) or experienced multiple IVF failures (n = 13). Lower fertilization (75.7% vs 83.0%) and cleavage rate on day 2 (72.9% vs 83.0%) was observed in oocytes injected with HA-bound spermatozoa than the conventional group, but the difference was not significant. Significantly lower cleavage rate was observed on day 3 in HA group (56.0% vs 69.6%, P = 0.038). Blastocyst formation rate and the number of transferred embryos were similar in both groups. In multiple IVF failure patients, significantly reduced fertilization rate (71.8% vs 85.3%, P = 0.046) and cleavage rate on day 2 (70.4% vs 85.3%, P = 0.029) and day 3 (53.5% vs 77.3%, P = 0.002) were noticed in HA group. Five women achieved pregnancy continuing more than 12 weeks after transfer (27.8%). Success of ICSI was not related with the number of embryos fertilized by HA-bound spermatozoa. Application of ICSI by sperm selection using HA binding is not helpful in couples with repeated poor fertilization or implantation despite normal sperm parameters.
Although various techniques have rapidly been developed over 30 yr in the field of assisted reproduction, the success rate remains low (1, 2). About a fifth of patients is diagnosed infertility without definite causes (3). In addition, small portion of patients fails to conceive despite multiple in vitro fertilization (IVF) procedures. The causes of recurrent implantation failure (RIF) are not clear yet (1). One of the suspicious etiologies of RIF is low implantation potential of embryo and this could be attributed to incompetent spermatozoa (4). Several sperm selection methods were introduced to improve the quality of embryo (5-9). Farhi et al. (6) reported that young patients with multiple IVF failures showed relatively higher prevalence of male factor infertility characterized by low fertilization rate with intracytoplasmic sperm injection (ICSI).
Among the novel sperm selection methods, ICSI using hyaluronic acid (HA) containing media has been suggested to have higher specificity and lower biological risk than other selection methods (10). HA is a polysaccharide which consists in extracellular matrix of the cumulus oophorus, and considered to have a role in selection of mature spermatozoa. HA-binding ability of spermatozoa is related to sperm membrane maturity and fertilizing potential, thus it has been suggested that sperm selection using HA could increase the implantation rate in ICSI cycles (5, 11-13). This novel sperm selection system has been referred to a 'physiologic ICSI (PICSI)' because high proportion of spermatozoa collected in conventional method was found to be unable to bind to HA (9, 13, 14). The majority of studies have consistently reported that HA-binding method is effective in selection of spermatozoa without DNA fragmentation and with normal nucleus (5, 12, 13, 15, 16). However, there are conflicting data regarding subsequent improvement of fertilization rate and cleavage rate after ICSI using HA-bound spermatozoa (14, 17-20). Herein we investigated the effect of sperm selection using HA-containing medium in couples with normal sperm parameters.
Eighteen couples who undertaken ICSI cycles between July and December 2011 were prospectively included. All of the patients agreed to participate in this study and signed the informed consent form. This prospective trial was approved by ethical committee of the institution. The inclusion criteria were as follows; 1) age of women ranged from 30 to 42 yr, 2) serum FSH level on menstrual day 3 ≤ 20 IU/L, 3) total number of oocytes retrieved ≥ 4, and 4) total sperm number > 2.0 × 106/mL and strict morphology > 4% according to WHO criteria (2010) (19). All of the participants were free of significant uterine pathology such as huge fibroids, intrauterine adhesions or adenomyosis. The ICSI indications were previous low fertilization rate (FR) with IVF (< 20%) and/or a history of multiple IVF failures (more than 2 cycles). Only fresh ICSI cycles were included in the analyses.
Depot triptorelin (Decapeptyl® SR, 3.75 mg; Ferring, Malmo, Sweden) injection was given in the mid-luteal phase of the previous cycle in the GnRH agonist long protocol. After pituitary down-regulation, gonadotropin (Gonal-F®; Serono, Geneva, Switzerland) and menotropin (Menopur®; Ferring) was added until either the leading follicle reached a mean diameter of 18 mm or two or more follicles reached 17 mm in diameter. Initial doses of gonadotropins were ranged between 150-300 IU depending on the patient's previous or anticipated response and the dose was adjusted according to the individual's response. In the ultrashort GnRH agonist combined with flexible GnRH antagonist protocol, daily administration of triptorelin (Decapeptyl®, 0.1 mg; Ferring) was started on the first or second menstrual day and continued for 3 consecutive days. Gonadotropins were initiated on the third day of menses with individually adjusted dose. Once at least one follicle had reached a diameter of 14 mm, cetrorelix (Cetrotide®, 0.25 mg; Serono) was added as described in previous studies (21, 22). In all cases, a recombinant human chorionic gonadotropin (Ovidrel®, 250 µg; Serono) was injected subcutaneously and transvaginal oocytes retrieval was done after 34-36 hr.
Liquefied semen was placed in a 15 mL conical tube dispensed with 1.0 mL of 40% gradient stock solution underlaid by 1.0 mL of 80% gradient stock solution (PureCeption®; SAGE, Trumbull, CT, USA). After centrifugation at 1,400 rpm for 20 min, the pellet under 80% layer was collected and then washed with Quinn's sperm washing media (SAGE) by centrifugation at 1,000 rpm for 10 min. Sample tubes were incubated at 37℃ for 45-60 min to allow progressively motile sperm to swim up into the overlaid medium.
Oocytes were incubated at 37℃ under 5% CO2 after retrieval. Cumulus-oocyte complexes were placed into a droplet of hyaluronidase solution for up to 40 sec. After final denudation, only the oocytes that were at the metaphase II stage at that time were identified. Sibling oocytes were allocated to two separate collection dishes in an alternating way. A computer-generated randomization list was used for allocation of the first dish to either HA-containing medium group or conventional group. For conventional, 10 µL of spermatozoa with high motility was diluted in HEPES-buffered human tubal fluid medium (SAGE) containing 10% of SPS (Serum Protein Substitute; SAGE) placed in the middle of plastic Petri dish. Before injection, 3 µL of sperm suspension was transferred to 7 µL of 7% polyvinylpyrrolidone (PVP; SAGE) solution to remove debris and get better control. Spermatozoa with best morphology were selected for injection into a MII oocytes using inverted microscope equipped with micromanipulators.
In HA-ICSI group, a 2 µL droplet with suspension of spermatozoa was placed to a 5 µL droplet of HA-containing medium (SpermSlow®; MediCult, Jyllinge, Denmark) and incubated for 15 min at 37℃ under oil. Spermatozoa bound to HA in the junction of the two droplets were identified and carefully detached by injecting pipette (ICSI Micropipette; TPC, Thebarton, Adelaide, South Australia) and subsequently injected into a MII oocyte. All the ICSI procedures were performed in 40 hr since ovulation triggering.
Presence of 2 pronuclei of each embryo was assessed about 18 hr after ICSI. Embryos, fertilized either by HA-based or conventional method, were transferred to the uterus via transcervical approach. Before uterine transfer, embryos were graded according to their morphologies and cleavage rate for subsequent 6 days of culture. Day 3 ET was performed (8 cycles) if number of viable embryo was less than five. In case of five or more, day 5 ET was done (10 cycles). Using recent embryo assessment criteria (23), up to three embryos with good quality were selected for transfer according to the Korean nationwide guideline for IVF. Then intramuscular injection of progesterone 50 mg (Watson Laboratories Inc., Morristown, NJ 07962 USA) was applied daily for luteal phase support. Clinical pregnancy was defined by the ultrasonographic visualization of the gestational sac at 3-4 weeks after oocyte retrieval.
Chi-square test and Mann-Whitney U test were used to compare the result between HA-containing medium group and conventional group. The statistical software package SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) was used and P value less than 0.05 was considered significant.
This study was approved by the institutional review board of Institute of Hamchoon Women's Clinic (HCIRB-1106-01-001). The participants had detailed explanation from the researchers and gave their written informed consents. There were no employees of our clinic among the study subjects.
Mean age of the study population was 35.4 ± 3.9 yr and basal serum level of AMH was 3.57 ± 1.70 ng/mL. Thirteen couples had a history of implantation failure for more than two fresh IVF cycles (3.3 ± 0.9 cycles on average) and the others had low fertilization history (mean fertilization rate in a previous cycle, 10.1% ± 9.3%). There were no significant differences in regard to patient's age, level of anti-Müllerian hormone (AMH) or follicle stimulating hormone (FSH), total dose and duration of gonadotropin, endometrial thickness on ET day and total number of retrieved oocytes between the two different ICSI indication groups.
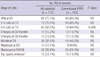
The total number of injected MII oocytes were 107 in HA group and 112 in conventional (PVP) group (Table 1). Oocytes injected with HA-bound spermatozoa had lower fertilization and cleavage rate on day 2 than the conventional group, but the differences did not reach statistical significance. However, on day 3, significantly lower cleavage rate was observed in HA group (56.0% vs 69.6%, P = 0.038). Blastocyst formation rates were similar on day 5 and day 6 between two methods. The total numbers of transferred embryos and top quality embryos, either on day 3 or 5, were not significantly different between two methods.
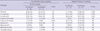
When the study population was divided by the ICSI indication, multiple IVF failure group showed significantly lower fertilization rate (71.8% vs 85.3%, P = 0.046) and embryo cleavage rate on day 2 (70.4% vs 85.3%, P = 0.029) and day 3 (53.5% vs 77.3%, P = 0.002) when HA-selected spermatozoa were used. In low fertilization history group, two selection methods showed similar fertilization, cleavage and blastocyst formation rate. Notably, all of the transferred embryos on day 5 were fertilized by HA-selected spermatozoa in low fertilization history group (13.9% vs 0%, P = 0.024) (Table 2).
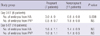
Overall ongoing pregnancy rate was 27.8% and implantation rate per embryos was 19.4% (7/36). One case was a biochemical pregnancy and two cases ended in missed abortion before 10 weeks. No significant difference in the women's age, level of basal serum FSH, endometrial thickness on ET day and presence of history of RIF between the pregnancy group and non-pregnancy group (data not shown). Cycles with achievement of clinical pregnancy showed higher number of transferred embryos from HA group at day 3. Between pregnant and non-pregnant groups, there was no significant difference in the number of transferred embryos fertilized by HA-selected spermatozoa at day 5. Either at day 3 or day 5, similar number of embryos from PVP method was observed between the two groups (Table 3).
Contrary to our expectation, selection of HA-bound spermatozoa had no benefits in terms of fertilization and subsequent embryo cleavage in ICSI cycles. Previous researches have shown inconsistent reports regarding the effect of HA-binding selection method on IVF/ICSI outcomes. Most of previous studies using HA-containing medium in ICSI cycles showed similar or improved fertilization and cleavage rate (8, 13, 14, 24). Because those studies included patients with abnormal sperm parameters, it is postulated that the gamete selection using HA-binding might be advantageous. Castillo-Baso et al. (17) have reported that embryos fertilized with HA-bound sperm showed improved quality only when strict morphology was less than 4%; the benefit was not maintained when that was more than 4%. This finding suggests that HA-binding method would be beneficial only in male factor infertility. The reasons for lower cleavage rate on day 3 in the present study are unclear. Previous report indicated that possible iatrogenic damage to spermatozoa might be caused by additional exposure to nonphysiologic conditions during HA-binding assay (10). Interestingly, in the present study, conventional method did not yield any blastocyst in previous low fertilization group; this suggests that HA-binding method could be helpful in cases of poor fertilization history, but further study will be needed to confirm this finding.
Regarding pregnancy outcomes, a recent study showed improved outcomes in patients with PICSI using commercial HBA® and PICSI® assays kit (Biocoat, Inc., Horsham, PA 19044 USA) (18). It was suggested that selection of sperm with better developmental and nuclear competence influences on preimplantation embryogenesis. Because we used both HA-binding and conventional method in sibling oocytes, it was not possible to evaluate the effect of HA-binding method on pregnancy outcome. In this study, the overall ongoing pregnancy rate was relatively lower (27.8%) and the pregnancy loss rate (28.6%) was higher than those in previous studies (18, 25). This could be partly due to the fact that the mean age of the study population was more than 35 yr which is associated with increased risk of implantation failure and miscarriage (26).
It has been reported that HA-selected spermatozoa show lower levels of numerical chromosomal aberrations than those of initial semen (16). In addition, considering individual-to-individual differences in Tygerberg sperm morphology scoring probably due to the various perceptions of shape normality (15), concurrent HA-binding result may minimize this inter-individual variability in sperm evaluation (9). Furthermore, sperm selection via HA-binding is an easily available method and does not require expensive instrumentation among the advanced sperm selection techniques (10). However, our data suggest that there is no value of HA-binding medium in patients with normal sperm parameters. Moreover, HA-binding method could cause even lower fertilization and cleavage rate than conventional method in multiple implantation failure patients. Further prospective studies to confirm the efficacy of HA-binding method are in need.
Figures and Tables
References
1. Ola B, Li TC. Implantation failure following in-vitro fertilization. Curr Opin Obstet Gynecol. 2006. 18:440–445.
2. Wright VC, Chang J, Jeng G, Macaluso M. Centers for Disease Control and Prevention (CDC). Assisted reproductive technology surveillance--United States, 2005. MMWR Surveill Summ. 2008. 57:1–23.
3. Kovacs P, Kovats T, Sajgo A, Szollosi J, Matyas S, Kaali SG. The role of hyaluronic acid binding assay in choosing the fertilization method for patients undergoing IVF for unexplained infertility. J Assist Reprod Genet. 2010. 28:49–54.
4. Sharif KW, Ghunaim S. Management of 273 cases of recurrent implantation failure: results of a combined evidence-based protocol. Reprod Biomed Online. 2010. 21:373–380.
5. Nijs M, Creemers E, Cox A, Janssen M, Vanheusden E, Van der Elst J, Ombelet W. Relationship between hyaluronic acid binding assay and outcome in art: a pilot study. Andrologia. 2010. 42:291–296.
6. Farhi J, Ben-Haroush A, Dresler H, Pinkas H, Sapir O, Fisch B. Male factor infertility, low fertilisation rate following ICSI and low number of high-quality embryos are associated with high order recurrent implantation failure in young IVF patients. Acta Obstet Gynecol Scand. 2008. 87:76–80.
7. Morrell JM, Rodriguez-Martinez H. Practical applications of sperm selection techniques as a tool for improving reproductive efficiency. Vet Med Int. 2011. doi: 10.4061/2011/894767.
8. Nasr-Esfahani MH, Razavi S, Vahdati AA, Fathi F, Tavalaee M. Evaluation of sperm selection procedure based on hyaluronic acid binding ability on ICSI outcome. J Assist Reprod Genet. 2008. 25:197–203.
9. Ebner T, Filicori M, Tews G, Parmegiani L. A plea for a more physiological ICSI. Andrologia. 2012. 44:2–19.
10. Said TM, Land JA. Effects of advanced selection methods on sperm quality and art outcome: a systematic review. Hum Reprod Update. 2011. 17:719–733.
11. Cayli S, Jakab A, Ovari L, Delpiano E, Celik-Ozenci C, Sakkas D, Ward D, Huszar G. Biochemical markers of sperm function: male fertility and sperm selection for ICSI. Reprod Biomed Online. 2003. 7:462–468.
12. Huszar G, Ozkavukcu S, Jakab A, Celik-Ozenci C, Sati GL, Cayli S. Hyaluronic acid binding ability of human sperm reflects cellular maturity and fertilizing potential: selection of sperm for intracytoplasmic sperm injection. Curr Opin Obstet Gynecol. 2006. 18:260–267.
13. Parmegiani L, Cognigni GE, Bernardi S, Troilo E, Ciampaglia W, Filicori M. "Physiologic ICSI": hyaluronic acid (HA) favors selection of spermatozoa without DNA fragmentation and with normal nucleus, resulting in improvement of embryo quality. Fertil Steril. 2010. 93:598–604.
14. Menezo Y, Junca AM, Dumont M, De Mouzon J, Cohen-Bacrie P, Ben Khalifa M. "Physiologic" (hyaluronic acid-carried) ICSI results in the same embryo quality and pregnancy rates as with the use of potentially toxic polyvinylpyrrolidone (PVP). Fertil Steril. 2010. 94:S232.
15. Prinosilova P, Kruger T, Sati L, Ozkavukcu S, Vigue L, Kovanci E, Huszar G. Selectivity of hyaluronic acid binding for spermatozoa with normal Tygerberg strict morphology. Reprod Biomed Online. 2009. 18:177–183.
16. Jakab A, Sakkas D, Delpiano E, Cayli S, Kovanci E, Ward D, Ravelli A, Huszar G. Intracytoplasmic sperm injection: a novel selection method for sperm with normal frequency of chromosomal aneuploidies. Fertil Steril. 2005. 84:1665–1673.
17. Castillo-Baso J, Garcia-Villafaña G, Santos-Haliscak R, Diaz P, Sepluveda-Gonzalez J, Hernandez-Ayup S. Embryo quality and reproductive outcomes of spermatozoa selected by physiologic-icsi or conventional icsi in patients with kruger <4% and >4% normo-morphology. Fertil Steril. 2011. 96:S159.
18. Worrilow KC, Eid S, Woodhouse D, Witmyer J, Khoury C, Liebermann J. Increased clinical pregnancy rates (CPR) and statistically significant decrease in loss rates using hyaluronan in sperm selection: prospective, multi-center, double-blind, randomized clinical trial. Fertil Steril. 2011. 96:S179.
19. WHO. WHO laboratory manual for the examination and processing of human semen. 2010. 5th ed. Geneva: World Health Organization.
20. Lee K, Hyslop JM, Nanassy L, Machaty Z. Incidence of apoptosis in parthenogenetic porcine embryos generated by using protein kinase or protein synthesis inhibitors. Anim Reprod Sci. 2009. 112:261–272.
21. Orvieto R, Kruchkovich J, Rabinson J, Zohav E, Anteby EY, Meltcer S. Ultrashort gonadotropin-releasing hormone agonist combined with flexible multidose gonadotropin-releasing hormone antagonist for poor responders in in vitro fertilization/embryo transfer programs. Fertil Steril. 2008. 90:228–230.
22. Orvieto R, Nahum R, Rabinson J, Gemer O, Anteby EY, Meltcer S. Ultrashort flare GnRH agonist combined with flexible multidose GnRH antagonist for patients with repeated IVF failures and poor embryo quality. Fertil Steril. 2009. 91:1398–1400.
23. Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011. 26:1270–1283.
24. Van Den Bergh MJ, Fahy-Deshe M, Hohl MK. Pronuclear zygote score following intracytoplasmic injection of hyaluronan-bound spermatozoa: a prospective randomized study. Reprod Biomed Online. 2009. 19:796–801.
25. Parmegiani L, Cognigni GE, Ciampaglia W, Pocognoli P, Marchi F, Filicori M. Efficiency of hyaluronic acid (HA) sperm selection. J Assist Reprod Genet. 2010. 27:13–16.
26. Kroon B, Harrison K, Martin N, Wong B, Yazdani A. Miscarriage karyotype and its relationship with maternal body mass index, age, and mode of conception. Fertil Steril. 2011. 95:1827–1829.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download