This article has been corrected. See "Erratum: Correction of Misspelling of Title and Author Affiliation" in Volume 27 on page 1607.
Abstract
This study was to evaluate the effect of additional brief counseling by a primary care physician on lifestyle modification of examinees after a periodic health examination. 1,000 participants of the 2007 Korean national health screening program were asked to note any variation in their health behavior after participating in the screening program. The degree of comprehensive motivation for lifestyle modification was assessed in terms of stages of health behavior change. We calculated odds ratio of positive change (enhanced stage of change) with multiple logistic regression analysis and age-adjusted proportion of positive changers. Of 989 respondents, 486 and 503 received the basic and additional programs, respectively. Additional group were more likely to be positive changer than basic group (adjusted OR 1.78; 95% CI 1.19-2.65), and this was more prominent in older age group (adjusted OR 2.38, 95% CI 1.23-4.58). The age-adjusted proportions of positive changers were 22.7% (95% CI, 17.9-28.3) and 36.2% (95% CI, 30.4-42.4) in the basic and additional groups, respectively (P < 0.001). The additional consultation led to improvements in the stage of health behavior change after the health examination. Thus, such a consultation should be considered when designing a health-screening program.
A periodic health examination (PHE) is a proven strategy for enhancing the delivery of many preventive health services at the population level (1). However, it has mixed effects on hospitalization cost, disability, mortality, and health habit and status (1). In contrast, lifestyle changes such as cessation of cigarette smoking, limited alcohol consumption, physical activity, and dietary modification have firm evidences to enhance the population health outcomes (2-5). Therefore, better health outcomes are expected if a PHE includes a brief intervention for lifestyle change.
Brief consultations with physicians or other professionals have a favourable effect on lifestyle modification (LSM). Even interventions as short as 3 min can significantly increase the cessation rate among smokers (6); similar results have been reported for insufficient exercisers (7, 8) and heavy drinkers (9). A brief consultation with a physician could motivate an examinee to modify their lifestyle and improve their health outcomes.
Given the benefit of health screening program and brief consultation of physician for health behavior, we could hypothesize synergistic effect of adding brief consultation using the results of health screening program. However, hardly any studies have been conducted to determine the effects of such consultations on the health outcomes after a PHE, especially at the population level.
The aim of this preliminary study was to determine the effect of additional brief counseling by a primary care physician on LSM by examinees after a PHE.
The Republic of Korea Government has conducted a national screening program since 1980. And the Korean Ministry of Health and Welfare launched the New National Screening Program for the Transitional Ages in Korea in April 2007 to tailor program according to age and gender and strengthen post-examinational follow up. In this program, specific examinations were conducted according to gender and age; the program also involved on-demand additional counseling for those with a poor lifestyle.
As part of the 2007 Program, the Korean National Health Insurance Corporation (KNHIC) sent a letter to inform each respondent about the screening program. When respondents visited a hospital, they entered a basic program. They answered the questionnaire about lifestyle and past medical histories. Examinations consisted of body measurements (height, weight, waist circumference, and blood pressure), blood sampling (blood sugar, cholesterol, and some liver or renal function tests), and radiological examinations (dual-energy X-ray absorptiometry [only for 66-yr-old women] and chest radiograph). Following all examinations, each hospital prepared a formal report on the examination results and a health risk appraisal (HRA). Those with higher HRA scores were prompted to enter an additional program for LSM by visiting a nearby primary care physician licensed for counseling after 3 hr of training, which consisted of contents and process of this program, interpretation of results of HRA, the way to use HRA for consultation, concept of stage of change and interventional strategy. The National Screening Program for the Transitional Ages in Korea was described in detail elsewhere (10).
Those who had higher HRA scores were informed that they could receive additional brief counseling. Every participant of basic program could choose whether they received this additional brief counseling of their own accord. Additional brief counseling consisted of 4 phase: physician's consultation about result of basic program, consultation about health behavior, consultation about mental health (especially for depression), recheck of blood pressure and blood glucose level to confirm diagnosis of hypertension and diabetes mellitus.
In the second phase of additional brief consultation, there were five domains of consultation; cigarette smoking, alcohol drinking, regular exercise, nutrition and obesity. In the consultation, examinees were informed of their cardiovascular health risk according to HRA scores, educated on relationship of five domains and their risk, assessed the motivation of health behavioral change, recommended health behavior change and suggested useful method for the change with provision of education material.
Overall, this brief counseling was expected to take 10 min for a person.
We received a list, in order of acceptance, of the 4,000 respondents who already finished this New Korean Health Screening Program for people in transition from the KNHIC. This list included 2,000 basic program participants and 2,000 additional program participants, with equal numbers of participants aged 40 and 66 yr (1,000 for each age). All listed participants were informed that they were candidate for telephone survey in advance.
A one-to-one telephone survey was conducted from August 7 to 13, 2007, by a professional survey institute (i.e., the telephonic survey team of the Korea Institute for Health and Social Affairs). Thirteen interviewers who received 3 hr of instruction about the new national program and the contents of the survey performed this telephonic survey. During each call, after explaining the purpose of the study and receiving verbal informed consent from the participants, the interviewers progressed to the main survey. The respondents were contacted consecutively in order of Korean alphabetical of their names, and the survey was planned to be conducted until 1,000 respondents agreed to participate survey (500 for basic program group and 500 for additional program group). Finally, we contacted 999 respondents of basic program participants and 996 respondents of additional program, and 1,000 of them (500 for each group) agreed to participate in telephonic survey. We excluded 10 respondents with misclassified data from 1,000 responses. And finally we included 989 responses in analysis (486 for basic program and 503 for additional program).
The degree of comprehensive motivation for LSM was assessed according to six stages of change (11): precontemplation, contemplation, preparation, action, maintenance, and termination. To improve the respondents' understanding, the definition of stage of change was modified to simpler expressions - action and maintenance, already; preparation, sooner or later; contemplation, someday; precontemplation, no plan - because half of the respondents were too old to understand the actual definition.
We gathered the following information from the questionnaire of the screening program: sociodemographics (age, sex), lifestyle (cigarette smoking, alcohol drinking, physical activity), and medical and family histories (stroke, coronary heart disease, diabetes, hypertension, dyslipidaemia, obesity, and abdominal obesity). The National Health Insurance premium was used as a surrogate marker of household income, because it is proportional to each individual's assets. And we gathered results of physical examination and laboratory tests from data of basic program.
And we gathered the following information from the telephone survey: general satisfaction with health screening program, degree of understanding the results of screening, stage of change, reason for not receiving additional brief counseling (for basic group), length of time of counseling (for additional group), understanding contents of counseling (for additional group).
In terms of the smoking status, the respondents were classified as current smoker, ex-smoker, or non-smoker. Further, an at-risk alcohol drinker was defined as a 40-yr-old man who drank more than 14 drinks per week or four drinks per occasion, or a 66-yr-old man or woman who drank more than seven drinks per week or three drinks per occasion (12). Physical activity was categorized by weekly counts of physical activity episodes such as brisk walking (> 30 min/day), moderate-intensity activity (> 30 min/day), and vigorous activity (i.e., > 20 min/day). If the sum of these episodes was five or more, the physical activity was regarded as adequate. Obesity (BMI ≥ 25) and abdominal obesity (≥ 90 cm in men and ≥ 85 cm in women) were defined according to the Korean obesity criteria (13).
If participants answered they took medications for hypertension, diabetes mellitus or hypercholesterolemia, they were considered to have the diseases. And if their systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, they were considered to have hypertension. If their serum fasting glucose level ≥ 126 mg/dL, they were considered to have diabetes mellitus. If their serum total cholesterol level ≥ 240 mg/dL, they were considered to have hypercholesterolemia.
To describe the characteristics of the respondents, we used simple frequency and its percentage, mean, and standard deviation (SD). The chi-square test was used to compare the characteristics of the program groups. To elucidate a shift in the stage of change in both program groups, the difference in the proportions of respondents before and after the program was calculated and compared with the chi-square test for each stage.
We performed univariate analysis to evaluate the association between 'positive change', which was defined as shift in the stage of change toward action and maintenance, and each variable by using the chi-square test and t-test according to the variables. Thus 'positive changer' was defined as participant who showed one or more step shift of stage of change from baseline stage to direction to action and maintenance. In the analysis, we tested the sociodemographic variables, health-related lifestyles (cigarette smoking, alcohol drinking and physical activity), and chronic disease (hypertension, diabetes mellitus, hypercholesterolemia and obesity). Then, we performed multiple logistic regression analysis to elucidated association of additional brief counseling with a shift in stage of change, adjusted for variables significant in univariate analysis.
We used Stata 11.2 for all statistical analyses and set the significance level at P < 0.05, except for univariate analysis where we set the significance level at P < 0.10 to prevent missing potential confounder in multivariate analysis.
Of the 989 respondents, 40% (396/990) were male, and 51% (505/989) were 40 yr old. There were 486 (49.1%) and 503 (50.9%) respondents in the basic and additional program groups, respectively. Initially, 49.0% (238/486) of the basic program respondents and 43.7% (220/503) of the additional program respondents were in the action/maintenance stage, without significant differences in the stages of change between the groups (P = 0.262). The additional program group included more male (35.8% vs 44.0%) and obese respondents (33.8% vs 40.7%) than the basic program group (P = 0.011 and 0.044, respectively). Two thirds of participants of additional program answered they were counselled within 10 min, and three quarters of them answered that they understood the counseling well (Table 1).
Proportion of positive changer was not different between different elapsed time from screening program to telephone survey. Proportion of positive changer according to elapsed time was 41.0% for less than 1 month, 42.6% for 1-2 months, 39.8% for 2-3 months, and 40.0% for over 3 months (P = 0.71).
Approximately 60% of the basic program group and 70% of additional program group were in the action/maintenance stage after the program, showing increases of 10% (50/486) and 27% (135/503), respectively. Although the proportion of respondents in the preparation stage was unremarkable, those in the contemplation and precontemplation stages significantly decreased (-5.5% and -8.6% in the basic program group and -12.9% and -14.3% in the additional program group, respectively).
The proportions of stages of change were significantly different before and after the program in both of two program groups (P < 0.001) (Table 2).
Younger age group was more likely to be a positive changer than older age group (P < 0.001), and physically active persons were more motivated than inactive persons (P < 0.001). If persons were hypertensive, they were less likely to be positive changer (P=0.047). In contrast, there was a tendency that a person having hypercholesterolemia tended to be positive changer (P=0.069). In addition, persons in precontemplation stage had a tendency to be positive changer (P=0.063).
However sex, national insurance premium, cigarette smoking, alcohol drinking, diabetes mellitus and obesity were not associated with shift in stage of change (all P>0.10).
Among participants of additional program, understanding of counseling was associated with shift in stage of change significantly (P=0.001), but counseling time did not show such association (Table 3).
From the results of univariate analysis, sex, physical activity, hypertension, hypercholesterolemia and baseline stage of change were included in multiple logistic regression analysis as adjustment variables.
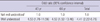
For participants of 40 yr, about 59% of increase of positive changer was observed in additional brief counseling group, but it became statistically insignificant after adjustment (unadjusted odds ratio 1.59, 95% CI 1.11-2.26; adjusted odds ratio was 1.45, 95% CI 0.86-2.46). And for participants of 66 yr, chance to be positive changer was doubled (unadjusted odds ratio 1.96, 95% CI 1.29-2.96; adjusted odds ratio was 2.38, 95% CI 1.23-4.58). For whole participants, over 60% of increase was observed (unadjusted odds ratio 1.68, 95% CI 1.29-2.19; adjusted odds ratio 1.78, 95% CI 1.19-2.65) (Table 4).
The proportions of positive changers adjusted for sex and significant variables in the univariate analysis were calculated according to age for both program groups. There was a marginal difference in the adjusted proportion of 40-yr-old positive changers (adjusted proportion 0.355, 95% CI 0.278-0.440 vs adjusted proportion 0.458, 95% CI 0.375-0.544; P=0.088) and a significant difference in the adjusted proportion of 66-yr-old positive changers (adjusted proportion 0.114, 95% CI 0.070-0.179 vs adjusted proportion 0.274, 95% CI 0.200-0.362; P<0.001) between the basic and the additional program groups. A similar finding was observed when both age groups were considered together (adjusted proportion 0.227, 95% CI 0.179-0.283 vs adjusted proportion 0.362, 95% CI 0.304-0.424, P<0.001) (Fig. 1).
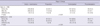
Over 4 fold increase of positive changer was observed for participants who answered they understood the counseling well compared to others (aOR 4.41, 95% CI 2.22-8.75). This finding was observed regardless of age groups (Table 5).
We sought to determine whether additional consultation with a primary care physician during a PHE has favourable effects on patient LSM. Both the basic and the additional program groups showed positive shifts in the stages of change. However, the proportion of respondents taking a real action (action/maintenance stage) was higher in the additional program group. After adjustment, positive changers were more frequently observed in the additional program group, especially in older age group. This result suggests that a brief intervention by a primary care physician has a beneficial impact on LSM. And positive change was more elevated when counsellee understood the counseling.
Previous studies showed that brief counseling by a primary care physician is an effective method to change the counselee's lifestyle: brief counseling could reduce cigarette smoking (6) and alcohol consumption (9), and increase physical activity (7, 8). The current study provides evidence that brief counseling by a primary care physician has an additional benefit when it is combined with a PHE compared with a PHE alone. However, primary care physicians have doubted the effectiveness of health promotion and lifestyle counseling, despite they were positive about doing them (14). Education and training for effectiveness of lifestyle counseling should be given to primary care physicians because they are ideally placed for this role.
Although a previous study showed that a PHE with a health consultation is a cost-effective and valid strategy to manage poor lifestyles or lifestyle diseases (15-17), Engberg and colleagues reported no beneficial effects of the addition of a 45-min health consultation to a PHE on the cardiovascular risk score after 5-yr follow-up (18). In their study, however, follow-up consultation for the intervention group was provided only annually and health screening was performed only once, at the time of enrollment. Another study showed that the effect of counselling on motivational readiness observed at 6 weeks after consultation disappeared at 8 months after consultation (19). Thus, a closer follow-up and intervention would be needed to maintain a long-term effect of an additional consultation on the motivation for LSM, in turn leading to long-term improvement in health outcomes such as life-year gain. This assumption is supported by the result of a study in which weekly telephonic counselling for 3 months after brief advice, compared with brief advice only, increased participation in physical activity at 3 and 6 months (20).
The stage of change shifted in a positive direction in both program groups, although suggesting that a PHE itself is effective to enhance lifestyle modification. After a systematic review of five randomized clinical trials, Boulware et al. concluded that a PHE has a mixed effect on health habits (1); however, these randomized clinical trials were performed from 1967 to 1989, and some were performed before contemporary clinical guidelines such as those of the US. Preventive Services Task Force were available. Thus, the implication of their result to the current clinical situation is limited, and further study of this issue is needed.
Even without a difference in the baseline stage of change between the program groups, a greater positive shift was observed in the additional program group. Further, after the program, the proportion of respondents in the action/maintenance stage, which could be assumed as taking a real action, was much higher in the additional program group. Thus, an additional consultation is an effective cue to action. According to the Health Belief Model, cues to action are strategies to activate readiness and consist of education, symptoms, and media information (20). Post-examinational consultation is a method of education: it could make a counselee perceive the threat of disease and then raise the likelihood of behavioral change.
A previous study showed that patients with diabetes older than 65 yr are more likely to adhere to physicians' advice about hypertension-related LSM (21). In this study, we observed a similar finding. Although the proportion of positive changers was less among the 66 yr olds than among the 40 yr olds, the 66 yr olds showed a greater effectiveness of additional program, suggesting that the addition of a lifestyle consultation to a PHE is more effective among the elderly.
Our finding showed that when counsellee understood the counselling, they were more likely to be positive changer, although time consumed did not show such association. This implies that quality of counselling could be more important factor than the quantity. Future research using sophisticated index of quality of counselling is needed to confirm this finding.
This study has some limitations. First, we retrospectively collected information about the stages of change before and after the program; this information was dependent on the respondents' memory. Thus, the possibility of recall bias cannot be excluded. However when it is considered that interval between screening program and telephone survey did not affect the proportion of positive changers, recall bias might influence the results minimally at best. Second, the respondents were limited to those who participated in the 2007 national health-screening program. Thus, generalizability could be limited to a more motivated population for health promotion. Third, because we assessed the short-term effect of lifestyle intervention on the stage of change by the participants' response, we could not evaluate the effect on an actual change or health outcome.
Despite these limitations, we found that the addition of a brief consultation for LSM to a PHE is effective to shift the stage of change in a positive direction. The results of this study should be confirmed by a longitudinal study with direct measurements of actual actions and health outcomes over a long period.
Additional brief consultation by a primary care physician after a PHE has a beneficial effect on the stage of change for lifestyle modification. Thus, brief medical counselling after a health examination should be considered for designing a health-screening program.
Figures and Tables
 | Fig. 1Age-adjusted proportion of positive changers in the basic and additional program groups. *Adjusted for age, sex, hypertension, hypercholesterolemia, physical activity level, baseline stage of change (age was adjusted only in total). |
Table 3
Association of shift in stage of change with sociodemographic, health risk factors and chronic diseases variables in univariate analysis

Table 4
Association between additional brief counseling and shift in stage of change in multivariate analysis
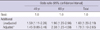
Table 5
Association between understanding of brief counselling and shift in stage of change among participants of additional program in multivariate analysis
*Adjusted for sex and variables significant in univariate analysis; physical activity, hypertension, hyperlipidemia and baseline stage of change (age was adjusted for total); †Categories of 'partially understood' and 'not understood' were combined, because there was no observation of positive changer in 'not understood'.
ACKNOWLEDGMENTS
We thank the staff of the Ministry for Health and Welfare, and the Korean National Health Insurance Corporation for their cooperation.
References
1. Boulware L, Marinopoulos S, Phillips K, Hwang C, Maynor K, Merenstein D, Wilson R, Barnes G, Bass E, Powe N. Systematic review: the value of the periodic health evaluation. Ann Intern Med. 2007. 146:289–300.
2. Anthonisen N, Skeans M, Wise R, Manfreda J, Kanner R, Connett J. The effects of a smoking cessation intervention on 14.5-year mortality. Ann Intern Med. 2005. 142:233–239.
3. Camacho T, Kaplan G, Cohen R. Alcohol consumption and mortality in Alameda county. J Chronic Dis. 1987. 40:229–236.
4. Paffenbarger R, Hyde R, Wing A, Hsieh C. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986. 314:605–613.
5. Knoops K, de Groot L, Kromhout D, Perrin A, Moreiras-Varela O, Menotti A, van Staveren W. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: The HALE project. JAMA. 2004. 292:1433–1439.
6. US Public Health Service. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A US Public health service report. Am J Prev Med. 2008. 35:158–176.
7. Marki A, Bauer G, Angst F, Nigg C, Gillmann G, Gehring T. Systematic counselling by general practitioners for promoting physical activity in elderly patients: a feasibility study. Swiss Med Wkly. 2006. 136:482–488.
8. Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: the activity counseling trial: a randomized controlled trial. JAMA. 2001. 286:677–687.
9. Whitlock E, Polen M, Green C, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US preventive services task force. Ann Intern Med. 2004. 140:557.
10. Kim H, Shin D, Lee W, Kim Y, Cho B. National screening program for transitional ages in Korea: a new screening for strengthening primary prevention and follow-up care. J Korean Med Sci. 2012. 27:S70–S75.
11. Prochaska J, DiClemente C. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983. 51:390–395.
12. U.S. Department of Health & Human Services. National Institutes of Health. National Institute on Alcohol Abuse and Alcoholism. Helping patients Who Drink Too Much: A Clinician's guide. 2005. Available in: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf.
13. Lee S, Park H, Kim S, Kwon H, Kim D, Kim D, Cho G, Han J, Kim S, Park C. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J Obes. 2006. 15:1–9.
14. McAvoy BR, Kaner EF, Lock CA, Heather N, Gilvarry E. Our healthier nation: are general practitioners willing and able to deliver? A survey of attitudes to and involvement in health promotion and lifestyle counselling. Br J Gen Pract. 1999. 49:187–190.
15. Rasmussen SR, Thomsen JL, Kilsmark J, Hvenegaard A, Engberg M, Lauritzen T, Sogaard J. Preventive health screenings and health consultations in primary care increase life expectancy without increasing costs. Scand J Public Health. 2007. 35:365–372.
16. Fleming MF, Manwell LB, Barry KL, Adams W, Stauffacher EA. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999. 48:378–384.
17. van der Veen J, Bakx C, van den Hoogen H, Verheijden M, van den Bosch W, van Weel C, van Staveren W. Stage-matched nutrition guidance for patients at elevated risk for cardiovascular disease: a randomized intervention study in family practice. J Fam Pract. 2002. 51:751–758.
18. Engberg M, Christensen B, Karlsmose B, Lous J, Lauritzen T. General health screenings to improve cardiovascular risk profiles: a randomized controlled trial in general practice with 5-year follow-up. J Fam Pract. 2002. 51:546–554.
19. Goldstein MG, Pinto BM, Marcus BH, Lynn H, Jette AM, Rakowski W, McDermott S, DePue JD, Milan FB, Dube C, et al. Physician-based physical activity counseling for middle-aged and older adults: a randomized trial. Ann Behav Med. 1999. 21:40–47.
20. Pinto BM, Goldstein MG, Ashba J, Sciamanna CN, Jette A. Randomized controlled trial of physical activity counseling for older primary care patients. Am J Prev Med. 2005. 29:247–255.
21. Egede LE. Lifestyle modification to improve blood pressure control in individuals with diabetes: is physician advice effective. Diabetes Care. 2003. 26:602–607.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download