Abstract
Chloracetanilide herbicides (alachlor, butachlor, metachlor) are used widely. Although there are much data about chronic low dose exposure to chloracetanilide in humans and animals, there are few data about acute chloracetanilide poisoning in humans. This study investigated the clinical feature of patients following acute oral exposure to chloracetanilide. We retrospectively reviewed the data on the patients who were admitted to two university hospitals from January 2006 to December 2010. Thirty-five patients were enrolled. Among them, 28, 5, and 2 cases of acute alachlor, metachlor, butachlor poisoning were included. The mean age was 49.8 ± 15.4 yr. The poison severity score (PSS) was 17 (48.6%), 10 (28.6%), 5 (14.3%), 2 (5.7%), and 1 (2.9%) patients with a PSS of 0, 1, 2, 3, and 4, respectively. The age was higher for the symptomatic patients (1-4 PSS) than that for the asymptomatic patients (0 PSS) (43.6 ± 15.2 vs 55.7 ± 13.5). The arterial blood HCO3 ¯ was lower in the symptomatic patients (1-4 PSS) than that in the asymptomatic patients (0 PSS). Three patients were a comatous. One patient died 24 hr after the exposure. In conclusion, although chloracetanilide poisoning is usually of low toxicity, elder patients with central nervous system symptoms should be closely monitored and cared after oral exposure.
Chloracetanilide herbicides are widely used in the United States, South America and Asian countries. Chloracetanilide herbicides are sold as alachlor, butachlor, metachlor and propachlor. This class of herbicides can control grasses and broad leaf weeds as a systemic herbicide. The herbicide's mode of action is not totally understood, but it is known that this class of herbicide inhibits the biosynthesis of lipids, alcohols, fatty acids, proteins, isoprenoids and flavonoids (1, 2). Alachlor is slightly toxic to mammals. The oral LD50 in rats ranges from 930 to 1,350 mg/kg (3). Several subchronic and chronic toxicology studies of alachlor have been conducted on animals and suggested the possibility of carcinogen (4-8). Genotoxicity studies and carcinogenicity studies have been conducted for chronic exposure or repeated doses of alachlor. Some studies have revealed that chronic exposure to alachlor causes nasal, stomach and thyroid tumors in animals. However, human data did not reveal that low exposure to alachlor could be carcinogenic (9, 10).
Butachlor and metachlor are also widely used in Asia, including Korea. These are a subclass of the acetamides, and have similar structures with alachlor. There are few data about acute exposure to chloracetanilide in animals or humans. The mechanism of toxicity following acute oral exposure has not been revealed. Lo et al. (11) retrospectively analyzed the cases reported to the Taiwan national poison center. Although alachlor and butachlor poisonings were usually of low toxicity, three of 113 patients died after manifesting profound hypotension and/or coma following alachlor ingestion. This suggested that alachlor poisoning could be fatal. There are few human data about acute chloracetanilide poisoning. Such clinical data should be collected and especially the data about the severe cases.
Therefore we investigated the clinical features, the poison severity score and the clinical course of patients following acute poisonings with three different chloracetanilide herbicides.
We retrospectively collected the data from the patients who were admitted to Soonchunhyang University Cheonan Hospital Pesticide Poisoning Center and the Ajou University Medical Center from January 2006 to December 2010. The subjects included in this study were all aged more than 18 yr and they had intentionally taken the poison orally. Patients were excluded if they were intoxicated with another pesticide in addition to chloracetanilide.
Trained physicians treated the patients and recorded all information on a standardized data-collection form. On admission, a standardized questionnaire including demographic characteristics and specific questions about the poisoning (amount of drug ingestion, time interval between ingestion and arrival, etc) was completed. Clinical toxicology specialist reviewed medical records.
The ingested amount was determined by the reported mouthfuls ingested (one mouthful was calculated as 20 mL). The time interval between ingestion and arrival at our centers was assessed. The following data was collected for each patient: symptoms, comorbidity, the poisoning severity score (PSS) within 24 hr following acute chloracetanilide intoxication, the initial laboratory parameters and the clinical outcomes (12). The PSS grades the severity of poisoning in five levels: 0) No symptoms or signs related to poisoning; 1) Minor, transient, and spontaneously resolving symptoms; 2) Pronounced or prolonged symptoms; 3) Severe or life-threatening symptoms; 4) Death. To investigate nephrotoxicity, we reviewed the sequential change of serum creatinine. We also investigated the incidence of rhabdomyolysis.
The symptoms were classified for four categories. The gastrointestinal category included nausea, vomiting, diarrhea and abdominal pain. Central nervous system involvement was documented if the patients presented with a change of mental status (alert, drowsy, stupor, coma, seizure). The cardiovascular category included hypertension (a systolic blood pressure > 140 mmHg or a diastolic blood pressure > 90 mmHg), hypotension (a systolic blood pressure < 90 mmHg), bradycardia (heart rate < 60/min) and tachycardia (heart rate > 100/min). The respiratory category included hypoxemia (PaO2 < 60 mmHg in room air) and respiratory failure (hypoxemia and require mechanical ventilation).
The data were presented as the mean ± standard deviation for continuous variables and as frequencies (in percents) for the categorical variables the differences between groups were compared with Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. A probability P < 0.05 was considered statistically significant. The statistical analysis was performed using SPSS for Windows (version 12.0, Chicago, IL, USA).
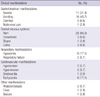
Thirty five patients were included in this study. They ingested alachlor (n = 28), metachlor (n = 5) and butachlor (n = 2), respectively. All the patients intentionally ingested the herbicides. Their mean age was 49.8 ± 15.4 yr. The baseline characteristics are shown in Table 1. After ingestion of chloracetanilide herbicide, most of the patients were asymptomatic or mild symptomatic (76.2%), but some patients were in a severe condition and one patient died. The PSS were as follows: 17 (48.6%) patients were PSS 0, 10 (28.6%) patients were PSS 1, 5 (14.3%) patients were PSS 2, 2 (5.7%) patients were PSS 3 and 1 (2.9%) patient was PSS 4. The age was higher for the symptomatic patients (1-4 PSS) than for the asymptomatic patients (0 PSS) (Table 1). The HCO3 ¯ was lower in the symptomatic patient (1-4 PSS) than that in the asymptomatic patients (0 PSS).
The serum creatinine was 1.5 mg/dL in 43 yr old man at 3 hr after metachlor poisoning. The serum creatinine was normalized (0.9 mg/dL) after hydration. Except this patient, nephrotoxicity was not observed.
The most frequent clinical manifestations were nausea and vomiting (Table 2). The central nervous system was normal in 80% of patients. Three patients were in a coma state at presentation. The first case was a 65 yr old man. He ingested 300 mL of alachlor to commit suicide. When he arrived at our hospital within 4 hr post ingestion, he had generalized tonic seizure and respiratory failure without cardiogenic shock. Benzodiazepine (midazolam 0.2 mg/kg bolus, 0.1 mg/kg maintenance) was intravenously injected and mechanical ventilation was applied. The seizure was not controlled by benzodiazepine, so phenytoin (1,000 mg loading, 100 mg q 8 hr maintenance) was administered intravenously. Fever then developed followed by rhabdomyolysis. After 22 days, mechanical ventilation was weaned.
Throughout this series, one fatality occurred. The patient was a 75-yr-old woman who ingested 300 mL of alachlor pesticide to commit suicide. When she arrived at the emergency room after 2 hr following ingestion of alachlor, her blood pressure was 110/70 mmHg. Soon her blood pressure dropped and her respiration was shallow. Inotropic agents were injected and intubation was done. Mechanical ventilation was applied. Deep coma developed within 3 hr after ingestion. She died due to severe cardiogenic shock at 24 hr post-ingestion.
Among them, the other one patient was a 45-yr-old woman. She recovered within 2 days and that patient underwent hemoperfusion.
In vivo and vitro studies, chronic exposure to chloracetanilide might be involved with neurotoxicity, genotoxicity and carcinogenicity (4-8). There have been studies on humans to investigate long term occupational exposure to alachlor and the incidence of cancer, the mortality and the effects on ocular health (9, 10). The data did not show that chronic exposure to low levels of alachlor was associated with an ocular effect, mortality and the incidence of cancer. Therefore it has been known that alachlor has low potential for adverse effects among workers who are exposed to low levels of alachlor.
There might be a difference between chronic exposure and acute exposure. The clinical data about chloracetanilide herbicide poisoning is rarely reported, although the herbicide has been widely used. So, we thought that some data are needed to predict the prognosis of patients with oral exposure and to determine the risk factors for severe symptom, including the effect of central nervous system, respiratory and cardiovascular systems. Lo et al. (11) recently suggested that alachlor and butachlor poisoning is usually of low toxicity. They reported 3 fatalities among 102 patients with oral exposure to alachlor or butachlor. Twenty-five percent of the oral exposure patients showed the effects on central nervous system.
Our data also showed the effects on central nervous systems in 20% of our patients. Among these patients, two patients developed respiratory failure and one patients died. The cause of the central nervous system (CNS) manifestations might be the direct effect of alachlor or the solvents added in the herbicides. Anyway, CNS effects suggest a severe case, and so clinicians should closely observe such a patient and promptly treat a patient with CNS symptoms after oral exposure to chloracetanilide herbicide.
We investigated the poison severity score. When comparing the asymptomatic patients (0 PSS) with the symptomatic patients (1-4 PSS), the symptomatic patients were significantly older and they had a lower bicarbonate level than the asymptomatic patients. Although there was no statistical significance, estimated amount of exposure tended to be larger in the symptomatic patients than in asymptomatic patients. We suggest that old age people with an initial low bicarbonate level could developed symptoms within 24 hr after oral exposure of chloracetanilide herbicide.
In our study, two cases of rhabdomyolysis were observed among 35 patients. Drug induced myopathy may result from several different mechanisms, and these are direct myotoxicity (mitochondrial myopathy), immunologically-induced inflammatory myopathy and indirect muscle damage (drug-induced coma, subsequent ischemic muscle compression, drug-induced hypokalemia, drug-induced hyperkinetic states, dystonic states, hyperthermia) (13, 14). In our study, one patient had seizure, which could have been indirect myotoxicity, but the others had no seizure, which suggests direct toxicity. Some studies showed that alachlor induced cellular injury were involved with reactive oxygen species production (15). So alachlor itself could cause muscle injury. There is not much data on herbicide-induced myopathy. Further in vivo and vitro studies about pesticide-induced myopathy are needed.
Our study has some limitations. First, this study had a retrospective design, including the use of data from past medical records. Second, ours was a small sized study. Although this study had some limitations, our data suggested acute oral exposure to chloracetanilide could be severe or fatal.
In conclusion, although chloracetanilide poisoning is usually of low toxicity, elder patients with CNS symptoms should be closely monitored and cared after oral exposure.
Figures and Tables
References
1. Ecobichon DJ. Klaassen CP, editor. Toxic effects of pesticides. Casarett & Doull's toxicology: the basic science of poisons. 2001. 6th ed. New York: McGraw-Hill Medical Pub Division;794–795.
2. Heydens WF, Lamb IC, Wilson AG. Krieger R, editor. Chloracetanilides. Handbook of pesticide yoxicology. 2002. 2nd ed. San Diego: Academic Press;1543–1558.
3. Ahrens WH. Herbicide handbook of the weed science society of America. 1994. 7th ed. Champaign: Weed Science Society of America.
4. Dearfield KL, McCarroll NE, Protzel A, Stack HF, Jackson MA, Waters MD. A survey of EPA/OPP and open literature on selected pesticide chemicals. II. Mutagenicity and carcinogenicity of selected chloroacetanilides and related compounds. Mutat Res. 1999. 443:183–221.
5. Burman DM, Shertzer HG, Senft AP, Dalton TP, Genter MB. Antioxidant perturbations in the olfactory mucosa of alachlor-treated rats. Biochem Pharmacol. 2003. 66:1707–1715.
6. Gebel T, Kevekordes S, Pav K, Edenharder R, Dunkelberg H. In vivo genotoxicity of selected herbicides in the mouse bone-marrow micronucleus test. Arch Toxicol. 1997. 71:193–197.
7. Osano O, Admiraal W, Klamer HJ, Pastor D, Bleeker EA. Comparative toxic and genotoxic effects of chloroacetanilides, formamidines and their degradation products on Vibrio fischeri and Chironomus riparius. Environ Pollut. 2002. 119:195–202.
8. Dierickx PJ. Glutathione-dependent cytotoxicity of the chloroacetanilide herbicides alachlor, metolachlor, and propachlor in rat and human hepatoma-derived cultured cells. Cell Biol Toxicol. 1999. 15:325–332.
9. Heydens WF, Wilson AG, Kier LD, Lau H, Thake DC, Martens MA. An evaluation of the carcinogenic potential of the herbicide alachlor to man. Hum Exp Toxicol. 1999. 18:363–391.
10. Acquavella JF, Riordan SG, Anne M, Lynch CF, Collins JJ, Ireland BK, Heydens WF. Evaluation of mortality and cancer incidence among alachlor manufacturing workers. Environ Health Perspect. 1996. 104:728–733.
11. Lo YC, Yang CC, Deng JF. Acute alachlor and butachlor herbicide poisoning. Clin Toxicol (Phila). 2008. 46:716–721.
12. Persson HE, Sjöberg GK, Haines JA, Pronczuk de Garbino J. Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998. 36:205–213.
13. Lane RJ, Mastaglia FL. Drug-induced myopathies in man. Lancet. 1978. 2:562–566.
14. Sieb JP, Gillessen T. Iatrogenic and toxic myopathies. Muscle Nerve. 2003. 27:142–156.
15. Grizard G, Ouchchane L, Roddier H, Artonne C, Sion B, Vasson MP, Janny L. In vitro alachlor effects on reactive oxygen species generation, motility patterns and apoptosis markers in human spermatozoa. Reprod Toxicol. 2007. 23:55–62.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download