Abstract
Exposure to cephalosporins could cause occupational allergic diseases in health care workers (HCWs). We evaluated the prevalence of serum specific IgE and IgG antibodies to cephalosporin-human serum albumin (HSA) conjugate and to identify potential genetic risk factors associated with sensitization to cephalosporins in exposed HCWs. The study population consisted of 153 HCWs who had been exposed to antibiotics in a single university hospital and 86 unexposed healthy controls. A questionnaire survey of work-related symptoms (WRS) was administered. A skin-prick test (SPT) was performed, and serum-specific IgE and IgG antibodies to 3 commonly prescribed cephalosporins were measured by ELISA. Four single-nucleotide polymorphisms of the candidate genes related to IgE sensitization were genotyped. The prevalence of WRS to cephalosporins was 2.6%. The prevalence rates of serum-specific IgE and IgG antibodies to cephalosporins were 20.3% and 14.7%, respectively. The FcεR1β-109T > C polymorphism was significantly associated with IgE sensitization to cephalosporins in HCWs (P = 0.036, OR = 3.553; CI, 1.324-9.532). The in vitro functional assay demonstrated that the T allele of FcεR1β-109T had greater promoter activity than did the C allele (P < 0.001). The FcεR1β-109T > C polymorphism may be a potential genetic risk factor for increased IgE sensitization to cephalosporins.
Occupational allergies caused by medicines in the hospital environment are becoming a problem for health care workers (HCWs). Digestive enzymes (1) and antibiotics (2, 3) are the main drugs that induce occupational allergies in Korea. In recent years, cephalosporins have become the most commonly prescribed antibiotics in most hospitals. These agents cause IgE-mediated reactions such as urticaria, angioedema, and anaphylaxis after sensitization.The early detection of sensitized workers may be critical for preventing the development of occupational allergies due to digestive enzymes and antibiotics (4). Although the pathogenic role of IgE in cephalosporin allergy is well known, about 30%-50% of patients with cephalosporin allergy show normal IgE levels (5). The roles of IgG antibodies in inducing or modifying allergic reactions have not been sufficiently investigated, but the T-cell system is also activated and involved in drug allergy and promotes the synthesis not only of IgE but also of IgG (6).
Workplace allergens can be categorized as either high (HMW) or low molecular weight (LMW) allergens. HMW allergens such as digestive enzymes cause allergic sensitization via an IgE-mediated mechanism (7), whereas LMW allergens such as antibiotics act as haptens and can cause sensitization that may or may not be associated with specific IgE (8). The main factors that affect the onset of symptoms are the type, duration, and intensity of allergen exposure (4).
Host genetic factors can modulate how individuals interact with these environmental agents and change individual susceptibility to occupational allergic diseases. The high-affinity receptor for IgE (FcεR1β) plays a central role in the induction and maintenance of IgE sensitization, as the FcεR1β gene, such as FcεR1β-109C > T (9) and FcεR1β-237A > G (10), is associated with elevated total and specific IgE levels and immediate penicillin allergy. Interleukin-4 (IL-4) is a major cytokine in IgE production and is involved in IgE-mediated responses. IL-4-589T > C (11) and IL-4-33C > T (12) have been shown to be associated with increased serum total IgE levels as well as the development of asthma and drug allergy. Given this background, we hypothesized that four single-nucleotide polymorphisms (SNPs) may be associated with occupational allergy due to cephalosporins in exposed HCWs: FcεR1β-109T > C, FcεR1β-237A > G, IL-4-589T > C, and IL-4-33C > T.
The present study was performed to evaluate the prevalence of IgE and IgG sensitization to commonly used cephalosporins in exposed HCWs and possible associations with these four candidate SNPs.
A total of 153 exposed HCWs and 86 unexposed nonatopic healthy controls were enrolled from Ajou University Hospital and the general population. The HCWs were all non-smoking women who were either nurses or pharmacists. They were regularly exposed to cephalosporins in their workplaces during the mixing and preparation of medications. The healthy controls were non-atopics and had no personal history of allergic disease or antibiotic allergy. All subjects were asked to complete written questionnaires, which addressed the duration of work, history of allergic disease, and work-related symptoms (WRS). WRS included respiratory symptoms, such as rhinorrhea, cough, dyspnea, wheezing, or cutaneous symptoms, such as urticaria or dermatitis, during and after handling any cephalosporins.
All of the subjects underwent a skin-prick test (SPT) using common aeroallergens (Dermatophagoides pteronyssinus, Dermatophagoides farina, tree pollens, grass pollens, weed pollens, dog dander, and cat dander; Bencard, Brentford, UK) and two cephalosporins (ceftriaxone and ceftizoxime, each 10 mg/mL). Normal saline and 1 mg/mL histamine were used as negative and positive controls, respectively. SPT was considered positive when a wheal larger than 3 mm with surrounding erythema was present 15 min after exposure. Atopy was defined as a positive SPT with at least one common aeroallergen. The total serum IgE level was measured using the ImmunoCAP System (Phadia, Uppsala, Sweden).
The most commonly prescribed cephalosporins were studied: cefotiam, ceftriaxone, and ceftizoxime. To detect serum-specific IgE and IgG to cephalosporins, three cephalosporin-human serum albumin (HSA) conjugates were prepared in our laboratory, and ELISA was performed as described previously (13, 14). The positive cutoff value of the ELISA was determined as the mean plus three standard deviations (SD) of the healthy controls. An ELISA inhibition test was performed to demonstrate the specificity of specific IgE binding as described previously (14).
Four genetic polymorphisms, FcεR1β-109T > C, FcεR1β-237A > G, IL-4-589T > C, and IL-4-33C > T, were genotyped using SNaPshot ddNTP primer-extension kits (Applied Biosystems, Foster City, CA, USA).
A 31-bp fragment of human FcεR1β gene promoter was amplified by PCR using specific primers, and the PCR products were used to prepare constructs as described in our previous report (15). Human mast cells (HMC-1) were transfected using an MP-100 microporator (Distal Biotechnology, Seoul, Korea) according the manufacturer's instructions. Briefly, 5 × 105 cells were seeded in 24-well plates and transfected with 1 µg of the reporter construct and 5 ng of Renilla control vector. Microporation was performed at 1,750 V with a pulse width of 20 ms for HMC-1. At 24 hr posttransfection, the cells were lysed and assayed for luciferase activity using Synergy 2 (BioTek, Winooski, VT, USA). The pGL3-control (Promega, Madison, WI, USA) and the promoterless pGL3-basic vectors were used as positive and negative controls, respectively. Transfection efficiency was determined by measuring Renilla activity after co-transfection of both the reporter construct and the Renilla control vector into the cell line.
Quantitative and qualitative results are given as means ± SD and absolute numbers or frequencies, respectively. Descriptive statistics were performed using SPSS ver. 12.0 (SPSS, Chicago, IL, USA). Statistical significance was assessed using the Mann-Whitney U-test for continuous variables and Fisher's exact test for categorical variables. Logistic regression analysis was used to estimate adjusted odds ratio (OR) for IgE and IgG sensitization to cephalosporins associated with the genetic polymorphisms. The regression analyses were adjusted for age, atopy, and occupation. Associations are expressed as the adjusted logistic OR and 95% confidence intervals (CI). P values were corrected using Bonferroni's test (R 2.7.1; R Foundation for Statistical Computing, Vienna, Austria), which is a statistical means of correcting for the confounding effects of multiple genetic and clinical factors. In all analyses, P < 0.05 was taken to indicate statistical significance.
All of the HCWs were women, and their mean age was 26.65 ± 3.25 yr. Of the 86 healthy controls, 61 (70.9%) were women, and their mean age was 22.7 ± 3.28 yr, which was significantly younger than the HCWs (P < 0.001). The 153 exposed HCWs were nurses (n = 135) or pharmacists (n = 18). The mean age of the nurses was significantly older than that of the pharmacists (26.84 ± 3.16 vs 25.22 ± 3.62 yr, respectively; P = 0.046). The mean duration of exposure of the HCWs was 41.34 ± 27.8 months, and there was no significant difference between the two groups (41.96 ± 26.57 vs 36.59 ± 36.61 months for nurses and pharmacists, respectively; P = 0.565). Four (2.6%) of the HCWs complained of WRS; all four were nurses, and two had histories of allergic disease. Respiratory and cutaneous symptoms were reported in three cases. Fifty-one (33.6%) had atopy, and 48 (31.4%) had a history of allergic disease, including asthma in 15 (9.8%), allergic rhinitis in 20 (13.1%), atopic dermatitis in 23 (15%), and allergic conjunctivitis in 7 (4.6%). There were no significant differences in the prevalences of previous allergic disease, antibiotic allergy, or atopy rate between the two groups. The mean serum total IgE level was 124.35 ± 211.25 KU/L, and the difference between the two groups was not significant (118.12 ± 204.39 vs 258.8 ± 61 KU/L in nurses and pharmacists, respectively; P = 0.323; Table 1).
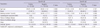
SPT with cephalosporins identified a single positive response in one (0.7%) HCW, who had a positive response to ceftriaxone. All the healthy controls showed negative results to SPT with aeroallergens and cephalosporins. The serum-specific IgE levels to each cephalosporin-HSA conjugate are shown in Fig. 1. Of the 153 HCWs tested, 31 (20.3%) had serum-specific IgE to at least one cephalosporin-HSA conjugate: 13.8% were positive for cefotiam, 5.5% for ceftizoxime, and 3.9% for ceftriaxone. Nineteen (14.7%) had serum-specific IgG antibodies: 11.5% were positive for cefotiam, and 3.7% for ceftriaxone; specific IgG to ceftizoxime was not detected (data not shown). No significant differences were found between the two occupational groups (Table 1). The specificity of the cephalosporin-HSA conjugate was analyzed using the ELISA inhibition test. The results indicated significant dose-dependent inhibition with serial addition of each cephalosporin conjugate and free cephalosporin (data not shown). There were no associations between the clinical parameters and the presence of WRS or serum-specific IgE and IgG antibodies to cephalosporin-HSA conjugate, except that the mean serum total IgE level was significantly higher in subjects without compared to those with serum-specific IgE (74 ± 85.33 vs 137.24 ± 231.32 KU/L, respectively; P = 0.016; Table 2).
Possible risk factors for positive serum-specific IgE and IgG to cephalosporin-HSA conjugate were analyzed using multiple logistic regression, controlling for age, atopy, and occupation. However, no significant risk factors were found (data not shown). Forty-four of the HCWs (28.8%) had either high serum-specific IgE or IgG to cephalosporin-HSA conjugate. Six (13.6%, n = 6/44) had both serum-specific IgE and IgG antibodies, four were positive for cefotiam-HSA conjugate, and two were positive for ceftriaxone-HSA conjugate. However, none reported WRS or showed a positive SPT response to cephalosporins. Twenty-five (56.8%, n = 25/44) had only serum-specific IgE antibodies, and 13 (29.6%, n = 13/44) had only serum-specific IgG antibodies.
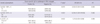
Four polymorphisms were genotyped in the 153 HCWs: FcεR1β-109T > C, FcεR1β-237A > G, IL-4-589T > C, and IL-4-33C > T. As the genotype distribution of the IL-4-589T > C polymorphism completely matched that of IL-4-33C > T polymorphism, the IL-4-589T > C polymorphism was excluded from the genetic analysis. The FcεR1β-109T > C polymorphism was significantly related to IgE sensitization to cephalosporin-HSA conjugate (P = 0.036). Furthermore, subjects with the TT genotype of FcεR1β-109T > C showed serum-specific IgE to cephalosporin-HSA conjugate significantly more often than did those carrying the CC or CT genotype (OR = 3.553; CI, 1.324-9.532) in multiple logistic regression controlling for age, atopy, and occupation. The IL-4-33C > T and FcεR1β-237A > G polymorphisms were not significantly associated with IgE sensitization to cephalosporin-HSA conjugate after adjusting for multiple comparisons with the Bonferroni test (Table 3). Moreover, no significant differences were found in the serum total IgE levels or atopy rate according to the genetic polymorphisms in total HCWs or in subjects with IgE sensitization to cephalosporin-HSA conjugate (data not shown). With regard to specific IgG sensitization, no associations were found with the four candidate gene polymorphisms.
To determine whether the FcεR1β-109T > C polymorphism is associated with altered promoter activity, a construct composed of the promoter sequence and luciferase reporter gene was transfected into HMC-1 cells. The construct containing the -109T allele exhibited significantly greater luciferase activity when compared with the constructs containing the -109C allele in HMC-1 cells (P < 0.001, Fig. 2).
The environments in which HCWs routinely work, including hospitals, clinics, and laboratories, are increasingly recognized as hazardous. Over the past few decades, latex allergy has become a major occupational health concern in hospitals, and this has since decreased with the increasing use of latex-free products. Drugs are one of the most common causes of occupational allergic diseases in HCWs. Digestive drugs, including pancreatic extracts, have been identified as occupational allergens that result in IgE-mediated respiratory symptoms in HCWs (16) and pharmaceutical workers (17). Beta-lactams, such as penicillins and cephalosporins, also cause occupational allergic diseases (18). Cephalosporins are the most widely used antibiotics for treating common infections in both outpatients and those admitted to hospital. As local administration and frequent exposure may increase sensitization, it is important to identify susceptibility factors associated with cephalosporin-induced occupational allergic diseases in exposed HCWs.
IgE-mediated reactions to beta-lactams in HCWs occur via skin contact (19) or inhalation (2). Skin contact to cefotiam can induce hand eczema, urticaria, and anaphylaxis (2, 20). SPT with cefotiam may lead to the development of new sensitization, and therefore it was excluded from the SPT battery in this study. Among hospital nurses without penicillin allergy, 12% showed a positive response on SPT or intradermal testing to penicillin in a Turkish population (21). Choi et al. (2) reported a sensitization rate of 2.6% to beta-lactams by SPT in nurses working in a tertiary hospital, and most of these cases were associated with contact urticaria. Regarding cephalosporins, Kim et al. (14) reported an IgE sensitization rate of 17.4% based on positive serum-specific IgE to three cephalosporins-HSA conjugates by ELISA in another cohort, whereas the sensitization rate based on SPT was very low (3.1%). In the present study, WRS occurred in 2.6% of HCWs, and the sensitization rate to cephalosporins on SPT was 0.7%, whereas serum-specific IgE was found in 20.1% of HCWs. There was no significant association between WRS and IgE sensitization, which may reflect the low prevalence of WRS in our cohort, as Donnay et al. (22) demonstrated underestimation of self-reported occupational exposure in a questionnaire administered to hospital workers. Diagnostic skin tests with cephalosporins are still considered experimental and show low sensitivity compared with the detection of serum specific IgE antibody because the antigenic determinants of each cephalosporin are unknown. Serum-specific IgE to cefteram was detected by ELISA in pharmaceutical company workers, in which ELISA, but not SPT, may be useful for detecting asymptomatic sensitized subjects among exposed workers (3). In this study, we detected higher positive rates of serum-specific IgE to three commonly prescribed cephalosporins than SPT in exposed HCWs. The reproducibility of ELISA and the specificity of IgE binding were confirmed with three repeated tests and the ELISA inhibition test and were also confirmed in our previous study (14). These findings suggest that it may be useful to set up an immunosurveillance system to monitor serum specific IgE to exposed cephalosporins using ELISA for screening and monitoring of susceptible individuals.
IgG antibody has been suggested to be related to occupational allergic reactions. Baker's asthma is one of the most common occupational respiratory disorders caused by HMW allergens in wheat flour. Wheat-specific IgG antibody was shown to be significantly associated with the intensity of wheat flour exposure and also WRS (23). With regard to occupational asthma (OA) caused by LMW allergens, serum-specific IgG antibody was useful to diagnose isocyanate-induced OA (24). The prevalence of specific IgG to methylene diphenyl diisocyanate (MDI) was 20.7% among MDI-exposed workers and was strongly associated with the prevalence of MDI-induced OA (25). Although the role of IgG antibody in allergic reaction has not been sufficiently clarified, it was reported that FcγRIII (low-affinity receptor for IgG) with IgG-containing immune complexes activated mast cells and basophils to produce anaphylactic reactions very similar to those induced through FcεR1 (26). Additionally, IgG4, a subclass of IgG, is produced as a result of a prolonged antigen exposure, and atopic disease and chronic allergen exposure are associated with elevated levels of specific IgG4, which was promoted by Th2 cytokines (27). In the present study, 14.7% of the HCWs had high serum-specific IgG to cephalosporin-HSA conjugate. The prevalence of serum-specific IgG antibody was not associated with WRS or serum-specific IgE antibody. Although the role of specific IgG antibody in the pathogenesis of cephalosporin-induced occupational allergic reactions is not clear in HCWs, it may represent a history of exposure to cephalosporin.
Some risk factors for sensitization to antibiotics have been reported. The class of drug, duration, frequency, and route of administration, intensity of exposure, and female gender are all predictors of developing drug allergy (28). This study evaluated sensitization to three cephalosporins, and the study subjects were all women. The duration of employment could reflect exposure duration, and the occupation reflected intensity of exposure. In the present study, the sensitization rate was not associated with exposure duration or intensity. Previous studies suggested that a history of allergic disease and atopy predispose HCWs to work-related allergic diseases (29). The causative agents were mostly HMW agents, such as latex and chemical agents, but not drugs. Atopy was related to sensitization to HMW allergens (30) but not to LWM allergens (8). Additionally, most drug allergies were not related to atopy (31). In the present study, neither atopy nor a history of allergic disease was related to WRS or to the presence of serum-specific IgE and IgG antibody, and no significant predisposing factors were found. These observations were comparable to our previous study of IgE sensitization to cefteram in pharmaceutical industry workers, which found no predisposing factors (3).
There is marked interindividual variation in susceptibility to occupational sensitization, despite similar workplace exposures, suggesting underlying differences in individual susceptibility. Recent genetic epidemiology research focused on common gene variants and identified a number of genetic associations and gene/environment interactions for allergic diseases. Several groups have reported genes that contribute to the development of drug allergy. Some studies showed that the FcεR1β-109C > T gene encoding the β-chain of FcεR1β was associated with elevated total and specific IgE levels in subjects with asthma (32) or without asthma (9). The association of the FcεR1β-237A > G polymorphism with the development of penicillin allergy was suggested (10). Qiao et al. (10) suggested that the AG or GG genotype of the FcεR1β-237A > G polymorphism contributes to the development of penicillin allergy via the production of specific IgE. With regard to the IL-4 gene, the T allele of IL-4-589T > C, known as the promoter region of IL-4, is related to asthma and elevated serum total IgE (11). The IL-4-33C > T polymorphism was shown to be significantly associated with penicillin allergy in an American population (12) and associated with asthma, serum IL-4, and total IgE levels in a Russian population (33).
To date, no study has identified potential genetic risk factors for antibiotic-induced occupational allergy in exposed HCWs. In the present study, the FcεR1β-109T > C polymorphism was significantly associated with IgE sensitization to cephalosporin-HSA conjugate in exposed HCWs, whereas no genetic associations were found with IgG sensitization. The IgE-mediated immediate hypersensitivity reaction is triggered by antigens cross-linking with IgE antibody bound to high-affinity IgE receptors on mast cell surfaces, and the FcεR1β plays a central role in the induction and allergic responses of mast cells and basophils (34). Moreover, the β-chain of FcεR1β plays a critical role via its capacity to amplify FcεR1β signaling and cell-surface expression. The FcεR1β gene is located on chromosome 11q13, which is a region that has been linked to atopy and asthma (35). The T allele at FcεR1β-109T > C was shown to be a risk factor for elevated total IgE and asthma status in Japanese subjects (32). Kim et al. (15) reported that the FcεR1β-109T > C polymorphism enhanced IgE sensitization to staphylococcal superantigens and eosinophil inflammation in patients with aspirin-exacerbated respiratory disease. Moreover, an in vitro functional study in mouse fibroblasts showed that the transition from C to T at -109 bp in the promoter region resulted in greater transcriptional activation. Another in vitro functional study using rat basophils and human airway epithelial cells showed increased promoter activity with the T allele of FcεR1β-109 compared with the C allele (15). In the present study, among the SNPs screened, the TT genotype of FcεR1β-109T > C was significantly associated with increased IgE sensitization to cephalosporin-HSA conjugate in exposed HCWs, indicating that the subjects carrying the T allele of FcεR1β showed higher levels of FcεR1 expression, leading to increased susceptibility to IgE sensitization to exposed cephalosporins in the work environment. As human mast cells are the most important effector cells for IgE sensitization, we set up an in vitro functional study to evaluate the genetic effects of FcεR1β-109T > C polymorphism using HMC-1 cells. We found significantly increased promoter activity of the FcεR1β T allele compared to the C allele in HMC-1 cells, indicating that FcεR1β expression may be increased at the human mast cell surface, leading to increased IgE sensitization to antibiotic exposure in the workplace. These findings suggest that the FcεR1β-109T > C polymorphism may be a potential genetic risk factor for IgE sensitization to cephalosporins in exposed HCWs. Further studies are needed to identify other genetic markers related to IgE sensitization to cephalosporins and other antibiotics.
In conclusion, 20.3% and 14.7% of the exposed HCWs working in a university hospital showed IgE and IgG sensitization to cephalosporins, respectively. The FcεR1β-109T > C polymorphism may be a useful genetic marker for enhanced IgE sensitization to cephalosporins.
Figures and Tables
Fig. 1
Serum-specific IgE levels in response to cephalosporin-human serum albumin (HSA) conjugates in health care workers (●) and unexposed nonatopic healthy controls (○): (A) cefotiam-HSA conjugates, (B) ceftriaxone-HSA conjugates, (C) ceftizoxime-HSA conjugates. The horizontal line represents the positive cutoff value derived from the mean + 3 SD of the absorbance value of the controls.

Fig. 2
Effects of FcεR1β-109T>C polymorphism on transcriptional activity in HMC-1 cells. Luciferase activity assay was performed in four independent experiments (total n = 12). Relative luciferase activity is represented as the ratio relative to luciferase activity in cells transfected with the empty control vector pGL3-basic.

Table 2
Comparison of the clinical characteristics of the subjects according to the presence of serum specific IgE and IgG to cephalosporin-HSA conjugate
References
1. Ye YM, Kim SH, Kim SH, Kim SH, Park HS. Genetic polymorphisms of ADRB2 and IL10 may be associated with the risk of IgE sensitization to digestive powders in exposed medical personnel. Int Arch Allergy Immunol. 2010. 153:193–200.
2. Choi IS, Han ER, Lim SW, Lim SR, Kim JN, Park SY, Chae SK, Lim HH, Seol YA, Bae YI, et al. Beta-lactam antibiotic sensitization and its relationship to allergic diseases in tertiary hospital nurses. Allergy Asthma Immunol Res. 2010. 2:114–122.
3. Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Occupational asthma and IgE sensitization in a pharmaceutical company processing cefteram pivoxil. Korean J Med. 2003. 64:309–316.
4. Yucesoy B, Johnson VJ. Genetic variability in susceptibility to occupational respiratory sensitization. J Allergy (Cairo). 2011. 2011:346719.
5. Guéant JL, Guéant-Rodriguez RM, Viola M, Valluzzi RL, Romano A. IgE-mediated hypersensitivity to cephalosporins. Curr Pharm Des. 2006. 12:3335–3345.
6. Aalberse RC, Schuurman J, van Ree R, Stapel S. IgG4 antibody assays in allergy diagnosis. Res Immunol. 1998. 149:263–266.
7. Moscato G, Vandenplas O, Van Wijk RG, Malo JL, Perfetti L, Quirce S, Walusiak J, Castano R, Pala G, Gautrin D, et al. EAACI position paper on occupational rhinitis. Respir Res. 2009. 10:16.
8. Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: prevalence, aetiology and determinants. Clin Exp Allergy. 2000. 30:1519–1534.
9. Shirakawa T, Li A, Dubowitz M, Dekker JW, Shaw AE, Faux JA, Ra C, Cookson WO, Hopkin JM. Association between atopy and variants of the beta subunit of the high-affinity immunoglobulin E receptor. Nat Genet. 1994. 7:125–129.
10. Qiao HL, Yang J, Zhang YW. Specific serum IgE levels and FceRIb genetic polymorphism in patients with penicillins allergy. Allergy. 2004. 59:1326–1332.
11. Rosenwasser LJ, Klemm DJ, Dresback JK, Inamura H, Mascali JJ, Klinnert M, Borish L. Promoter polymorphisms in the chromosome 5 gene cluster in asthma and atopy. Clin Exp Allergy. 1995. 25:74–78.
12. Apter AJ, Schelleman H, Walker A, Addya K, Rebbeck T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008. 122:152–158.
13. Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Heterogeneity of IgE response to cefteram pivoxil was noted in 2 patients with cefteram-induced occupational asthma. J Allergy Clin Immunol. 2003. 112:209–210.
14. Kim JE, Kim SH, Jin HJ, Hwang EK, Kim JH, Ye YM, Park HS. IgE Sensitization to cephalosporins in health care workers. Allergy Asthma Immunol Res. 2012. 4:85–91.
15. Kim SH, Bae JS, Holloway J, Lee JT, Suh CH, Nahm DH, Park HS. A polymorphism of MS4A2 (-109T>C) encoding the β-chain of the high-affinity immunoglobulin E receptor (FcεR1β) is associated with a susceptibility to aspirin-intolerant asthma. Clin Exp Allergy. 2006. 36:877–883.
16. Kim SH, Ye YM, Kim HM, Lee MK, Suh CH, Nahm DH, Park HS. Occupational allergy caused by inhalation of pancreatic extracts in the medical personnel and identification of the major allergens. Korean J Asthma Allergy Clin Immunol. 2007. 27:10–19.
17. Nakamura S. Studies on asthma bronchiale. 6. On the occupational allergy caused by pancreatin among pharmacists. Arerugi. 1971. 20:361–364.
18. Sastre J, Quirce S, Novalbos A, Lluch-Bernal M, Bombín C, Umpiérrez A. Occupational asthma induced by cephalosporins. Eur Respir J. 1999. 13:1189–1191.
19. Kim JE, Kim SH, Choi GS, Ye YM, Park HS. Detection of specific IgE antibodies to cefotiam-HSA conjugate by ELISA in a nurse with occupational anaphylaxis. Allergy. 2010. 65:791–792.
20. Tadokoro K, Niimi N, Ohtoshi T, Nakajima K, Takafuji S, Onodera K, Suzuki S, Muranaka M. Cefotiam-induced IgE-mediated occupational contact anaphylaxis of nurses: case reports, RAST analysis, and a review of the literature. Clin Exp Allergy. 1994. 24:127–133.
21. Verna N, Di Giampaolo L, Renzetti A, Balatsinou L, Di Stefano F, Di Gioacchino G, Di Rocco P, Schiavone C, Boscolo P, Di Gioacchino M. Prevalence and risk factors for latex-related diseases among healthcare workers in an Italian general hospital. Ann Clin Lab Sci. 2003. 33:184–191.
22. Donnay C, Denis MA, Magis R, Fevotte J, Massin N, Dumas O, Pin I, Choudat D, Kauffmann F, Le Moual N. Under-estimation of self-reported occupational exposure by questionnaire in hospital workers. Occup Environ Med. 2011. 68:611–617.
23. Hur GY, Koh DH, Kim HA, Park HJ, Ye YM, Kim KS, Park HS. Prevalence of work-related symptoms and serum-specific antibodies to wheat flour in exposed workers in the bakery industry. Respir Med. 2008. 102:548–555.
24. Wisnewski AV. Developments in laboratory diagnostics for isocyanate asthma. Curr Opin Allergy Clin Immunol. 2007. 7:138–145.
25. Hur GY, Koh DH, Choi GS, Park HJ, Choi SJ, Ye YM, Kim KS, Park HS. Clinical and immunologic findings of methylene diphenyl diisocyanate-induced occupational asthma in a car upholstery factory. Clin Exp Allergy. 2008. 38:586–593.
26. Mukai K, Obata K, Tsujimura Y, Karasuyama H. New insights into the roles for basophils in acute and chronic allergy. Allergol Int. 2009. 58:11–19.
27. Ishizaka A, Sakiyama Y, Nakanishi M, Tomizawa K, Oshika E, Kojima K, Taguchi Y, Kandil E, Matsumoto S. The inductive effect of interleukin-4 on IgG4 and IgE synthesis in human peripheral blood lymphocytes. Clin Exp Immunol. 1990. 79:392–396.
28. Thong BY, Tan TC. Epidemiology and risk factors for drug allergy. Br J Clin Pharmacol. 2011. 71:684–700.
29. Filon FL, Radman G. Latex allergy: a follow up study of 1040 healthcare workers. Occup Environ Med. 2006. 63:121–125.
30. Vandenplas O, Delwiche JP, Evrard G, Aimont P, van der Brempt X, Jamart J, Delaunois L. Prevalence of occupational asthma due to latex among hospital personnel. Am J Respir Crit Care Med. 1995. 151:54–60.
31. Haddi E, Charpin D, Tafforeau M, Kulling G, Lanteaume A, Kleisbauer JP, Vervloet D. Atopy and systemic reactions to drugs. Allergy. 1990. 45:236–239.
32. Hizawa N, Yamaguchi E, Jinushi E, Kawakami Y. A common FCER1B gene promoter polymorphism influences total serum IgE levels in a Japanese population. Am J Respir Crit Care Med. 2000. 161:906–909.
33. Gervaziev YV, Kaznacheev VA, Gervazieva VB. Allelic polymorphisms in the interleukin-4 promoter regions and their association with bronchial asthma among the Russian population. Int Arch Allergy Immunol. 2006. 141:257–264.
34. Dombrowicz D, Lin S, Flamand V, Brini AT, Koller BH, Kinet JP. Allergy-associated FcRbeta is a molecular amplifier of IgE- and IgG-mediated in vivo responses. Immunity. 1998. 8:517–529.
35. Nishiyama C, Akizawa Y, Nishiyama M, Tokura T, Kawada H, Mitsuishi K, Hasegawa M, Ito T, Nakano N, Okamoto A, et al. Polymorphisms in the Fc epsilon RI beta promoter region affecting transcription activity: a possible promoter-dependent mechanism for association between Fc epsilon RI beta and atopy. J Immunol. 2004. 173:6458–6464.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download