Abstract
The aim of this study was to describe the cause of the recent improvement in the outcomes of patients who experienced in-hospital cardiac arrest. We retrospectively analyzed the in-hospital arrest registry of a tertiary care university hospital in Korea between 2005 and 2009. Major changes to the in-hospital resuscitation policies occurred during the study period, which included the requirement of extensive education of basic life support and advanced cardiac life support, the reformation of cardiopulmonary resuscitation (CPR) team with trained physicians, and the activation of a medical emergency team. A total of 958 patients with in-hospital cardiac arrest were enrolled. A significant annual trend in in-hospital survival improvement (odds ratio = 0.77, 95% confidence interval 0.65-0.90) was observed in a multivariate model. The adjusted trend analysis of the return of spontaneous circulation, six-month survival, and survival with minimal neurologic impairment upon discharge and six-months afterward revealed similar results to the original analysis. These trends in outcome improvement throughout the study were apparent in non-ICU (Intensive Care Unit) areas. We report that the in-hospital survival of cardiac arrest patients gradually improved. Multidisciplinary hospital-based efforts that reinforce the Chain of Survival concept may have contributed to this improvement.
In-hospital cardiac arrest is a leading cause of morbidity and mortality. Approximately one to five of every 1,000 patients that are admitted to a hospital undergo cardiac arrest, and this contributes to the approximate 80% in-hospital mortality rate (1, 2). Despite this high mortality rate, there have been no significant changes in the in-hospital survival rate for the past several decades (3, 4).
Improving survival outcome following in-hospital cardiac arrest can be difficult due to the complexity of pre-arrest to post-resuscitation treatment. The Chain of Survival concept is useful for understanding these complexities (5, 6). The steps of the 'in-hospital chain of survival' are composed of prevention, calling for help, cardiopulmonary resuscitation (CPR), defibrillation, advanced life support, and post-resuscitation care. Recent studies have reported that several interventions aimed at enhancing the quality of care at each of these steps may improve the outcome of in-hospital arrest (7-12).
To improve the outcome of in-hospital cardiac arrest, we have implemented several interventions such as CPR education, CPR team reformation, and the activation of a medical emergency team (MET). The aim of this study was to assess the changes in outcome of adult patients who experienced in-hospital cardiac arrest over the past five years. We also attempted to show how the outcomes changed when multidisciplinary hospital-based approaches were implemented.
This study was conducted at the Samsung Medical Center, a tertiary academic hospital in Seoul, Korea that has 1,951 beds. We retrospectively analyzed a historical data set that was drawn from the in-hospital CPR registry between January 2005 and December 2009 according to Utstein-style guidelines (13). Cardiac arrest was defined as the cessation of cardiac mechanical activity as confirmed by lapse in circulation, which was determined by the absence of a palpable central pulse, unresponsiveness, and apnea according to the guidelines mentioned above. Exclusion criteria included patients younger than 15 yr of age and patients who had previously signed a "Do Not Resuscitate" order.
The major changes that occurred in the in-hospital resuscitation policies and CPR education programs are summarized in Fig. 1. Limited CPR education programs were available prior to 2008. Basic life support (BLS) training classes were rarely offered and utilized only one or two manikins for a large number of employees. For the first time in 2005, we began a brief training course for first-year residents that included airway management and CPR algorithms. In 2007, BLS and advanced cardiac life support (ACLS) education were selectively provided to physicians belonging to CPR teams.
Extensive BLS and ACLS education programs have been offered at Samsung Medical Center since 2008. More than 5,000 hospital employees per year (more than 90% of all hospital employees), regardless of job category, completed a 2-hr BLS training course that was based on the 2005 international CPR guidelines and used the practice-while-watching (PWW) method of instruction (14). The student-to-manikin ratio was between 1:1 and 1:4 in order to ensure that each trainee received an adequate amount of practice.
Simulation ACLS training and team approaches were selectively provided for doctors and nurses. Official American Heart Association (AHA) ACLS courses or hospital-specific programs were used for the ACLS education programs. First-year residents from all departments, senior residents, and fellows from the departments of Internal Medicine and Surgery, intensivists, cardiologists, and emergency physicians all completed these courses.
ACLS-trained physician coverage was less than 20% prior to 2007. The coverage increased to 50% in 2007 and surpassed 80% in 2008 and 2009. The CPR teams were reorganized in October of 2007 to increase the emergency physician coverage, especially in the general wards. The in-hospital CPR committee reviewed cases of cardiac arrest on a weekly basis and monitored the adequacies of the initial response and performance of the CPR team. Feedback was provided to the initial responders and CPR team members when necessary.
Another alteration in the program was the activation of an MET in 2009. The team consisted of specialists, senior internal medicine residents, and respiratory therapists. The members of the MET also responded to cardiac arrests as members of the CPR team, especially in the intensive care unit (ICU).
One of the noticeable non-interventional changes was the expansion of the cancer center in January of 2008, in which 699 general ward beds and 21 ICU beds were added.
The primary endpoint was in-hospital survival. The secondary endpoints included the return of spontaneous circulation (ROSC), six-month survival, and neurologic status, which were assessed according to the Glasgow-Pittsburgh cerebral performance categories (CPC) score upon discharge and again after six months (15). ROSC was defined as the onset of an organized rhythm with a palpable pulse and a measurable blood pressure for at least 20 min (10). Survival with minimal neurologic impairment was defined as a CPC score ≤ 2. Data was obtained from the reviews of medical records and telephone interviews conducted by research nurses.
Continuous variables were expressed as the mean ± standard deviation or the median (interquartile range). These variables were compared using the Kruskal-Wallis test, while categorical variables were compared with a chi-square test. Multiple logistic regression analysis was used to evaluate the adjusted trends in the outcome variables throughout the five-year study period. Each year of the study period was converted to a continuous variable. In addition to the demographic factors and the CPR variables, the maximal value of the Sequential Organ Failure Assessment (SOFA) score in the 24 hr prior to the arrest and the Deyo-Charlson score were used to reflect the burden of comorbidities and to adjust for pre-arrest conditions, respectively (3, 16-18). Those variables were selected according to previous reports about in-hospital arrest (19, 20). Cox regression analysis was used to estimate the hazard ratio (HR) of the six-month mortality. All values of odds ratio (OR) or HR were shown using modeling mortality, significant neurologic deficit, or failure to achieve ROSC. Version 11.0 of the Stata software was used to perform the statistical analyses, and two-tailed P values < 0.05 were considered to be significant.
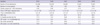
A total of 1,185 in-hospital cardiac arrests occurred during the study period. Of these patients, 227 were excluded from the study because they were younger than 15 yr of age (n = 196), had signed a "Do Not Resuscitate" order (n = 27), or data on the patient was insufficient (n = 4). Ultimately, there were a total of 958 patients in the study population. The baseline characteristics and the comparative results throughout the five year study period are shown in Table 1. There were no significant differences except for the location of arrest.
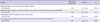
The total number of admissions had noticeably increased in 2008 (Table 2). On the other hand, the occurrence of cardiac arrests per 1,000 admissions slightly decreased beginning in 2007, although this decrease was not statistically significant. There was no significant difference in the time interval from the time of arrest or the time at which the CPR team responded and performed defibrillation.
In terms of the outcome variables, there was a gradual trend of improvement between the years of 2005 and 2009. The survival rate was lowest in 2006 and highest in 2009. We also compared the survival rates according to the location of arrest, which revealed significant differences in the incidence (Fig. 2). The improvement in survival was prominent in the general ward, the outpatient department, radiologic examination rooms, and public spaces throughout the hospital.
The multivariate regression model that was used to evaluate the factors associated with in-hospital mortality is presented in Table 3. The model showed that the annual trend of improvement in in-hospital survival was significant (odds ratio of mortality = 0.77, 95% confidence interval 0.65-0.90). Other factors associated with survival were shockable rhythm, surgical illness category, and the use of percutaneous cardiopulmonary support. Predictors for mortality were age, CPR duration, cause of arrest (septic cause), Deyo-Charlson score, and pre-arrest SOFA score.
Adjusted odds ratios or hazard ratios for the secondary endpoints, which were derived from the additional multivariate models using the same variables, are also shown in Table 4. The results are similar to those obtained from the original analysis.
The survival rate of patients with in-hospital cardiac arrest has been unchanged for the past several decades (3, 4, 21). However, we have recently experienced a significant improvement in the outcomes of in-hospital arrest victims between the years of 2005 and 2009. In this report, we attempted to identify the historically implemented multidisciplinary efforts that resulted in these improvements. Major changes that occurred were the addition of extensive BLS and ACLS education programs, CPR team reformation with trained physicians, and the activation of an MET. Another non-interventional change was the expansion of the hospital.
Improving survival after in-hospital cardiac arrest requires an integrated set of coordinated actions that are described by the "Chain of Survival." (22) Therefore, multifaceted efforts that reinforce the Chain of Survival could potentially show a synergistic effect compared to that of a single method of intervention. Strengthening these procedures to maximize survival outcome also requires effective resuscitation education and the implementation of high quality treatment (22, 23).
The quality of the CPR procedure has been shown to affect post-cardiac arrest survival rates, and effective CPR training is particularly vital in maintaining that high quality (22-25). Our BLS education program emphasized chest compressions, minimal interruptions, and the importance of avoiding hyperventilation in order to enhance the quality of the CPR procedure. We hypothesize that these changes played key roles in improving the outcomes of cardiac arrests, although we were unable to directly compare the quality of CPR among performers. Further studies are needed to examine the effects of these changes on implementation and skill retention.
Increases in the number of ACLS-trained team members present at in-hospital resuscitation training efforts might increase the survival rate following cardiac arrest (7, 26). ACLS training improves the resuscitation skills, knowledge, and performance of CPR teams. ACLS education is also thought to play a beneficial role in cardiac arrest prevention according to a study indicating that the introduction of a simple and widespread educational program was associated with reductions in both the number of in-hospital cardiac arrests and unsuccessful cardiopulmonary resuscitation attempts (8).
The MET, which is a well-known tool for cardiac arrest as the first link in the Chain of Survival, was introduced to our hospital in January 2009 (1, 5, 6, 12). It was shown to have a positive effect in a previously published prospective, historically controlled study from our hospital. The presence of an MET decreased the incidence of cardiac arrest in the general wards and the ICU-dearranged time, which is the time interval between the initial physiologic derangement that meets the MET activation criteria and ICU admission (27). While we were unable to fully evaluate the effects of MET activation, we hypothesize that the MET positively affected the trend of decreasing cardiac arrest events in 2009.
The locations of the general wards and the emergency department (ED) are known to be associated with the worst outcomes (19). In addition, overall ED overcrowding has been aggravated even though the length of stay in the ED has decreased through hospital expansion. Therefore, we were encouraged by the improvements in survival observed in both the general wards and the ED.
On the other hand, the increasing numbers of admissions into the ICU might affect the improvement in survival in our study because ICU admission is a known predictor for survival in in-hospital arrest patients. A possible explanation for these results is the more timely ICU admission of a patient from a non-ICU area prior to deterioration. Other important contributing factors might include early recognition and transfer of critically ill patients to the ICU and the availability of ICU beds. The increased availability of ICU beds due to hospital expansion was thought be especially associated with the decreasing number of arrests in the emergency department.
The ROSC and survival rates in 2007 were the second highest among the years studied. This may indicate that other changes had taken place or a high natural yearly variability. For example, a previous report from a single center showed a very high variability that ranged from 25% to 45% (28). In our study, we identified relatively clear time trends using multivariate models. We also determined that the number of trained physicians and their coverage began to increase by selective education in 2007.
Therapeutic hypothermia, which has an important role in post-arrest care, is one of the principal treatment modalities in patients with cardiac arrest. However, it has not been accepted as a standard treatment for in-hospital arrest at our hospital and has been applied in only four cases since 2007. The potential synergistic effect of hypothermia with our implementations requires further study.
Our study has several limitations due to the fact that it is a single- center, retrospective, nonrandomized, observational study. First, we were unable to identify which interventions were directly associated with improvements in survival. We did not compare prospective data or the objective measurements with the quality of CPR as measured by the chest compression rate, hyperventilation, and the rate of the first responder CPR. The interventions were individually implemented. Second, we were unable to fully adjust for the effects of the changes in the overall case mixture, staffing, or hospital environment. Hidden biases may remain, although our statistical approach should have reduced these levels. Finally, there was great variability in the baseline hospital characteristics and survival within different areas (29, 30). The results of this study may not be applicable to other hospitals in other regions since our study was based on the data from a single tertiary teaching hospital in Korea. We believe that a locally implemented strong in-hospital chain of survival, which is customizable to specific requirements, is probably the best way to improve outcomes in individual hospitals (29).
We report that the in-hospital survival of cardiac arrest patients gradually improved between the years of 2005 and 2009, especially in non-ICU areas of the hospital. Multidisciplinary hospital-based efforts that reinforce the concepts of Chain of Survival may have contributed to the improvement in survival of cardiac arrest patients.
Figures and Tables
 | Fig. 1Major changes in the in-hospital resuscitation policies and CPR education programs. CPR, cardiopulmonary resuscitation; BLS, basic life support; ACLS, advanced cardiac life support; AHA, American Heart Association. |
 | Fig. 2Annual changes in the in-hospital survival rate according to the location of arrest. ICU, intensive care unit; OR, operating room; Cath lab, catheterization laboratory. |
Table 1
Baseline clinical characteristics and cardiopulmonary resuscitation variables throughout the five year study period

Table 2
Annual changes in cardiac arrests per 1,000 admissions, response time, and outcome variables
ACKNOWLEDGMENTS
We thank In Jung Woo and Kyongnam Yoo, charge nurses from the Office of CPR Operations and Training, for managing the BLS and ACLS training programs. We also thank Hee Kyoung Choi, a research nurse working in the emergency department, for his assistance in data collection. We appreciate the excellent educational support of Aerin Yoon, a charge nurse at the Clinical Simulation Center.
References
1. Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007. 33:237–245.
2. Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O'Donnell C, Kittner S, Lloyd-Jones D, Goff DC Jr, Hong Y, Adams R, Friday G, Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P, Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006. 113:e85–e151.
3. Ehlenbach WJ, Barnato AE, Curtis JR, Kreuter W, Koepsell TD, Deyo RA, Stapleton RD. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009. 361:22–31.
4. Bloom HL, Shukrullah I, Cuellar JR, Lloyd MS, Dudley SC Jr, Zafari AM. Long-term survival after successful inhospital cardiac arrest resuscitation. Am Heart J. 2007. 153:831–836.
5. Perkins GD, Soar J. In hospital cardiac arrest: missing links in the chain of survival. Resuscitation. 2005. 66:253–255.
6. Smith GB. In-hospital cardiac arrest: is it time for an in-hospital 'chain of prevention'? Resuscitation. 2010. 81:1209–1211.
7. Moretti MA, Cesar LA, Nusbacher A, Kern KB, Timerman S, Ramires JA. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. 2007. 72:458–465.
8. Spearpoint KG, Gruber PC, Brett SJ. Impact of the Immediate Life Support course on the incidence and outcome of in-hospital cardiac arrest calls: an observational study over 6 years. Resuscitation. 2009. 80:638–643.
9. Thigpen K, Davis SP, Basol R, Lange P, Jain SS, Olsen JD, Erickson BR, Schuchard TN, Aufderheide TP. Implementing the 2005 American Heart Association guidelines, including use of the impedance threshold device, improves hospital discharge rate after in-hospital cardiac arrest. Respir Care. 2010. 55:1014–1019.
10. Edelson DP, Litzinger B, Arora V, Walsh D, Kim S, Lauderdale DS, Vanden Hoek TL, Becker LB, Abella BS. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008. 168:1063–1069.
11. Sandroni C, Ferro G, Santangelo S, Tortora F, Mistura L, Cavallaro F, Caricato A, Antonelli M. In-hospital cardiac arrest: survival depends mainly on the effectiveness of the emergency response. Resuscitation. 2004. 62:291–297.
12. Konrad D, Jäderling G, Bell M, Granath F, Ekbom A, Martling CR. Reducing in-hospital cardiac arrests and hospital mortality by introducing a medical emergency team. Intensive Care Med. 2010. 36:100–106.
13. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. International Liaison Committee on Resuscitation. American Heart Association. European Resuscitation Council. Australian Resuscitation Council. New Zealand Resuscitation Council. Heart and Stroke Foundation of Canada. InterAmerican Heart Foundation. Resuscitation Councils of Southern Africa. ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004. 110:3385–3397.
14. International Liaison Committee on Resuscitation. 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 8: Interdisciplinary topics. Resuscitation. 2005. 67:305–314.
15. Prohl J, Röther J, Kluge S, de Heer G, Liepert J, Bodenburg S, Pawlik K, Kreymann G. Prediction of short-term and long-term outcomes after cardiac arrest: a prospective multivariate approach combining biochemical, clinical, electrophysiological, and neuropsychological investigations. Crit Care Med. 2007. 35:1230–1237.
16. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992. 45:613–619.
17. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001. 286:1754–1758.
18. Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med. 1998. 26:1793–1800.
19. Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation. 2010. 81:302–311.
20. Shin TG, Choi JH, Jo IJ, Sim MS, Song HG, Jeong YK, Song YB, Hahn JY, Choi SH, Gwon HC, Jeon ES, Sung K, Kim WS, Lee YT. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: a comparison with conventional cardiopulmonary resuscitation. Crit Care Med. 2011. 39:1–7.
21. Tian J, Kaufman DA, Zarich S, Chan PS, Ong P, Amoateng-Adjepong Y, Manthous CA. American Heart Association National Registry for cardiopulmonary Resuscitation Investigators. Outcomes of critically ill patients who received cardiopulmonary resuscitation. Am J Respir Crit Care Med. 2010. 182:501–506.
22. Bhanji F, Mancini ME, Sinz E, Rodgers DL, McNeil MA, Hoadley TA, Meeks RA, Hamilton MF, Meaney PA, Hunt EA, Nadkarni VM, Hazinski MF. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010. 122:S920–S933.
23. Soar J, Monsieurs KG, Ballance JH, Barelli A, Biarent D, Greif R, Handley AJ, Lockey AS, Richmond S, Ringsted C, Wyllie JP, Nolan JP, Perkins GD. European Resuscitation Council Guidelines for Resuscitation 2010 Section 9. Principles of education in resuscitation. Resuscitation. 2010. 81:1434–1444.
24. Chamberlain DA, Hazinski MF. European Resuscitation Council. American Heart Association. Heart and Stroke Foundation of Canada. Australia and New Zealand Resuscitation Council. Resuscitation Council of Southern Africa. Consejo Latino-Americano de Resuscitación. Education in resuscitation. Resuscitation. 2003. 59:11–43.
25. Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, Vanden Hoek TL, Becker LB. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005. 293:305–310.
26. Dane FC, Russell-Lindgren KS, Parish DC, Durham MD, Brown TD. In-hospital resuscitation: association between ACLS training and survival to discharge. Resuscitation. 2000. 47:83–87.
27. Lim SY, Park SY, Park HK, Kim M, Park HY, Lee B, Lee JH, Jung EJ, Jeon K, Park CM, Ko MG, Park MR, Nam JM, Won SY, Jung JH, Cho SH, Suh GY. Early impact of medical emergency team implementation in a country with limited medical resources: a before-and-after study. J Crit Care. 2011. 26:373–378.
28. Fredriksson M, Aune S, Thorén AB, Herlitz J. In-hospital cardiac arrest: an Utstein style report of seven years experience from the Sahlgrenska University Hospital. Resuscitation. 2006. 68:351–358.
29. Skrifvars MB, Castrén M, Aune S, Thoren AB, Nurmi J, Herlitz J. Variability in survival after in-hospital cardiac arrest depending on the hospital level of care. Resuscitation. 2007. 73:73–81.
30. Carr BG, Kahn JM, Merchant RM, Kramer AA, Neumar RW. Inter-hospital variability in post-cardiac arrest mortality. Resuscitation. 2009. 80:30–34.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download