Abstract
We investigated the livebirths prevalence and occurrence pattern of birth defects in Korea. After the survey on birth defects was done in 2,348 medical institutions around the nation, the birth defect prevalence of livebirths in 2005-2006 was calculated. This study was based on the medical insurance claims database of the National Health Insurance Corporation. The number of livebirths in Korea was 883,184 from 2005-2006, and 25,335 cases of birth defects were notified to our study, equivalent to a prevalence of 286.9 per 10,000 livebirths. Anomalies of the circulatory system were the most common defects, accounting for 43.4% of birth defects with a prevalence of 124.5 per 10,000 livebirths. It was followed by the musculoskeletal system anomalies, the digestive system anomalies, and the urinary system anomalies. The five major birth defects based on the ranking of prevalence were atrial septal defect, ventricular septal defect, hydronephrosis, patent ductus arteriosus, and cleft lip/palate. Birth defects in livebirths were associated with a high proportion of low birthweight, prematurity, multiple births and advanced maternal age. The prevalence of birth defects in Korea is similar to or lower than those reported in developed countries. Our study suggests baseline data to explain the current status of birth defects and to establish a registry system of birth defects in Korea.
Birth defects are defined as structural abnormalities, sensory changes, chromosomal abnormalities, metabolic abnormalities and neurodevelopmental defects that are present at birth and remain an important public health issue because they are a main cause of fetal and infant mortality and lifelong disabilities. Birth defects are known to occur due to single gene defects, chromosomal abnormalities, environmental factors and multifactorial causes following reciprocal effects of environmental and genetic factors, but causes of 60%-70% of defects have not been determined (1). Birth defects occur in 2%-3% of all births (2-5), and 25% of severe birth defects are multiple defects. Severe birth defects account for 20%-25% of perinatal mortality (2-4), and the prevalence of birth defects is much higher in abortion or stillbirth (6, 7).
Developed countries have examined prevalence of birth defects through registration or surveillance system of fetuses and infants with birth defects since the 1970s and have taken effective management measures based on the collected data. In addition, establishment of international organizations have led to an active comparison of prevalence of major birth defects according to countries and regions and an active search for preventive measures by sharing information.
In Korea, however, although medical costs for some urgent birth defects are financially supported considering that over 20% of infant mortality is caused by birth defects, statistics showing overall occurrence and prevalence of birth defects are still insufficient. Reported birth defects prevalence has varied considerably, and differences may be because of racial and geographical factors, definition of birth defects, accuracy and sources of data, examination time and performance of autopsy.
This study aimed to elucidate the current status of birth defects in Korea by investigating its prevalence and occurrence patterns. It is hoped the results of this study will contribute to the establishment and promotion of related policies and support efforts to minimize the burden caused by birth defects.
This study was conducted by utilizing data about infants with at least one birth defect, delivered between 2005 and 2006, from the congenital anomaly survey performed by the Korea Institute for Health and Social Affairs. These data were based on the medical insurance claims database of the National Health Insurance Corporation on medical institutes across the country. In this study, the research categories and research subjects were selected beforehand, and a web-based research system was operated for the efficient collection of data. While the research was ongoing, the progress status was monitored in real time, and thus, the researchers were able to respond to needs and problems that arouse at the research site. The collected data from the research was reviewed to make up for the weak points, and the data were aligned in regards to the differences or overlap in diagnoses between medical institutions. By adding the 2005-2006 infant and maternal mortality survey, the birth defects prevalence of livebirths and stillbirths in 2005-2006 was calculated. As the time for diagnosis of birth defects is different according to disease, international birth defect surveillance organizations, such as the International Clearinghouse for Birth Defects Surveillance and Research (ICBDSR) and the European Surveillance of Congenital Anomalies (EUROCAT), have been reporting general statistics including diagnosis to postnatal one year. This study also contains the diagnosis made to postnatal one year. The Korean Medical Record Association reviewed the progress of investigation and directly collected the birth defects database.
Birth defects were categorized by birth defect group (the system affected), subtype (the individual disease) according to the 10th Revision of the International Classification of Diseases (ICD-10) and were investigated by including major groups of birth defects managed by EUROCAT, ICBDSR, and the National Birth Defects Prevention Network (NBDPN), which play leading roles internationally in this area.
In this study, we analyzed the medical insurance claims database including birth defects diagnosis during the first year after birth (referring to the main disease code and sub-code) to obtain information regarding study subjects in advance and investigate risk factors for birth defects that could be determined from medical records. Most importantly, data on the same disease in the same patient from various institutions were collated and reviewed. The possibility that birth defects could occur in combination in the same patient was considered; particularly, birth defects of the circulatory system were classified into the complex disease group (a maximum of three diseases) by a pediatric cardiologist. However, the major disease of the three was the main focus of the investigation. Because of the tendency of birth defects to be serious and chronic, cases of minor anomalies (Q32.0, Q67.0-Q67.8, Q68.0, Q68.3-Q68.5, Q76.0, Q76.5, Q82.5, Q83.3, Q84.5, Q95.0, Q95.1) treated as outpatients were excluded.
According to the above standards, there were 38,396 selected study subjects from 2,505 medical institutions. When these results were organized based on the affiliation status of the medical institutions, there were 38,199 study subjects from 2,348 medical institutions. When reconfirmation of diagnoses, rule-out diagnoses, and diseases name were done on the individual diagnosis of the study subjects, 32,727 of them were diagnosed with or suspected of one or more birth defects. In addition, from these, cases with rule-out diagnoses of birth defects and inappropriate cases were excluded. Moreover, since complex diseases frequently arise from anomalies of the circulatory system, with the help of a pediatric cardiologist, the study subjects were categorized into complex disease groups with a maximum of three diseases with the main disease as the center. Therefore, the final number of study subjects selected for analysis from patients born from 2005 to 2006 was 25,335 (Fig. 1).
As birth defects occur during intrauterine life, it is important to include stillbirths and abortions in birth defects statistics with total livebirths as a denominator. However, birth defects can be eliminated through spontaneous abortion in the early stage of pregnancy, so it is thought to be nearly impossible to determine a truly accurate birth defects total including abortions, stillbirth, and livebirths (denominator) in pregnant women for the same period.
Therefore, this study calculated livebirths prevalence of birth defects by dividing the number of livebirths with birth defects by the total number of livebirths and birth defects prevalence was measured with 10,000 livebirths as a standard.
We used the Poisson distribution to calculate 95% confidence intervals of birth defects prevalence. Variables collected for analysis were maternal and paternal age, occupation of parents, educational background and pregnancy-related factors such as gestational age, birthweight, fetal gender, and plural pregnancy.
The number of livebirths in Korea was 883,184 from 2005-2006, with 435,031 in 2005 and 448,153 in 2006. The number of infants with birth defects was 25,335 in 2,348 medical institutions. Baseline demographic characteristics of total livebirths and birth defects in 2005-2006 are presented in Table 1. Data on paternal age, educational background and parents' occupation were not analyzed due to high non-response rates.
In addition, the total number of stillbirths in 2005-2006 was 5,079, and out of those, 640 had birth defects. Therefore, the total number of birth defects among total livebirths and stillbirths was 25,975 in 2005-2006. However, only the live birth prevalence of birth defects was analyzed in our study due to lack information on stillbirths in our dataset.
The prevalence of birth defects was 286.9 per 10,000 livebirths in 2005-2006. Anomalies of the circulatory system were the most common defects, accounting for 43.4% of all birth defects and its prevalence per 10,000 livebirths was 124.5. The next most common defects were musculoskeletal system anomalies (53.1 per 10,000 livebirths, 18.5%), digestive system anomalies (33.0 per 10,000 livebirths, 11.5%) and urinary system anomalies (27.5 per 10,000 livebirths, 9.6%) (Table 2). Atrial septal defect (ASD) was the most common birth defect of the circulatory system, with a prevalence of 66.6 per 10,000 livebirths. The prevalence of congenital hypertrophic pyloric stenosis was also high (8.6 per 10,000 livebirths, 3.0%) among digestive system anomalies. The obstructive genitourinary defect was the most common urinary system anomaly (21.5 per 10,000 livebirths, 7.5%), followed by congenital hydronephrosis (16.7 per 10,000 livebirths, 5.8%) and cystic kidney (3.3 per 10,000 livebirths, 1.2%). Polydactyly was the most common musculoskeletal system anomaly. Its prevalence was 10.9 per 10,000 livebirths. The prevalence of nervous system anomalies was 9.5 per 10,000 livebirths. Spina bifida was the most common birth defect of the nervous system, with a prevalence of 2.6 per 10,000 livebirths.
The occurrence of multiple birth defects is associated with the stage of embryonic development for each organ. Table 3 shows birth defects prevalence according to the number of birth defect types involved. Prevalence of single birth defects was 235.2 per 10,000 livebirths, accounting for 82% of all birth defects. The prevalence of two and three or more defects was 40.7 (14.2%) and 11.1 (3.9%) per 10,000 livebirths, respectively.
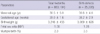
The five major birth defects based on the ranking of prevalence were atrial septal defect (66.6), ventricular septal defect (38.4), hydronephrosis (16.7), patent ductus arteriosus (14.4) and cleft lip/palate (11.1). In particular, the prevalences of atrial and ventricular septal defects were more than two times higher than those of other defects (Table 4).
Birth defects in livebirths were associated with a high proportion of low birthweight, prematurity, multiple births and advanced maternal age, which are high-risk populations in maternal and child health (Fig. 2). The prevalence of birth defects among premature infants in 2005 and 2006 tended to be 3.2 times higher than that of infants more than 37 weeks of gestational age. The prevalence of birth defects was 1.7 times higher in multiple births than in singletons. The prevalence of birth defects in infants with low birthweight was 3.5 times higher than that of normal birthweight infants. The prevalence of birth defects according to maternal age was 1.1 times higher in mothers ≥35 yr of age than in mothers <35 yr of age. There were significant differences in the prevalence of circulatory system anomalies and chromosomal abnormalities between maternal age 35 yr or older and less than 35 yr. Also, our study indicated that all birth defect groups was associated with preterm delivery (Table 5).
The prevalence of chromosomal anomalies was 6.3 per 10,000 livebirths in 2005-2006. Down syndrome was the most common chromosomal anomaly and its prevalence was 3.7 per 10,000 livebirths, accounting for 1.3% of all birth defects (Table 6).
The prevalence of birth defects in Korea was similar to or somewhat lower than those of the compared countries (Table 7). Down syndrome prevalence (3.7 per 10,000 livebirths) in Korea was especially lower than in Japan (10.57 per 10,000 livebirths) and the United States (13.56 per 10,000 livebirths), which may reflect terminations of pregnancy after prenatal diagnosis of Down syndrome.
Since the importance of birth defects was recognized in the 1960s, studies have been done to determine its prevalence. However, since most of the studies were limited to a single institute or region and not nationwide, birth defects prevalence varied widely from 0.5% to 6.8% (8, 9). In this study, we investigated the prevalence and occurrence pattern of birth defects in Korea.
The reported frequency of birth defects has been 2%-3% (2-5). The prevalence of birth defects in Korea found in this study was 286.9 per 10,000 livebirths, which was similar to previous studies. Among all birth defects studied, the prevalence of circulatory system anomalies was 124.5 per 10,000 livebirths (43.4%) followed by anomalies of the musculoskeletal system, digestive system, and urinary system. Kang et al. (8) reported the prevalence of birth defects was highest in the genitourinary system followed by the central nervous and digestive system. McIntosh et al. (10) reported the order to be the musculoskeletal, integumentary, and central nervous system, while Hong et al. (11) reported the order to be the musculoskeletal, digestive, and genitourinary system. The fact that reported frequencies vary may be due to the variety and subjectivity of classification criteria, whether or not autopsy was carried out, and differences in diagnostic ability. It is generally considered that the proportion of multiple birth defects is 20%-30% (12), but the proportion was 18.0% in this study.
We compared Korean birth defects prevalence with that of countries that reported data produced under similar criteria through ICBDSR and NBDPN, and the results showed that it was similar to or lower than those of the compared countries. The prevalence of Down syndrome was particularly low in Korea, which may be because of terminations of pregnancy after prenatal diagnosis. The prevalence of cleft lip/palate was similar to or somewhat lower than that of the compared countries (13-15).
The difference in statistical reports of birth defects frequency is due to differences in race, environmental factors, data collecting methods, time and method of birth defects diagnosis, whether or not autopsy was carried out after death of the newborn infants, and so on. In particular, it is assumed that many of the internal birth defects that can be discovered by means of autopsy are missed since autopsies of stillborn infants are performed less frequently in Korea than in other countries.
According to our study, the prevalence of birth defects was higher in high-risk populations of the maternal and child health, such as low birthweight, prematurity, multiple births and advanced maternal age. The relationship between maternal age and the prevalence of birth defects has been discussed in several studies. Schull (16) reported that the prevalence of birth defects increased as maternal age increased and, especially, the occurrence of Down syndrome was closely related to advanced maternal age. Hook (17) reported that the prevalence of significant cytogenetic abnormalities increased with maternal age and significantly contribute to the overall rate at the older ages. Although high-risk pregnancy is not determined only by maternal age, maternal age is significant because the prevalence of chronic diseases increases as maternal age increases.
Additionally, our study showed that the prevalence of birth defects was high in cases where the birthweight was less than 2,500 g or the gestation age was less than 37 weeks. The prevalence of birth defects among low birthweight and normal birthweight infants was 8.7% and 2.4%, respectively, indicating that the frequency was higher in low birthweight infants. This result is in line with the results of two previous studies conducted by Choi et al. and Park and Lee, respectively (18, 19). In the former study, the prevalence of birth defects among low birthweight and normal birthweight infants was 1.9% and 0.5% while it was 8.14% and 1.62% in the latter study.
Based on this result, it is assumed that the high prevalence may also be related to intrauterine growth retardation and preterm birth caused by birth defects. In addition, Tanner et al. (20) reported that the risk of congenital heart defect was 2.4 times higher in premature infants than in mature infants. Purisch et al. (21) reported that the risk of childbirth at the 35th week or before was 3.2 times higher and the risk of childbirth at the 28th week or before was 4.8 times higher in the infants with birth defects.
However, this result only means that the prevalence of birth defects is highly related to the variables, but it does not mean that low birthweight or preterm birth is the cause of birth defects. Since the causes of low birthweight infants are similar to the causes of birth defects in general, it is reported that birth defects are highly related to the occurrence of low birthweight infants.
With respect to sex, the probability of birth defects is higher in males than in females in this study. Similarly, Marden et al. (4) showed the ratio of male to female infants was 58:42; and the ratio was 61:39 in the study by McIntosh et al. (10).
Systematic data gath ering and monitoring of birth defects started in 1958 in Birmingham, United Kingdom (22). Since then, the interest in birth defects has elevated worldwide: EUROCAT was founded and is working in Europe (23), and an extensive monitoring of birth defects has been carried out in the United States mainly by the Centers for Diseases Control and Prevention and other public health authorities in each state (12). On the contrary, a comprehensive monitoring system has not been established in Korea, not only on the national scale but also on the local scale. Although international monitoring of birth defects is actively performed as an effort not only to improve quality of life but also to reduce disease burden, Korea has not yet participated since the system to produce statistical data has not been established. Since birth defects are particularly affected by changes in the environment, international cooperation is required for effective prevention and management.
In this study, statistical analysis was not accurately carried out because it was focused on parturient women who had delivered infants with birth defects, and thus the comparison with parturient women who have delivered normal infants was not performed well. In addition, a careful analysis of medicine taken during pregnancy, mothers' occupation and living environment is required to investigate the correlation between environmental factors and birth defects, but most of the data lacked detailed records. Therefore, future studies are needed to make a more accurate and objective analysis.
Birth defects are the frequent cause of spontaneous abortion and death of newborn infants and are one of the three major causes of death in the perinatal period in addition to premature birth and birth injury (6). The proportion of birth defects in cases of death in the perinatal period will increase due to the development of intensive care for newborn infants. It is necessary to produce data periodically so that trends can be monitored for effective prevention and management of birth defects. This study is a nationwide investigation of birth defects in Korea which suggests baseline data to be helpful in understanding the current status of birth defects and in monitoring the occurrence pattern of birth defects.
Figures and Tables
Fig. 2
Proportion of birth defects according to birthweight, gestational age, maternal age, and plurality in Korea, 2005-2006. BW, birthweight; GW, gestational weeks.

Table 3
Prevalence of birth defects according to the number of different birth defect groups involved
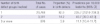
Table 4
Prevalence of major birth defect subtypes in Korea, 2005-2006

*Patent ductus arteriosus was excluded if birth weight was less than 2,500 g; †Undescended testis was excluded if gestational age was less than 36 weeks. CI, confidence interval; ASD, atrial septal defect; VSD, ventricular septal defect; PDA, patent ductus arteriosus; TOF, tetralogy of Fallot; CoA, coarctation of aorta.
References
1. Beckman DA, Brent RL. Mechanism of known environmental teratogens: drugs and chemicals. Clin Perinatol. 1986. 13:649–687.
2. Kalter H, Warkany J. Congenital malformations (second of two parts). N Engl J Med. 1983. 308:491–497.
3. Kalter H, Warkany J. Medical progress. Congenital malformations: etiologic factors and their role in prevention (first of two parts). N Engl J Med. 1983. 308:424–431.
4. Marden PM, Smith DW, McDonald MJ. Congenital anomalies in the newborn infant, including minor variations. a study of 4,412 babies by surface examination for anomalies and buccal smear for sex chromatin. J Pediatr. 1964. 64:357–371.
5. Pitkin RM. Screening and detection of congenital malformation. Am J Obstet Gynecol. 1991. 164:1045–1048.
6. Cordero JF. Finding the causes of birth defects. N Engl J Med. 1994. 331:48–49.
7. Chung CS, Myrianthopoulos NC. Congenital anomalies: mortality and morbidity, burden and classification. Am J Med Genet. 1987. 27:505–523.
8. Kang BH, Lee JG, Chung KH, Yang JB, Kim DY, Rhee YE, Noh HT. Incidence of congenital anomalies and diagnosis of congenital anomalies by antenatal ultrasonography. Korean J Obstet Gynecol. 2004. 47:2070–2076.
9. Kim SJ, Kim SP. Clinical study of the lethal anomalies by antenatal ultrasonogram. Korean J Obstet Gynecol. 1998. 41:1459–1464.
10. McIntosh R, Merritt KK, Richards MR, Samuels MH, Bellows MT. The incidence of congenital malformations: a study of 5,964 pregnancies. Pediatrics. 1954. 14:505–522.
11. Hong S, Lee B, Choi D, Yang Y. The clinical epidemiologic study of congenital anomalies in the newborn infants. Korean J Obstet Gynecol. 1986. 29:686–691.
12. Lynberg M, Edmonds L. Wilcox L, Marks J, editors. State use of birth defects surveillance. From Data to Action: CDC's public health surveillance for women, infants, and children. 1994. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health & Human Services.
13. International Clearinghouse for Birth Defects Surveillance and Research. Annual report 2008 with data for 2006. 2008. Rome, Italy: International Clearinghouse for Birth Defects.
14. International Clearinghouse for Birth Defects Surveillance and Research. Annual report 2007 with data for 2005. 2007. Rome, Italy: International Clearinghouse for Birth Defects.
15. Parker SE, Mai CT, Canfield MA, Rickard R, Wang Y, Meyer RE, Anderson P, Mason CA, Collins JS, Kirby RS, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010. 88:1008–1016.
16. Schull WJ. Congenital malformations: current knowledge of etiology. Clin Ostet Ginecol. 1961. 63:365–382.
17. Hook EB. Rates of chromosome abnormalities at different maternal ages. Obstet Gynecol. 1981. 58:282–285.
18. Choi J, Chun Y, Kim C, Woo B, Kang S. Congenital anomaly, 103 cases in a ten and half year period. Korean J Obstet Gynecol. 1978. 21:1025–1036.
19. Park M, Lee J. Clinical study of the congenital anomaly. Korean J Obstet Gynecol. 1986. 29:692–702.
20. Tanner K, Sabrine N, Wren C. Cardiovascular malformations among preterm infants. Pediatrics. 2005. 116:e833–e838.
21. Purisch SE, DeFranco EA, Muglia LJ, Odibo AO, Stamilio DM. Preterm birth in pregnancies complicated by major congenital malformations: a population-based study. Am J Obstet Gynecol. 2008. 199:287.e1–287.e8.
22. Knox EG, Lancashire R. Epidemiology of congenital malformations. 1991. London: Her Majesty's Stationery Office.
23. Lechat MF, Dolk H. Registries of congenital anomalies: EUROCAT. Environ Health Perspect. 1993. 101:Suppl 2. 153–157.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download