Abstract
This was designed to assess the outcomes of side branch (SB) stenosis after implantation of three drug-eluting stents (DES). From 2,645 patients in the ZEST (Comparison of the Efficacy and Safety of Zotarolimus-Eluting Stent with Sirolimus-Eluting and PacliTaxel-Eluting Stent for Coronary Lesions) Trial, 788 patients had 923 bifurcation lesions with SB ≥ 1.5 mm were included. SB was treated in 150 lesions, including 35 (3.8%) receiving SB stenting. Of untreated SB with baseline stenosis < 50%, the incidences of periprocedural SB compromise was similar in the zotarolimus (15.8%), sirolimus (17.2%), and paclitaxel (16.6%) stent groups (P = 0.92). At follow-up angiography, delayed SB compromise occurred in 13.9%, 3.2%, and 9.4% (P = 0.010) of these groups. When classified into four groups (< 50%, 50%-70%, 70%-99%, and 100%), 9.0% of untreated SB were worsened, whereas improvement and stationary were observed in 9.6% and 81.4%. In a multivariable logistic regression model, main branch (MB) stenosis at follow-up (%) was the only independent predictor of SB stenosis worsening (odds ratio, 1.03; 95% confidence interval, 1.01-1.04; P < 0.001). After MB stenting in bifurcation lesions, a minority of SB appears to worsen. DES with strong anti-restenotic efficacy may help maintain SB patency.
Although the use of drug-eluting stent (DES) has improved the outcomes of percutaneous coronary intervention (PCI), procedures for treatment of bifurcation lesions remain challenging because of their technical complexity and unpredictable complications (1, 2). In particular, no optimal procedure for side branch (SB) treatment, using either balloon angioplasty or stenting, nor the timing thereof, has been determined. This issue is more clinically relevant when the bifurcation lesion is treated with a single-stent technique, in which stenting is performed for the main branch (MB) alone, leaving the SB untouched. For example, the benefits of kissing balloon angioplasty, which is frequently applied in the single-stent technique, have not been completely evaluated (10, 11). Indeed, the long-term outcomes of SB stenosis are unclear because the natural course of SB after MB stenting has not been determined. Although studies using DES or bare-metal stent (BMS) have suggested spontaneous improvement of SB flow, the reports on the initial and follow-up angiographic outcomes of SB stenosis after DES implantation are still limited (12-14). Therefore, the present study was designed to assess the frequency and outcomes of SB stenosis after implantation of three DESs, randomly evaluated in the Comparison of the Efficacy and Safety of Zotarolimus-Eluting Stent with Sirolimus-Eluting and PacliTaxel-Eluting Stent for Coronary Lesions (ZEST) trial (15).
This study was a bifurcation substudy, which had been prespecified in the protocol of the ZEST trial. The ZEST trial was a prospective, randomized, single-blind, multicenter study comparing the safety and effectiveness of zotarolimus-eluting stents (ZES, Endeavor; Medtronic Vascular, Minneapolis, MN, USA), sirolimus-eluting stents (SES, Cypher select; Cordis, Johnson & Johnson, Bridgewater, NJ, USA), and paclitaxel-eluting stents (PES, Taxus Liberte; Boston Scientific, Natick, MA, USA) in patients randomized 1:1:1 (15). The study enrolled 'all comers' undergoing PCI except those with acute ST-segment elevation myocardial infarction necessitating primary PCI, severe left ventricular dysfunction with ejection fraction < 35%, cardiogenic shock, left main stenosis, in-stent restenosis of DES, or inability to receive antiplatelet treatment. This bifurcation substudy retrospectively included patients enrolled in the ZEST trial who had bifurcation coronary lesions with SB ≥ 1.5 mm in diameter within the stented segment of the MB.
All procedures were performed using standard techniques for PCI. As our protocol did not specify the methods to be used to treat bifurcation lesions, the choice of predilation, kissing balloon inflation, or stenting in SB was at the discretion of each physician. All lesions in MB and SB were recommended to be treated with the assigned DES type. Antithrombotic therapy consisted of standard dual antiplatelet therapy with 100 mg/day aspirin and 75 mg/day clopidogrel for at least 12 months after stenting.
Patients were followed-up at 30 days and 4, 9, and 12 months. All patients were asked to receive angiographic follow-up 8 to 10 months after the procedure, or earlier if anginal symptoms occurred. Patient demographic, clinical, angiographic, procedural, and outcome characteristics were collected using dedicated electronic case report forms. All events, including death, myocardial infarction, and repeat revascularization, were centrally adjudicated by an independent clinical event committee based on the source documents collected at each hospital.
Baseline, post-procedure, and follow-up angiograms were analyzed using an automated edge-detection analysis system (CAAS-5, Pie Medical Imaging, Maastricht, the Netherlands) in an angiographic core laboratory of the CardioVascular Research Foundation (16, 17). Quantitative angiographic analysis of the MB was performed within the stented segment (in-stent) and over the entire segment, including the stent and margins 5 mm proximal and distal thereto (in-segment) (16). Measured variables included the reference diameter, minimal lumen diameter, percentage diameter stenosis, and late luminal loss. The reference diameter was determined by interpolation. Binary restenosis was defined as ≥ 50% percent stenosis on follow-up angiography. In SB analysis, all angiographic measurements were made by visual estimation. The degree of diameter stenosis was classified as < 50%, 50%-70%, 70%-99%, and 100%, and vessel size was classified as < 1.5 mm, 1.5-2.0 mm, 2.0-2.5 mm, 2.5-3.0 mm, and ≥ 3.0 mm. Visually estimated bifurcation classifications were made according to the MEDINA classification (18). SB compromise after a procedure (periprocedural) and at follow-up (delayed) was defined as ≥ 50% diameter stenosis at the ostial SB. Spontaneous recanalization was defined as the SB which had post-procedural flow of TIMI grade 0 but ≥ TIMI grade 1 at follow-up.
The primary endpoint of this study was SB diameter stenosis at follow-up angiography. All other angiographic parameters were considered to be secondary endpoints. Deaths were considered to be of cardiac origin unless a noncardiac cause could be identified. Myocardial infarction was diagnosed based on the presence of new Q waves in at least two contiguous leads on an electrocardiogram or an elevation of creatine kinase or its MB isoenzyme to at least three times the upper limit of the normal range in at least two blood samples. Target lesion revascularization was defined as any revascularization with either PCI or bypass surgery in the targeted segments and the adjacent 5 mm. Stent thrombosis was defined as definite or probable according to the Academic Research Consortium definition (19).
Data for continuous and categorical variables are presented as means ± standard deviations and numbers (with percentages), respectively. Differences among treatment groups were evaluated by one-way ANOVA for continuous variables and by the chi-square or Fisher's exact test for categorical variables, with the Bonferroni correction used for post-hoc comparisons. The variables were further compared using the Kruskal-Wallis test when they were not normally distributed by the Kolmogorov-Smirnov test. All analyses were based on the intention-to-treat principle.
Angiographic outcomes in SBs were estimated in the two cohorts, consisting of all SBs with or without treatment and naive SBs without any treatment during the principal procedure. In the naive SB group, independent predictors of worsening of SB stenosis were estimated using a multivariable logistic generalized estimated equation model with robust standard errors that accounted for the clustering between lesions in the same subject. The model for the outcome variable was reduced by using backward elimination until the model contained only factors with P values < 0.1. Because of the limited number of events, the model used 15 covariates: age; gender; symptom presentation; diabetes mellitus; chronic renal failure; hypercholesterolemia; MB stent length; MB stenosis at baseline, post-procedure and follow-up; MB in-stent late loss; SB size group; and SB stenosis group at baseline and post-procedure. All P values were two-sided, and P values less than 0.05 were considered statistically significant. SAS software, version 9.1 (SAS Institute, Cary, NC, USA) was used for statistical analysis.
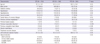
Of the 2,645 patients with 3,613 lesions enrolled in the ZEST trial, 788 (29.8%) patients having 923 (25.5%) bifurcation lesions with SB ≥ 1.5 mm in diameter were included in this substudy. Table 1 shows the baseline clinical characteristics of the ZES, SES, and PES patients. All variables were well matched except for the slightly lower incidence of previous PCI or myocardial infarction in the ZES group. Baseline characteristics of 3 DES groups were also well matched in patients with angiography follow-up except in the ZES group in the same manner.
Lesion and procedural characteristics are shown in Table 2. In all three treatment groups, the left anterior descending artery of the MB and the diagonal branch of the SB were most frequently involved. The prevalence of total occlusion was slightly lower in the ZES group, and the numbers and lengths of stents used in the MB were comparable in the three groups. However, the maximal device diameter was slightly smaller in the ZES group. SB treatment was performed on 150 (16.3%) lesions, with a similar distribution across the three groups, whereas 35 (3.8%) lesions underwent stenting in both branches. Stents were used as the assigned randomization in all patients. Peri-procedural MI, defined as procedure-related increase of creatine kinase or its MB isoenzyme to at least three times the upper limit of the normal range, occurred in 24 (7.9%), 33 (10.2%) and 24 (8.2%) lesions after ZES, SES, and PES implantations, respectively (P = 0.53).
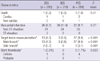
Table 3 shows the results of quantitative angiographic analysis of the MB. Follow-up angiography was obtained for 635 (68.8%) lesions, including 221 ZES (72.5%), 204 SES (63.0%), and 210 (71.4%) PES (P = 0.018) treated lesions. At baseline and immediately post-procedure, all angiographic parameters were almost identical among the three groups. However, at follow-up angiography, because of the lower late loss in the SES group, that group had a significantly higher minimal lumen diameter and a significantly smaller diameter stenosis than did the ZES or PES groups. When the differences were compared using the Kruskal-Wallis test, the statistical differences were not changed in any variable. As a result, the restenosis rate was significantly lower in the SES than in the ZES or PES groups. Angiographic outcomes at follow-up were, however, similar between the ZES and PES groups.
Table 4 shows angiographic analysis data of all SBs. True bifurcation lesions involving both branches, defined as MEDINA classes 1.1.1., 1.0.1., and 0.1.1., were observed in 27.9% of the ZES, 29.0% of the SES, and 31.0% of the PES (P = 0.70) lesions. SB vessel size was averaged between 2.0 and 2.5 mm. After the procedure, periprocedural SB compromise, defined as ≥ 50% diameter stenosis, occurred in 21.0% of the ZES, 22.8% of the SES, and 23.8% of the PES (P = 0.70) lesions. At follow-up angiography, the mean value of diameter stenosis was lower in the SES than in the ZES and PES groups. Therefore, the prevalence of delayed SB compromise at follow-up was numerically lower in the SES (17.2%) than in the ZES (24.0%) and PES (24.3%) lesions, but the difference did not attain statistical significance (P = 0.14). However, when the diameter stenosis was compared using the Kruskal-Wallis test, the statistical significance was not significant at baseline (P = 0.61), post-procedure (P = 0.72) and follow-up (P = 0.29).
When we analyzed naive, untreated SBs, we observed true bifurcation lesions in 21.7% of the ZES, 24.6% of the SES, and 27.5% of the PES (P = 0.32) lesions (Table 5). After the procedure, periprocedural SB compromise from non-diseased SBs occurred in 15.8% of the ZES, 17.2% of the SES, and 16.6% of the PES (P = 0.92) lesions (Fig. 1). However, delayed SB compromise at follow-up angiography was found in 13.9% of the ZES, 3.2% of the SES, and 9.4% of the PES (P = 0.010) lesions (Fig. 2). Although SB diameter stenosis at follow-up was numerically lower in the SES than in the ZES and PES groups, this did not attain statistical significance by parametric and non-parametric analyses. The incidence of SB total occlusion was 2.1% (16 lesions). Of the 10 occluded SBs having follow-up angiography, 6 showed spontaneous recanalization.
When the degree of SB diameter stenosis was classified into four groups (< 50%, 50%-70%, 70%-99%, and 100%), worsening of SB stenosis occurred in 48 (9.0%) of lesions comprising 21 (11.6 %), 8 (4.7%), and 19 (10.4%) lesions of the ZES, SES and PES lesions (P = 0.059), respectively (Fig. 3), whereas improvement and stationary of SB stenosis were observed in 51 (9.6%) and 434 (81.4%) of lesions, respectively. In a multivariable logistic regression model, in-stent MB stenosis at follow-up (%) was the only independent predictor of worsening of SB stenosis (odds ratio, 1.03; 95% confidence interval, 1.01-1.04; P = 0.0003).
Peri-procedural MI, defined as procedure-related increase of creatine kinase or its MB isoenzyme to at least three times the upper limit of the normal range, occurred in 24 (7.9%), 33 (10.2 %), and 24 (8.2%) lesions after ZES, SES, and PES implantations, respectively (P = 0.53).
One-year clinical follow-up was completed for 97.2% of lesions, and the clinical outcomes are shown in Table 6. There were no differences among the three groups in the incidence of death or myocardial infarction. However, the incidence of target lesion revascularization for MB, SB, and stent thrombosis, were higher in the PES than in the SES lesions. All target lesion revascularizations for SB restenoses were treated percutaneously. One patient in the PES group received bypass graft surgery for MB restenosis. In naive SBs without treatment, target lesion revascularization was performed in 2 (0.7%) of the ZES, none of the SES, and 8 (2.8%) of the PES lesions (P = 0.002).
This was a substudy of the ZEST trial, a large randomized study comparing use of the three types of DESs for elective PCI in real practice. The major finding of this study was that a minority of patients experienced a worsening of SB stenosis at follow-up angiography after single-stent implantation with DES for treatment of bifurcation lesions. In addition, because follow-up SB stenosis was mainly influenced by the severity of MB stenosis, DESs effectiveness to maintain small stenosis in MB at follow-up may help maintain the luminal patency of untreated SBs.
The ZEST trial was a study of 'all-comers' undergoing elective PCI with DES in real practice. Therefore, our subgroup analysis has the advantage of allowing us to assess outcomes patterns following current bifurcation treatments. In addition, we could compare the outcomes using the three current types of DESs to treat specific bifurcation lesion sets, with minimal selection bias. Of all lesions treated with DESs, approximately one-fourth had SBs > 1.5 mm in diameter, requiring protection during PCI (10). Of these SBs, approximately 20%, or 5% of all lesions, had significant SB stenosis within true bifurcation segments. As a diseased SB is the most important predictor of SB compromise during MB stenting (8), special attention must be given to PCI lesions at risk for complications related to SB compromise. Because of the small proportion of true bifurcations, about one-fifth of bifurcations underwent SB treatment, with less than 5% of all lesions receiving stenting in both branches. Our conservative treatment pattern was indicated by previous results, showing a comparable effectiveness of single- and two-stent techniques for treatment of bifurcation lesions (4, 6, 9).
The major purposes of this study were to assess the incidence of periprocedural SB compromise and the long-term angiographic outcomes. Few previous studies have described the long-term outcomes of untreated SBs after DES implantation in the MB (13). Furthermore, the insight on the 'clinically significant SB stenosis' has not been consistent across operators. The degree of SB compromise necessitating provisional SB stenting ranged from 50% to 100% in the diverse clinical trials (3, 5, 9). We found that significant periprocedural SB compromise after MB stenting occurred in 16.5% of non-diseased SBs. Although the three DESs had different stent platforms, the incidence of periprocedural SB compromise were comparably low in all groups, indicating that the three current DES platforms are comparable in maintaining SB patency during the procedure. Consequently, kissing balloon inflation with or without SB stenting was selectively performed in about 10% of patients.
The long-term differential effectiveness of the three DESs in maintaining SB patency was measured by analysis of follow-up SB stenosis. Overall, delayed SB compromise at follow-up was observed in only 9.3% of lesions, all of which had been free of stenosis just after the main procedure, in good agreement with the findings of a previous trial (the RAVEL trial), which compared follow-up angiographic outcomes of 118 SBs after SES and 124 SBs after BMS implantation (13). Of the 12 and 9 occluded SBs, respectively, 11 (92%) and 6 (67%) spontaneously recanalized. Other studies using BMS also supported the phenomenon of natural recanalization of occluded SBs after stent implantation (12, 14, 20). In our present study, spontaneous recanalization occurred in 6 of the 10 occluded SBs. Therefore, our findings, together with previous results, suggest that routine treatment of compromised SBs (i.e., the 'oculo-stenotic reflex') during or after the procedure should be avoided, especially in lesions receiving single-stent treatment for bifurcations. Recent results from the Nordic Bifurcation III trial also suggested that routine kissing-balloon inflation of bifurcation lesions may not provide superior clinical benefit compared with provisional SB treatment (11).
In previous studies, the predictors of delayed SB stenosis or occlusion were the preprocedural morphology or stenosis of SB (12, 13). In our multivariate analysis, however, the small MB stenosis at follow-up treated with SES compared to ZES or PES might translate to improved SB stenosis at follow-up, where angiography showed that only 3% of lesions were delayed SB compromise after SES implantation, compared with 14% for ZES and 9% for PES. This finding indicates that DES with higher anti-restenotic potencies may be effective even for preservation of untreated SB patency after single-stent bifurcation treatment. Furthermore, the relative benefit of SES in reducing MB restenosis, compared with ZES or PES, was similarly observed as the major outcome of the ZEST trial (15). Nevertheless, all three DESs were associated with an improvement of stenosis in 10% of SBs and a recanalization of 60% of occluded SBs, indicating that clinical outcomes in SB stenosis are relatively benign. Only 1.2% of SB compromises underwent target lesion revascularization when MB revascularizations were performed.
Our study had several limitations. First, this was a post-hoc analysis of a large clinical trial. Therefore, although the subgroup analyzed was extracted from a large randomized study, selection bias, resulting in a lack of statistical power, could not be completely avoided. In fact, although the delayed SB compromise occurred less frequently after SES implantation for naive lesions without treatment, the numerical degree of stenosis at follow-up was not statistically significant across the different DESs. Second, due to the limitation of current angiographic analysis system, quantitative angiographic analysis was not performed for SB (21). Therefore, because of visual estimation of SB stenosis, inter- or intra-observer variations might have occurred (21). A new dedicated quantitative analysis system for bifurcation lesions may improve the accuracy of measurement. Third, because of the limited number of true bifurcation lesions, our results may not be extrapolated to treatment for complex bifurcation lesions. Fourth, a follow-up bias may occur due to the incomplete performance of angiographic follow-up. Finally, a lack of data on functional ischemia limits our understanding of the clinical implications of these angiographic results. As previously reported, the correspondence rate between angiographic stenosis and flow impairment detected by fractional flow reserve is low (7). Thus, future studies on bifurcation coronary lesions are required. We found that the long-term incidence of aggravation of SB stenosis was low and may be associated with the degree of intimal hyperplasia in the MB after DES implantation. Therefore, aggressive SB treatment of bifurcation lesions may not be necessary in real-world practice. Our results indicate the need for additional clinical studies to determine an effective SB treatment, in view of the technical complexity, clinical prognosis, and costs of procedures addressing bifurcation coronary lesions.
In conclusion, after main-branch stenting in bifurcation lesions, a minority of SB appeared to experience worsening of stenosis. DES with strong anti-restenotic efficacy may help maintain SB patency.
Figures and Tables
Fig. 1
Change in side branch stenosis between baseline and post-procedure for non-diseased side branches without treatment. Periprocedural side branch compromise, defined as ≥ 50% diameter stenosis from non-diseased (< 50%) side branches, occurred in 15.8% of the zotarolimus- (ZES), 17.2% of the sirolimus- (SES), and 16.6% of the paclitaxel-eluting stent (PES) lesions (P = 0.92).

Fig. 2
Change in side branch stenosis between post-procedure and 8-month follow-up from non-compromised side branches without treatment. Delayed side branch compromise, defined as ≥ 50% diameter stenosis at follow-up from non-compromised (< 50%) side branches, occurred in 13.9% of the zotarolimus- (ZES), 3.2% of the sirolimus- (SES), and 9.4% of the paclitaxel-eluting stent (PES) lesions (P = 0.010).

Fig. 3
Change in side branch stenosis between post-procedure and 8-month follow-up in all lesions without treatment. Changes in side branch stenosis were assessed according to stenosis group, classified as < 50%, 50%-70%, 70%-90%, and 100%. The statistical difference of incidences was not significant (NS).

References
1. Kim YH, Park DW, Suh IW, Jang JS, Hwang ES, Jeong YH, Lee SW, Lee SW, Lee CW, Hong MK, et al. Long-term outcome of simultaneous kissing stenting technique with sirolimus-eluting stent for large bifurcation coronary lesions. Catheter Cardiovasc Interv. 2007. 70:840–846.
2. Kim YH, Park SW, Hong MK, Park DW, Park KM, Lee BK, Song JM, Han KH, Lee CW, Kang DH, et al. Comparison of simple and complex stenting techniques in the treatment of unprotected left main coronary artery bifurcation stenosis. Am J Cardiol. 2006. 97:1597–1601.
3. Pan M, de Lezo JS, Medina A, Romero M, Segura J, Pavlovic D, Delgado A, Ojeda S, Melián F, Herrador J, et al. Rapamycin-eluting stents for the treatment of bifurcated coronary lesions: a randomized comparison of a simple versus complex strategy. Am Heart J. 2004. 148:857–864.
4. Colombo A, Moses JW, Morice MC, Ludwig J, Holmes DR Jr, Spanos V, Louvard Y, Desmedt B, Di Mario C, Leon MB. Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004. 109:1244–1249.
5. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006. 114:1955–1961.
6. Ferenc M, Gick M, Kienzle RP, Bestehorn HP, Werner KD, Comberg T, Kuebler P, Büttner HJ, Neumann FJ. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008. 29:2859–2867.
7. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005. 46:633–637.
8. Louvard Y, Thomas M, Dzavik V, Hildick-Smith D, Galassi AR, Pan M, Burzotta F, Zelizko M, Dudek D, Ludman P, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008. 71:175–183.
9. Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, Sheiban I, Paloscia L, Grube E, Schofer J, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009. 119:71–78.
10. Lefèvre T, Louvard Y, Morice MC, Dumas P, Loubeyre C, Benslimane A, Premchand RK, Guillard N, Piéchaud JF. Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc Interv. 2000. 49:274–283.
11. Niemelä M, Kervinen K, Erglis A, Holm NR, Maeng M, Christiansen EH, Kumsars I, Jegere S, Dombrovskis A, Gunnes P, et al. Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011. 123:79–86.
12. Poerner TC, Kralev S, Voelker W, Sueselbeck T, Latsch A, Pfleger S, Schumacher B, Borggrefe M, Haase KK. Natural history of small and medium-sized side branches after coronary stent implantation. Am Heart J. 2002. 143:627–635.
13. Tanabe K, Serruys PW, Degertekin M, Regar E, van Domburg RT, Sousa JE, Wülfert E, Morice MC. Fate of side branches after coronary arterial sirolimus-eluting stent implantation. Am J Cardiol. 2002. 90:937–941.
14. Arora RR, Raymond RE, Dimas AP, Bhadwar K, Simpfendorfer C. Side branch occlusion during coronary angioplasty: incidence, angiographic characteristics, and outcome. Cathet Cardiovasc Diagn. 1989. 18:210–212.
15. Park DW, Kim YH, Yun SC, Kang SJ, Lee SW, Lee CW, Park SW, Seong IW, Lee JH, Tahk SJ, et al. Comparison of zotarolimus-eluting stents with sirolimus- and paclitaxel-eluting stents for coronary revascularization: the ZEST (Comparison of the Efficacy and Safety of Zotarolimus-Eluting Stent with Sirolimus-Eluting and PacliTaxel-Eluting Stent for Coronary Lesions) randomized trial. J Am Coll Cardiol. 2010. 56:1187–1195.
16. Popma JJ, Leon MB, Moses JW, Holmes DR Jr, Cox N, Fitzpatrick M, Douglas J, Lambert C, Mooney M, Yakubov S, et al. Quantitative assessment of angiographic restenosis after sirolimus-eluting stent implantation in native coronary arteries. Circulation. 2004. 110:3773–3780.
17. Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, Pichard AD, Kent KM, Stone GW, Leon MB. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation. 1999. 100:1872–1878.
18. Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006. 59:183.
19. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007. 115:2344–2351.
20. Mazur W, Grinstead WC, Hakim AH, Dabaghi SF, Abukhalil JM, Ali NM, Joseph J, French BA, Raizner AE. Fate of side branches after intracoronary implantation of the Gianturco-Roubin flex-stent for acute or threatened closure after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1994. 74:1207–1210.
21. Goktekin O, Kaplan S, Dimopoulos K, Barlis P, Tanigawa J, Vatankulu MA, Koning G, Tuinenburg JC, Mario CD. A new quantitative analysis system for the evaluation of coronary bifurcation lesions: comparison with current conventional methods. Catheter Cardiovasc Interv. 2007. 69:172–180.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download