Abstract
Damselfish Chromis notata is a small fish less than 15 cm long and it is widespread in the Indo-Pacific Ocean. Of all the cases of fish bone foreign body (FBFB) disease at our hospital, a damselfish FBFB was very common, and a specific part of the bone complex was involved in the majority of cases. This study was performed to evaluate the clinical characteristics of damselfish FBFB in Jeju Island. We retrospectively reviewed the medical records from March 2004 to March 2011 for foreign body diseases. Among 126 cases of foreign body diseases, there were 77 (61.1%) cases of FBFB. The mean age ± standard deviation was 57.8 ± 12.7 yr, and this was higher in females 60.9 ± 14.6 yr vs 54.1 ± 8.7 yr. Damselfish was the most common origin of a FBFB 36 out of total 77 cases. The anal fin spine-pterygiophore complex of damselfish was most commonly involved and cause more severe clinical features than other fish bone foreign bodies; deep 2.7 ± 0.8 cm vs 2.3 ± 0.8 cm; P < 0.01, more common mural penetration 23/36 vs 10/41; P < 0.01, and longer hospital stay 12.6 ± 20.0 days 4.7 ± 4.8 days; P = 0.02. We recommend removing the anal fin spine-pterygiophore complex during cleaning the damselfish before cooking.
The most common cause of foreign body diseases is coins in children. However, in adults, this can vary in different localities and there are some differences among different nations. In Western countries, impacted meat was prevalent (1) and this could be associated with esophageal structural abnormalities. In Asian countries, fish bones were the most prevalent cause (2) and this seemed related to Asian's eating habits.
An esophageal fish bone foreign body (FBFB) is common among the people of Jeju Island because the local people enjoy eating fish. Among the fish, they especially like to eat the fish named locally as "Jari" or "Jaridom", the damselfish or coralfish Chromis notata, which is a less than a 15 cm sized small fish. It inhabits the inshore and offshore coral or rocky reefs from 2 to 15 m depth and this fish is distributed in the northwest Pacific, including southern Japan, Taiwan, China, and southern Korea, including Jeju Island (3).
During our medical practice, we found that the FBFBs of damselfish are common and caused by exclusively a specific part of the fish's skeleton. Therefore, we conducted this study to determine which the parts of the fish skeleton was involved and to evaluate the clinical characteristics of patients with a FBFB from damselfish.
We reviewed retrospectively the medical records, endoscopic photographs and radiologic findings of the patients who had endoscopic or surgical treatment for esophageal foreign body to find the rate of damselfish FBFB from March 2004 to March 2011 in Jeju National University Hospital. We collected the data on age and gender of the patients, the kinds of foreign body and the types of fish, the sizes and nature of the foreign bodies, the involved levels, the causative fish, the cooking recipes, evidence of mural penetration, the time delay from symptom onset to a hospital, and the admission durations.
The time delays between symptom onset and the hospital arrival were divided four groups as follows; within 24 hr, 48 hr, 72 hr, and over 72 hr. The types of fish bone were classified to four groups; linear bone, anal fin spine (AFS), skull bone and back bone according to the photographically assessed shapes. The skull bones included flat bones, jaw bones and gills. All the sharp and linear pin-like bones are grouped to the linear bones except AFS. The recipes were soup, hard-boiled, baked, sliced raw fish with sauce Jari mulhoe, salt-pickled, and steamed. Various Korean recipes that had a broth component were all classified to soup. The lodged sites were classified to four groups as 1) pharynx, 2) upper esophagus; the upper esophageal sphincter to 23 cm from the upper incisor, 3) mid esophagus; the aortic arch eminence to 31 cm from the upper incisor, and 4) lower esophagus; below the mid esophagus.
The simple X-rays and the computed tomography (CT) images were read by a radiologist. The CT findings were categorized to five groups; 1) those with negative finding, 2) visible fish bone without adjacent wall edema, 3) visible fish bone with adjacent wall edema, 4) visible mediastinal free air and 5) abscess and prominent mediastinitis.
Endoscopic evidence of pharyngeal and esophageal wall penetration was also evaluated. In the cases of surgical treatment without endoscopy, it was judged by the surgical records.
The monthly and yearly distributions of FBFB were also checked. Above procedures including reading the endoscopic photography and grouping the fish bones into different categories and judging the penetration were done by one person to reduce the interpersonal variation and to achieve consistency.
The statistical analyses were done using the SPSS for Windows (V. 13.0, SPSS, Chicago, IL, USA), and P values < 0.05 were considered to be significant. Descriptive statistics were used to summarize the characteristics of the cases and controls. Bivariate analysis was performed with chi-squared tests for the categorical variables and t-tests were used for the continuous variables as appropriate.
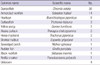
Our study included 126 cases of upper gastrointestinal foreign bodies: fish bones were most common and they were recorded in 77 cases 61.1%, meat in 26 cases 20.6%, other food material in 6 cases, chicken bones in 5 cases, drug in 4 cases; pills in 2, a press-through package in 2 and others in 8; nasogastric tube in 3, denture 2, tooth brush, sea shell and safety pin in one case each. The most common FBFB was damselfish and it accounted for 36 cases (46.8%). Others were armorclad rockfish in 14, houttuyn in 8, cutlassfish in 3, yellow porgy in 3, Alaska pollack in 2, horse mackerel in 2, unknown 4 and the others in 5 cases; shotted halibut, sawedged perch, rudder fish, black rockfish and redlip croaker in one case each (Table 1). The FBFB cases were common from April to August and they were most common in May, especially in damselfish FBFB case (Fig. 1).
The gender distribution was 35 men and 42 women in all the FBFB disease cases, and 16 men and 20 women for the cases of damselfish FBFB disease (Table 2). The mean age (mean ± standard deviation) was 57.8 ± 12.7 yr. The men were younger than the women 54.1 ± 8.7 for men and 60.9 ± 14.7 for women.
The time delays to hospital arrival were grouped as within 24 hr (n = 57), 48 hr (n = 10), 72 hr (n = 5), and over 72 hr (n = 4). Except for 1 case each in the latter two groups, the remaining 8 cases were damselfish FBFB. The longest time delay to hospital arrival were 5 days in two cases.
Simple X-rays were taken in 67 cases and 7 cases had overt evidence of FBFB disease sensitivity: 10.5%. Of these 7 cases, 6 cases were damselfish FBFB disease (P = 0.04). CTs were taken in 44 cases and 43 cases had positive findings (sensitivity 97.7%). The positive groups were classified to four subgroups: only a FBFB was detected in 25 cases, FB induced tissue edema was detected in 3 cases, positive free gas was detected in 11 cases, and abscess or mediastinitis was detected in 4 cases. Of the 11 cases with positive free gas findings, 10 cases were damselfish FBFB and 3 out of the 4 cases of the abscess or mediastinitis group were damselfish FBFB. Damselfish FBFB diseases had more serious findings on CT (P = 0.04).
The shapes of the FBFBs were categorized to four groups: 11 linear bones, 33 anal fin spine-pterygiophore complexes (ASPC), 29 skull bones and 4 spinal bones. Except for one case of a skull bone FB, 28 cases were from fish other than damselfish. Of the total 36 cases of damselfish FBFB, the ASPC was involved in 32 cases (88.9%) and it was the most common. The mean length of the FBFBs was 2.51 ± 0.81 cm; damselfish 2.73 ± 0.77 cm, other fish 2.33 ± 0.81 cm.
In the damselfish FBFB group, one recipe was soup, 7 were hard-boiled, 6 were baked, 5 were sliced raw fish with sauce, 8 were salt-pickled and 2 were steamed. Sliced raw fish with sauce and salt-pickled are relatively unique recipes for damselfish. In the other FBFB group, soup (n = 27) was most common recipe and the 2 hard-boiled and 4 baked. The most common recipes were soup in the total FBFB cases. There were remarkable differences in the recipes between damselfish and the other FBFB groups (P < 0.01).
The lodged sites for the total FBFBs were the pharynx in 22 cases (28.6%), the upper esophagus in 35 cases (45.5%), the mid-esophagus in 11 cases (14.3%) and the lower esophagus in 9 cases (11.7%). The most common site was the upper esophagus. There was no statistical significance in the foreign body lodged site between the damselfish and other FBFB groups (P = 0.11).
In 33 cases (damselfish 23, other fishes 10), endoscopic evidence of mural penetrations by the FBFB was noticed. Because the damselfish FBFBs were exclusively ASPC that had sharp points on both ends, both sides of pharyngoesophageal penetration were seen in 14 cases of damselfish FBFBs, compared to 2 cases of other FBFBs (P < 0.01).
Among the 77 cases of FBFB disease, 75 cases were treated by endoscopy and the remaining two cases were surgically operated on. All the two operated cases were caused by a damselfish FBFB. Thirty one cases (40.3%) were hospitalized after FBFB removal and the mean number of days of hospital treatment was 10.3 ± 17.3 days. Hospital admission was more common in the damselfish FBFB group (n = 22) compared with the other FBFB group (n = 9) and the mean number of days of hospital treatment was longer in the damselfish FBFB group compared with that of the other FBFB group (12.6 ± 20.0 cm vs 4.7 ± 4.8 cm, respectively, P = 0.02).
The scientific name of damselfish is Chromis notata. Among the many bony portions of damselfish causing esophageal fish bone foreign body, a uniquely-shaped linear bone portion was frequently noticed. Endoscopically, it was boomerang shaped and it had two sharp ends and a joint on the mid portion. It can penetrate both sides of the luminal wall of the esophagus and perforate it (Fig. 2). We examinated 18 damselfish that were caught in October to identify the specific boomerang-shaped, sharp portion of the damselfish bone. After boiling the damselfish, we took the meat off the bones. The typical shaped bone portion was found at the anal fin portion just posterior to the anus. One damselfish anal fin had 12 AFSs and the first two AFSs were ossified and very sharp. The first AFS was short, but the second AFS was very long and sharp. The first two AFSs were jointed to the inner pterygiophore. The first anal pterygiophore was also strongly ossified and long. Three portions of the bone were tightly adhered with joints. The mean length of the processed ASPC was 3.67 cm. They were not dislocated even after being hard-boiled, baked or roasted. They jointed with a wide angle and they flexed to 120°. The first and second AFSs were independently mobile. The tip of the pterygiophore was sharp. However, the AFSs were very sharp, hard and comparable to sewing needles (Fig. 3). Contrary to the very strong first and second AFSs, the pectoral and pelvic fins were relatively soft, and the first dorsal spines were short and easily dissociated from the pterygiophores.
The bone unit of the ASPC was very strong, dense and long enough to perforate both esophageal walls. The ASPC is linked by means of a simple joint and ligament. The ASPC is typically sharp at both ends. The spine side is sharper and harder. The long spine is the second AFS and the rudimentary small first AFS is also attached to it (Fig. 3). If the complex deeply penetrates the esophageal wall by the pterygiophore side, the FB removal becomes very difficult because the first AFS acts as an anchor in the esophageal wall during the foreign body removal.
In present study, fish bone was the most prevalent foreign body (61.1%) and meat was ranked second (20.6%); and this ranking was not different compared to other Asian country (2). Damselfish was the most prevalent source of FBFB. The high prevalence of damselfish FBFB may be due to 1) abundant and cheap, 2) traditionally favored fish, and 3) unique shape of the FBFB. In this study, it was unknown why the female patients were older than the male patients 60.9 ± 14.6 yr vs 54.1 ± 8.7 yr, respectively, and the trend was same in the damselfish and other fish FBFB disease groups.
Delayed hospital arrival is one of the poor prognostic factors. There was no significant difference of age and gender between early and later arrival groups. However, of 9 cases who were delayed over 48 hr, 8 cases (88.9%) were the patients of damselfish FBFB. We thought it was caused by the morphological characteristics of the damselfish FBFB; the both side penetrable shape of the FBFB, which enable decreased luminal pressure despite of both side perforation.
The sensitivity of plain radiography is low to detect foreign bodies, and early detection is depend on the bony calcification or kind of fishes (4, 5). CT is superior to plain radiographs for localizing and identifying foreign bodies and it is highly reliable for localizing foreign bodies in the esophagus (6). Some authors reported that the sensitivity and specificity of CT reached 78% and 96% respectively, and the positive and negative predictive value reached upto 75% and 97% respectively (7). In the present study, plain radiography detected only 7 fish bones in 67 cases (11.7%). A 6 of the 7 cases were caused by damselfish bones. The FBFBs detected by CT in 43 of 44 cases (97.7%). The missing case was caused by a 1-cm sized transparent small flat bone.
The local people usually eat raw flesh of medium sized fish as sashimi at first, and then boil the remaining fish head and back bones for soup for the medium sized fish. That is the reason why the flat fish skull bones were common in the other FBFBs. Exceptionally houttuyn is initially boiled for soup without eat sashimi. On the other hand, the majority of the local people cooks and eats damselfish as unboned state. Because the skull and back spine of damselfish are small and weak, the fishbone could be enough to chew and swallow without luminal lodgement. However the ASPC is too hard to be chewed. Of the total 36 cases of damselfish FBFB disease, 31 cases were caused by the ASPC. It is important that it has two sharp, bony ends that are long enough to penetrate deeply the esophageal wall.
Generally, esophageal perforation due to foreign body ingestion is rare and accounts for 1%-4% of the total reported cases (8). In one study, the pharyngeal location, fish bone, and radiolucency were associated with an increased incidence of complications in patients over 10 yr of age (9). The fish bones have a sharp polygonal or pin-like pointed structure and they can perforate or tear the esophageal wall. It can cause pneumomediastinum, mediastinitis, pneumothorax (10), tracheoesophageal fistula (11), major vascular damage (8, 12), and so far as to systemic air embolism in rare case (13). Upper esophageal and oropharyngeal FBFB can cause soft tissue infection and other complications including fistula formation and carotid arterial injury (14, 15). We already had several cases of pneumomediastinum, mediastinitis, and aortic injury.
Thoracic esophageal perforations carry a greater risk of morbidity and mortality than cervical esophageal perforations due to the operative risks (16). The overall mortality rate in the case of esophageal perforation is 22%, but the survival rate is up to 80%-90% when the primary repair is completed within 24 hr of rupture (17). Successful treatment of esophageal perforation is depends on the size of the perforation, the time delay to diagnosis and the underlying medical condition (18). In present study, only two cases underwent surgical operation because of abscess formation. In those cases, the time delay was 3 and 5 days before hospital arrival and the foreign body lodged to upper esophageal junction and hypopharynx. We had no case of mortality associated with FBFB disease and surgery. Except for the two cases, most of the cases successfully treated with conservative management.
Most of the small foreign bodies are naturally eliminated via the esophagus and gastrointestinal tract without symptom or complication (19). Therefore, nonoperative intervention is needed in 10%-20% of the cases; and surgical treatment is needed in 1% (20). The indications for surgery are peritoneal perforation, pneumothorax, clinical signs of systemic sepsis, respiratory insufficiency, shock and widespread of contamination due to a large perforation (21-24). In the other hand, the criteria for nonoperative treatment include early diagnosis, limited air leakage, not associated with visceral obstruction or malignancy, no evidence of septicemia (25-27), and the most reliable setting is locally contained and limited inflammatory changes surrounding the perforation (28). Antibiotics that active on both aerobes and anaerobes should be started because of the polymicrobic bacterial natures of the majority of cases and anaerobes predominance (29). In this study, many cases of FBFB due to the damselfish ASPC penetrated the esophageal wall. The majority of the perforations sealed with the FBFB itself and the perforation size were as small as a pin hole. Therefore, if the FBFB disease was diagnosed early and there were no signs and symptoms of mediastinitis, then medically supportive care would be sufficient.
The damselfish have an anal fin with two spines and adhered to the fish body by the pterygiophore (3). The pterygiophore is ossified linear bone serves as roots of the anal fins, and muscles for the movement of the fins are attached (30). The esophagus runs with the major vessels in the thoracic cavity, and it has three physiologic narrowed points. The portion near the aortic arch is one of them. In this study, the aortic arch level was included in the mid esophagus and 14.3% of all the FBFBs were lodged in the site. Damselfish FBFBs were relatively common in the mid esophagus (22.2%). The damselfish FBFBs are sharp and long enough to perforate the aorta or other thoracic organs. Several cases involved in the aorta or major vessels (Fig. 4).
In conclusion, damselfish FBFBs are most common in the people of Jeju Island. The majority of the FBFBs are caused by the ASPC and this caused a more significant clinical course. It is important to be aware that a damselfish FBFB can damage major vessels. This study is the first report that a specific part of fish bone, the ASPC, is the major cause of FBFB disease and it can be dangerous. We recommend removing the ASPC during cleaning the damselfish befor e cooking it. An early diagnosis and treatment is important because a delayed diagnosis can cause severe complications and increase the need for surgery.
Figures and Tables
Fig. 2
Typical features of a fish bone foreign body due to Chromis notata's anal fin spine-pterygiophore complex (ASPC). (A) The foreign body penetrates both side walls of the esophagus. (B) After the removal, the erosive-penetrated lesions remain at both sides of the esophageal wall. (C) The removed ASPC.

Fig. 3
Photography and radiography of the Chromis notata and its ASPC. (A) The raw fish. The arrow head denotes the anal fin. (B) The radiographic finding of the fish. The pterygiophore is deeply inserted to the fish body. Note the ASPC is one of the most radio-opaque portions in the fish skeleton. The pelvic spines (arrow) is also radio-opaque because they lay paired one upon another. (C) The magnified photography of the ASPC. It is a union of a pterygiophore and two anal fin spines (AFS) with a joint. The second AFS is longer than the first AFS. *Pterygiophore; †second AFS; ‡first AFS.

Fig. 4
Computed tomographic finding in two patients. (A) A typical case of esophageal damselfish bone foreign body. The ASPC penetrated both sided of the esophageal wall. Note that both sharp ends reached the wall of the descending aorta the inferior vena cava. (B-D) Serial sections of the aortic arch level of another patient. The tip of the damselfish bone penetrated the esophageal wall and the aortic wall (dotted circle).

Table 2
Clinical characteristics of fish bone foreign body disease

*Mean ± standard deviation, †Linear bone includes all the sharp and slender bones, including the ribs; skull bone includes the skull, mandible and gills; back bone includes the neural spine and tall bones. ‡Soup denotes all kinds of recipes with a broth component such as "maeuntang, jiri, guk": sliced with sauce denote sliced raw fish with sauce and this is called "jari mulhoe". FB, foreign body; CT, computed tomography; ASPC, anal fin spine-pterygiophore complex; ESP, esophagus.
References
1. Guitron A, Adalid R, Huerta F, Macias M, Sanchez-Navarrete M, Nares J. Extraction of foreign bodies in the esophagus. Experience in 215 cases. Rev Gastroenterol Mex. 1996. 61:19–26.
2. Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990. 211:459–462.
3. Nelson JS. Fishes of the World. 2006. 4th ed. Hoboken, New Jersey: John Wiley & Sons Inc.;393–394.
4. Wu IS, Ho TL, Chang CC, Lee HS, Chen MK. Value of lateral neck radiography for ingested foreign bodies using the likelihood ratio. J Otolaryngol Head Neck Surg. 2008. 37:292–296.
5. Ritchie T, Harvey M. The utility of plain radiography in assessment of upper aerodigestive tract fishbone impaction: an evaluation of 22 New Zealand fish species. N Z Med J. 2010. 123:32–37.
6. Shihada R, Goldsher M, Sbait S, Luntz M. Three-dimensional computed tomography for detection and management of ingested foreign bodies. Ear Nose Throat J. 2009. 88:910–911.
7. Luk WH, Fan WC, Chan RY, Chan SW, Tse KH, Chan JC. Foreign body ingestion: comparison of diagnostic accuracy of computed tomography versus endoscopy. J Laryngol Otol. 2009. 123:535–540.
8. Scher RL, Tegtmeyer CJ, McLean WC. Vascular injury following foreign body perforation of the esophagus. Review of the literature and report of a case. Ann Otol Rhinol Laryngol. 1990. 99:698–702.
9. Singh B, Kantu M, Har-El G, Lucente FE. Complications associated with 327 foreign bodies of the pharynx, larynx, and esophagus. Ann Otol Rhinol Laryngol. 1997. 106:301–304.
10. Shimizu T, Marusawa H, Yamashita Y. Pneumothorax following esophageal perforation due to ingested fish bone. Clin Gastroenterol Hepatol. 2010. 8:A24.
11. Mukhopadhyay B, Tripathy BB, Saha S, Shukla RM, Saha SR. Acquired tracheo-oesophageal fistula: a case report. J Indian Med Assoc. 2008. 106:806. 808.
12. Macchi V, Porzionato A, Bardini R, Parenti A, De Caro R. Rupture of ascending aorta secondary to esophageal perforation by fish bone. J Forensic Sci. 2008. 53:1181–1184.
13. Blanco Ramos M, Rivo Vazquez JE, Garcia-Fontan E, Amoedo TO. Systemic air embolism in a patient with ingestion of a foreign body. Interact Cardiovasc Thorac Surg. 2009. 8:292–294.
14. Maseda E, Ablanedo A, Baldo C, Fernandez MJ. Migration and extrusion from the upper digestive tract to the skin of the neck of a foreign body (fish bone). Acta Otorrinolaringol Esp. 2006. 57:474–476.
15. Okafor BC. Aneurysm of the external carotid artery following a foreign body in the pharynx. J Laryngol Otol. 1978. 92:429–434.
16. White RK, Morris DM. Diagnosis and management of esophageal perforations. Am Surg. 1992. 58:112–119.
17. Sabiston DCJ, Lyerly HK. Textbook of Surgery: the biological basis of modern surgical practice. 1997. 15th ed. Philadelphia: W.B. Saunders Co..
18. Katsetos MC, Tagbo AC, Lindberg MP, Rosson RS. Esophageal perforation and mediastinitis from fish bone ingestion. South Med J. 2003. 96:516–520.
19. McCanse DE, Kurchin A, Hinshaw JR. Gastrointestinal foreign bodies. Am J Surg. 1981. 142:335–337.
20. Nandi P, Ong GB. Foreign body in the oesophagus: review of 2394 cases. Br J Surg. 1978. 65:5–9.
21. Skinner DB, Little AG, DeMeester TR. Management of esophageal perforation. Am J Surg. 1980. 139:760–764.
22. Michel L, Grillo HC, Malt RA. Operative and nonoperative management of esophageal perforations. Ann Surg. 1981. 194:57–63.
23. Wesdorp IC, Bartelsman JF, Huibregtse K, den Hartog Jager FC, Tytgat GN. Treatment of instrumental oesophageal perforation. Gut. 1984. 25:398–404.
24. Radmark T, Sandberg N, Pettersson G. Instrumental perforation of the oesophagus. A ten year study from two ENT clinics. J Laryngol Otol. 1986. 100:461–465.
25. Cameron JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR. Selective nonoperative management of contained intrathoracic esophageal disruptions. Ann Thorac Surg. 1979. 27:404–408.
26. Altorjay A, Kiss J, Voros A, Bohak A. Nonoperative management of esophageal perforations. Is it justified? Ann Surg. 1997. 225:415–421.
27. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004. 77:1475–1483.
28. Shaffer HA Jr, Valenzuela G, Mittal RK. Esophageal perforation. A reassessment of the criteria for choosing medical or surgical therapy. Arch Intern Med. 1992. 152:757–761.
29. Brook I, Frazier EH. Microbiology of mediastinitis. Arch Intern Med. 1996. 156:333–336.
30. George VL. Evans DH, Claiborne JB, editors. Locomotion. The physiology of fishes. 2006. 3rd ed. Boca Raton, FL: Taylor & Francis Group;3–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download