Abstract
The purpose of this study was to determine the clinical significance of nodal micrometastasis detected by immunohistochemistry in patients that had undergone curative surgery for pancreatic cancer. Between 2005 and 2006, a total of 208 lymph nodes from 48 consecutive patients with pancreatic cancer that had undergone curative resection were immunostained with monoclonal antibody against pan-ck and CK-19. Micrometastasis was defined as metastasis missed by a routine H&E examination but detected during an immunohistochemical evaluation. Relations between immunohistochemical results and clinical and pathologic features and patient survival were examined. Nodal micrometastases were detected in 5 (29.4%) patients of 17 pN0 patients. Nodal micrometastasis was found to be related to tumor relapse (P = 0.043). Twelve patients without overt nodal metastasis and micrometastasis had better prognosis than 5 patients with only nodal micrometastasis (median survival; 35.9 vs 8.6 months, P < 0.001). The Cox proportional hazard model identified nodal micrometastasis as significant prognostic factors. Although the number of patients with micrometastasis was so small and further study would be needed, our study suggests that the lymph node micrometastasis could be the predictor of worse survival and might indicate aggressive tumor biology among patients undergoing curative resection for pancreas cancer.
Ductal adenocarcinoma of the pancreas is a highly aggressive malignancy with a remarkably poor prognosis, and unfortunately, even for patients with apparently localized surgically resectable disease, long-term survival after curative resection remains poor. In fact, majority of patients with pancreatic cancer suffer from postoperative local recurrence or distant metastasis despite histologically confirmed curative resection and tumor free lymph nodes. These recurrences are thought to arise from occult tumor cell dissemination or micrometastatic disease that cannot be detected using current staging procedures (1-3). Accordingly, more sensitive techniques, such as immunohistochemistry and molecular biology assays, to detect minimal residual disease of pancreatic cancer with the potential for metastasis have been introduced. Immunohistochemical assays were the earliest to be developed, and these are more frequently used than other alternatives in several cancers including those of the breast (4, 5), lung (6, 7), stomach (8, 9), and colon (10, 11). The majority of studies have used antibodies against a broad spectrum of cytokeratins (CK) (4-11). However, little is known about the clinical significance of nodal micrometastasis in pancreatic cancer (12-15). Accordingly, we conducted this study to investigate the clinical significance of nodal micrometastasis detected by immunohistochemical staining with antibodies against cytokeratin (pan-CK and CK-19) in pancreatic cancer patients that had undergone curative surgery.
Forty-eight patients who underwent macroscopically curative resection (12 cases of pancreatoduodenectomy and 36 cases of pylorus preserving pancreatoduodenectomy) for ductal adenocarcinoma of the pancreatic head at Seoul National University Hospital from 2005 to 2006 were evaluated. No patients received any preoperative chemotherapy or radiotherapy. Preoperative work-up included laboratory investigations such as tumor markers (CEA and CA19-9) and radiologic studies (chest radiograph, triple phase MDCT in 2.5 mm slice thickness). For further evaluation, 3D-GRE MRI with MRCP or 18F-FDG PET/CT were also checked. Primary tumor and lymph nodes were prospectively collected from all 48 consecutive patients, and resected primary tumors and lymph nodes were examined histologically by H&E staining. Histopathologic and TNM classifications were made in accordance with the Union Internacional Contra la Cancrum (UICC) classification of 2002 (16). Resected lymph nodes included; posterior pancreatoduodenal lymph nodes, lymph nodes around the celiac axis, common hepatic artery, hepatoduodenal ligament, and superior mesenteric artery, and para-aortic lymph nodes. A tumor-free margin was achieved in all patients. Follow-up durations ranged from 5 to 41.9 months (median, 20 months) and patient survivals were determined from surgery to death or most recent follow-up. All patients were followed-up after discharge as follows: plain-film radiography every 1-3 months, and computed tomography every 3-6 months.
The study group contained 32 men and 16 women ranging in age from 43 to 78 yr (median, 62 yr). One patient had a pT1 tumor and the other 47 patients a pT3 tumor. Pathologically, all tumors were invasive ductal adenocarcinomas (46 moderately differentiated, 2 poorly differentiated). Of the 48 patients, 17 had no lymph node disease (pN0) as determined by H&E staining, and the remaining 31 had lymph node involvement (pN1).
A total of 1,221 lymph nodes (25.4 nodes/patient), including 836 regional, 160 paraaortic, and 225 paragastric or paracolic nodes, were retrieved from the 48 sets of surgical specimens. Among the 1,221 lymph nodes, a total of 208 lymph nodes were sampled (4.3 nodes/patient). Two serial 3-µm sections were cut from each node area. One section was routinely for H&E stained for histologic examination, and the other was stained pan-CK and CK-19 mouse monoclonal antibody (DAKO, Glostrup, Denmark) for immunohistochemical examination. Antibody binding was detected using Vectastain ABC 'Elite' avidin/biotin/peroxidase kits (Vector laboratories, Burlingame, CA, USA) according to the manufacturer's instructions. After deparaffinizing and rehydrating sections were pretreated with 10 mM citrate buffer solution (pH 6.0) for 15 min in a 700 W or more microwave to retrieve antigens, endogenous peroxidase activity was then blocked by treating sections with 3% hydrogen peroxide for 6 min. Sections were then incubated with primary monoclonal antibody diluted at 1:100 in PBS at room temperature for 1 hr. After rinsing, sections were incubated with secondary antibody, and then treated with biotinylated anti-mouse IgG. Reaction products were visualized with DAB (diaminobenzidine; Sigma, St. Louis, MO, USA) as chromogen, and sections were counterstained with Mayer's hematoxylin. H&E and immunohistochemically stained sections were examined independently for metastasis by an experienced pathologist unaware of clinical details.
The term "overt" lymph node metastasis is used to describe a metastasis detected during a routine histologic examination by H&E staining. The "micrometastasis" is used to describe a metastasis missed by a routine H&E staining but detected by an anticytokeratin antibody immunohistochemical study. Lymph node micrometastases were visualized as single-cells or as small clusters of tumor cells.
Results are expressed as mean ± SD. Statistical analysis was performed using Fisher's exact probability test or the Mann-Whitney U test, as appropriate. Postoperative survivals were calculated using the Kaplan-Meier method and differences between survival curves were compared using the log-rank test. Multivariate analysis was conducted using the Cox proportional hazard model. Statistical significance was accepted for P value of < 0.05.
The study group consisted of 48 patients with ductal adenocarcinomas of the pancreas with histologically tumor-free resection margins (R0). Routine histopathological examinations of resected lymph nodes revealed lymph node metastasis in 31 patients (64.6%) of total 48 patients and 104 (8.5%) of 1,221 resected lymph nodes.
For the immunohistochemical analysis, a total of 208 lymph nodes from these 48 patients were sampled. Of these sampled lymph nodes, H&E staining identified 16 (7.7%) positive nodes while immunohistochemical staining identified 24 (11.5%) positive nodes that were judged to be "tumor-free" by routine histopathology including 8 (33.3%) single cell micrometastases and 16 (66.7%) cluster micrometastases. Of the 17 patients with pN0 disease, micrometastases were detected in 5 (29.4%) patients including two patients with single cell micrometastases and 3 patients with cluster micrometastases.
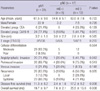
Nodal micrometastases were most frequently found in posterior pancreatoduodenal nodes (28.1%) (Table 1). Clinicopathologic details of the 31 patients with overt metastasis (pN1), of the 5 patients with micrometastasis and without overt metastasis (pN0mi[i+]) and of the 12 patients with neither micrometastasis nor overt metastasis (pN0mi[i-]) are shown in Table 2. Nodal micrometastasis was found to be significantly related to tumor relapse (P = 0.026).
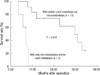
The 31 patients with overt node metastasis exhibited significantly worse survival compared with the 17 patients without overt node metastasis(median survival; 16.3 vs 27.8 months, P = 0.05). Survival of the 21 patients with lymph node micrometastasis regardless as to whether the nodal metastasis was overt or not was poorer than that of the 27 patients without lymph node micrometastasis (median survival; 12.8 vs 27.3 months, P = 0.008) (Fig. 1). The 12 patients without overt metastasis or micrometastasis had a better prognosis than the 5 patients with only nodal micrometastasis (median survival; 35.9 vs 8.6 months, P < 0.001) (Fig. 2). Five patients with only nodal micrometastasis developed tumor relapse within a median time of 3.9 months; relapse occurred in the liver in 4 and in the skull in one.
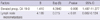
Univariate analysis revealed that overt lymph node metastasis (P = 0.05), lymph node micrometastasis (P < 0.001), poor differentiation (P < 0.001), angiolymphatic invasion (P = 0.05), and an elevated preoperative serum CA 19-9 level (P = 0.01) were significant poor prognostic factors. Multivariate analysis using the Cox proportional hazard model was performed using these five significant variables, lymph node micrometastasis (P < 0.001) and an elevated preoperative serum CA 19-9 level (P = 0.01) were found to be significant independent prognostic factors (Table 3).
Lymph node metastasis is known to be an important prognostic factor in patients with pancreatic cancer. However, even in patients with pN0 disease, 5-yr survival rates following resection have been reported to be as low as 5%-36% (17-19). The question why some node negative patients die within a few months after curative resection is not sufficiently answered because of metastases or local recurrence whereas others enjoy a more favorable outcome. Early metastatic relapse after complete resection of an apparently localized primary pancreatic cancer lesion indicates that disseminated tumor cells, undetectable by current methods, were probably present at the time of surgery. Knowledge about occult metastases is essential to patients and their physicians in deciding on a course of adjuvant treatment to improve the postoperative outcome.
In this study, we detected the lymph node micrometastasis by the immunohistochemical staining for cytokeratin. Although conclusive results are not available, cytokeratin is a component of the cytoskeleton of epithelial cells that is not present in normal lymph nodes; therefore, immunohistochemistry using an antibody that recognizes cytokeratin enables the detection of minute deposits of tumor cells in the lymph nodes. We hypothesized that the relatively low survival rate of node-negative pancreatic cancer could result from the presence of lymph node micrometastasis. Only patients without a gross residual tumor were used in this study because it might have concealed the prognostic significance of nodal micrometastasis and the present study shows that isolated tumor cells or small tumor cell clusters detected in lymph nodes using a sensitive immunohistochemical assay method independently predict relapse-free and overall survival in pancreatic cancer, regardless of overt nodal status.
Comparing with other studies (1, 14, 15) on pancreas cancer and other carcinomas (2, 4-11, 20-22), our study appeared a contradictory result that five of our patients with nodal micrometastasis but no overt metastasis achieved poorer survival than 12 patients without neither micrometastasis nor overt metastasis (Fig. 2). This number is far too small to allow a firm conclusion to be drawn, but considering the previous study (23) about gallbladder cancer that reported similar results, we could explain the results as follows. Nodal micrometastasis presents as single cells or small clusters of tumor cells. It is likely that single cells or small clusters of cells can migrate more easily within the lymphatic system than larger cell aggregates. These free cancer cells in the lymphatic system could enter the systemic blood stream by a venous route or via the thoracic duct, and then spread systemically. We therefore think that nodal micromeatstasis could be also an indicator of systemic spread. In our series, tumor relapse occurred predominantly at distant sites in patients with nodal micrometastasis. This finding suggests that these cells are indicators of generalized occult metastatic disease with a high load of residual tumor cells, rather than indicators of advanced locoregional disease that might be controlled by radical tumor resection with tumor free resection margins. However, till now, it is unclear the potential of disseminated cells to develop into overt metastasis.
Some defined micrometastasis as metastatic tumor cells not detectable on routine histologic examination, whereas others (24-27) considered metastatic tumor cells by size into "micrometastases" (measuring > 0.2 mm) and "isolated tumor cells" (measuring ≤ 0.2 mm), as recommended by the sixth edition of the TNM classification of malignant tumors by UICC (16). Our definition of micrometastasis was the presence of tumor cells in regional lymph nodes not detected on routine H&E staining and we divided the metastasis into single-cell and cluster types in light of previous suggestions that this differentiation may be important (24-27). However, in our study, the patient number analyzed (single cell micrometastases, n = 2, cluster micrometastases, n = 3) was too small to compare the prognosis between two groups. Further discussions are required to reveal the difference in prognostic impact between single and cluster micrometastases.
In the present study, only 2 serial sections from each lymph node, 1 for routine H&E staining and another for immunohistochemical staining, were examined for metastasis. Although the examination of a representative section per node is standard practice at our institution and others (9, 11, 28), some authors recommended the use of multiple sections (20-22). If we had used multiple sections, the incidences of nodal micometastasis might have been higher. However, because immunohistochemical examinations for lymph node micrometastasis are time-consuming and rather expensive, there is still no consensus about how many slides should be considered as representative samples for the detection of micro-metastases.
In conclusion, our study suggests that lymph node micrometastasis is the predictor of reduced survival and indicate aggressive tumor biology among patients undergoing curative resection for pancreas cancer. Although our study was prospective in nature and, hence, free from biases that may arise from retrospective reviews, it is limited by small sample size to reach a definite conclusion. Elucidation of the characteristics of the disseminated cancer cells are required for future researches and it is likely that in the future a prognostic profile combining primary tumor characteristics and nodal analysis will be part of a more comprehensive staging schema similar to that currently being used in breast cancer.
Figures and Tables
Fig. 1
Overall survival graph. Outcome after resection for patients without nodal micrometastasis compared favorably with those with nodal micrometastasis (P = 0.008).
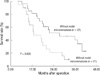
Fig. 2
Overall survival graph. The outcome after resection in patients with neither overt nodal metastasis nor nodal micrometastasis compared favorably with those with no overt nodal metastasis and nodal micrometastasis (P < 0.001).
AUTHOR SUMMARY
Clinical Implications of Immunohistochemically Demonstrated Lymph Node Micrometastasis in Resectable Pancreatic Cancer
Seung Eun Lee, Jin-Young Jang, Min-A Kim and Sun-Whe Kim
We investigated the clinical significance of nodal micrometastasis detected by immunohistochemistry in patients underwent curative surgery for pancreatic cancer. Although the small number of patients with micrometastasis requests further study, the result suggests that the lymph node micrometastasis could be the predictor of worse survival, and might indicate aggressive tumor biology.
References
1. Benassai G, Mastrorilli M, Quarto G, Cappiello A, Giani U, Forestieri P, Mazzeo F. Factors influencing survival after resection for ductal adenocarcinoma of the head of the pancreas. J Surg Oncol. 2000. 73:212–218.
2. Noguchi S, Aihara R, Motomura K, Inaji H, Imaoka S, Koyama H. Detection of breast cancer micrometastases in axillary lymph nodes by means of reverse transcriptase-polymerase chain reaction. Am J Pathol. 1996. 148:649–656.
3. Trede M, Richter A, Wendl K. Personal observations, opinions, and approaches to cancer of the pancreas and the periampullary area. Surg Clin North Am. 2001. 81:595–610.
4. McGuckin MA, Cummings MC, Walsh MD, Hohn BG, Bennett IC, Wright RG. Occult axillary node metastases in breast cancer: their detection and prognostic significance. Br J Cancer. 1996. 73:88–95.
5. Clare SE, Sever SF, Wilkens W, Goldschmidt R, Merkel D, Winchester DJ. Prognostic significance of occult lymph node metastases in node-negative breast cancer. Ann Surg Oncol. 1997. 4:447–451.
6. Goldstein NS, Mani A, Chmielewski G, Welsh R, Pursel S. Immunohistochemically detected micrometastases in peribronchial and mediastinal lymph nodes from patients with T1, N0, M0 pulmonary adenocarcinomas. Am J Surg Pathol. 2000. 24:274–279.
7. Ohta Y, Oda M, Wu J, Tsunezuka Y, Hiroshi M, Nonomura A, Watanabe G. Can tumor size be a guide for limited surgical intervention in patients with peripheral non-small cell lung cancer? Assessment from the point of view of nodal micrometastasis. J Thorac Cardiovasc Surg. 2001. 122:900–906.
8. Maehara Y, Oshiro T, Endo K, Baba H, Oda S, Ichiyoshi Y, Kohnoe S, Sugimachi K. Clinical significance of occult micrometastasis lymph nodes from patients with early gastric cancer who died of recurrence. Surgery. 1996. 119:397–402.
9. Cai J, Ikeguchi M, Maeta M, Kaibara N. Micrometastasis in lymph nodes and microinvasion of the muscularis propria in primary lesions of submucosal gastric cancer. Surgery. 2000. 127:32–39.
10. Jeffers MD, O'Dowd GM, Mulcahy H, Stagg M, O'Donoghue DP, Toner M. The prognostic significance of immunohistochemically detected lymph node micrometastases in colorectal carcinoma. J Pathol. 1994. 172:183–187.
11. Oberg A, Stenling R, Tavelin B, Lindmark G. Are lymph node micrometastases of any clinical significance in Dukes stages A and B colorectal cancer? Dis Colon Rectum. 1998. 41:1244–1249.
12. Kanemitsu K, Hiraoka T, Tsuji T, Inoue K, Takamori H. Implication of micrometastasis of lymph nodes in patients with extended operation for pancreatic cancer. Pancreas. 2003. 26:315–321.
13. Hosch SB, Knoefel WT, Mety S, Stoecklein N, Niendorf A, Broelsch CE, Izbicki JR. Early lymphatic tumor cell dissemination in pancreatic cancer: frequency and prognostic significance. Pancreas. 1997. 15:154–159.
14. Scheunemann P, Stoecklein NH, Rehders A, Bidde M, Metz S, Peiper M, Eisenberger CF, Schulte Am Esch J, Knoefel WT, Hosch SB. Occult tumor cells in lymph nodes as a predictor for tumor relapse in pancreatic adenocarcinoma. Langenbecks Arch Surg. 2008. 393:359–365.
15. Kurahara H, Takao S, Maemura K, Shinchi H, Natsugoe S, Aikou T. Impact of lymph node micrometastasis in patients with pancreatic head cancer. World J Surg. 2007. 31:483–490.
16. Frederick LG. AJCC cancer staging manual. 2002. 6th ed. Chicago: Springer.
17. Peters JH, Carey LC. Historical review of pancreaticoduodenectomy. Am J Surg. 1991. 161:219–225.
18. Reinders ME, Allema JH, van Gulik TM, Karsten TM, de Wit LT, Verbeek PC, Rauws EJ, Gouma DJ. Outcome of microscopically nonradical, subtotal pancreaticoduodenectomy (Whipple's resection) for treatment of pancreatic head tumors. World J Surg. 1995. 19:410–414.
19. Jung KW, Kim MH, Lee TY, Kwon S, Oh HC, Lee SS, Seo DW, Lee SK. Clinicopathological aspects of 542 cases of pancreatic cancer: a special emphasis on small pancreatic cancer. J Korean Med Sci. 2007. 22:Suppl. S79–S85.
20. Gu CD, Osaki T, Oyama T, Inoue M, Kodate M, Dobashi K, Oka T, Yasumoto K. Detection of micrometastatic tumor cells in pN0 lymph nodes of patients with completely resected non-small cell lung cancer: impact on recurrence and survival. Ann Surg. 2002. 235:133–139.
21. Glickman JN, Torres C, Wang HH, Turner JR, Shahsafaei A, Richards WG, Sugarbaker DJ, Odze RD. The prognostic significance of lymph node micrometastasis in patients with esophageal carcinoma. Cancer. 1999. 85:769–778.
22. Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg. 2003. 237:201–207.
23. Vogel I, Krüger U, Marxsen J, Soeth E, Kalthoff H, Henne-Bruns D, Kremer B, Juhl H. Disseminated tumor cells in pancreatic cancer patients detected by immunocytology: a new prognostic factor. Clin Cancer Res. 1999. 5:593–599.
24. Marinho VF, Zagury MS, Calderia LG, Gobbi H. Relationship between histologic features of primary breast carcinomas and axillary lymph node micrometastases: detection and prognostic significance. Appl Immunohistochem Mol Morphol. 2006. 14:426–431.
25. Rena O, Carsana L, Cristina S, Papalia E, Massera F, Errico L, Bozzola C, Casadio C. Lymph node isolated tumor cells and micrometastases in pathological stage I non-small cell lung cancer: prognostic significance. Eur J Cardiothorac Surg. 2007. 32:863–867.
26. Lee HS, Kim MA, Yang HK, Lee BL, Kim WH. Prognostic implication of isolated tumor cells and micrometastases in regional lymph nodes of gastric cancer. World J Gastroenterol. 2005. 11:5920–5925.
27. Messerini L, Cianchi F, Cortesini C, Comin CE. Incidence and prognostic significance of occult tumor cells in lymph nodes from patients with stage IIA colorectal carcinoma. Hum Pathol. 2006. 37:1259–1267.
28. Sakata E, Shirai Y, Yokoyama N, Wakai T, Sakata J, Hatakeyama K. Clinical significance of lymph node micrometastasis in ampullary carcinoma. World J Surg. 2006. 30:985–991.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download