Abstract
The purpose of this study was to evaluate the value of fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) for detecting the recurrence of gastric cancer. We performed a retrospective review of 139 consecutive patients who underwent PET/CT and contrast-enhanced abdominal CT (CECT) for surveillance of gastric cancer after curative resection. Recurrence of gastric cancer was validated by histopathologic examination for local recurrence or serial imaging study follow-up with at least 1 yr interval for recurrence of distant metastasis form. Twenty-eight patients (20.1%) were confirmed as recurrence. On the patient based analysis, there was no statistically significant difference in the sensitivity, specificity and accuracy of PET/CT (53.6%, 84.7%, and 78.4%, respectively) and those of CECT (64.3%, 86.5%, and 82.0%, respectively) for detecting tumor recurrence except in detection of peritoneal carcinomatosis. Among 36 recurrent lesions, 8 lesions (22.2%) were detected only on PET/CT, and 10 lesions (27.8%) only on CECT. PET/CT had detected secondary malignancy in 8 patients. PET/CT is as accurate as CECT in detection of gastric cancer recurrence after curative resection, excepting detection of peritoneal carcinomatosis. Moreover, additional PET/CT on CECT could improve detection rate of tumor recurrence and provide other critical information such as unexpected secondary malignancy.
Gastric cancer is the second most common cause of cancer death worldwide (1). Within the Asian region, the incidence of gastric cancer is high, and it is the most common cancer in Korea (2).
Complete surgical resection of gastric cancer is considered potentially curative, but its long-term survival is frequently reported as poor. In fact, despite successful surgery, the five-year survival rate is approximately 35%; and even with adjuvant chemotherapy in selected patients, the survival rate is 40% (3). After curative surgery, about 80% of the patients die within a short period of time from locoregional recurrence (87%) and/or distant metastasis (30%) (4).
To detect the gastric cancer recurrence, various methods such as tumor markers, endoscopy or imaging studies have been used. Contrast-enhanced abdominal computed tomography (CECT) has been most popularly used imaging study in diagnosing recurrent gastric cancer. To date, however, only few reports have been published on CECT findings after gastrectomy (5, 6). They described that CECT lacks specificity particularly in diagnosing local recurrence because its diagnostic capability is based on only the morphologic changes of the involved organs, and distorted anatomic structures make image interpretation difficult (5).
Positron emission tomography (PET) with 18F-fluorodeoxyglucose (FDG) is a non-invasive technique for determination of metabolically active lesions, which has been widely used for restaging or follow-up after treatment in various cancers (7-9). However, unlike the other cancers, only limited number of reports is available on the use of PET or integrated PET/CT in detecting recurrent gastric cancer (1, 10-14).
The purpose of this study was to evaluate the efficacy of PET/CT for detecting gastric cancer recurrence after curative resection, and to compare the diagnostic accuracy of FDG PET/CT with that of CECT.
Between August 2007 and July 2008, 139 consecutive patients (age, 61.5 ± 11.6 yr; 88 men and 51 women) were retrospectively enrolled for this investigation. The study inclusion criteria were as follows: 1) an interval of less than 3 yr between curative surgical resection and study inclusion, 2) both integrated PET/CT and CECT were performed within 2 months for the surveillance of gastric cancer recurrence with or without suspicion of recurrence, and 3) for suspicious lesion of local or distant recurrence, histopathologic confirmation through endoscopic biopsy or serial imaging study follow-up for at least 1 yr interval, were performed.
The initial treatment methods of these patients included total gastrectomy (n = 12), proximal gastrectomy (n = 6), radical subtotal gastrectomy with Billroth anastomosis (n = 116), endoscopic mucosal resection (n = 4) and wedge resection (n = 1). Their histopathologic types included adenocarcinoma (n = 117), signet ring cell carcinoma (n = 19), mucinous adenocarcinoma (n = 1) and others (n = 2). All patients underwent follow-up gastroscopy, CECT and PET/CT scans after surgery at 3 to 6 months intervals. The follow-up period from initial surgery to the final confirmation of recurrence ranged from 3.6 to 46.2 months (18.5 ± 9.0 months). A mean interval between CECT and PET/CT scans was 11 days. The final confirmation for the presence or absence of recurrence was done histopathologically in 25 patients (endoscopic biopsy, n = 22; surgery, n = 2; percutaneous biopsy, n = 1) and radiologically in 114 patients. These final confirmations were considered as gold standards for patient or organ based analysis.
All follow-up CECT scans were performed with multi-detector row CT scanners (Somatom Volume Zoom, Siemens AG, Enlangen, Germany), spanning from the liver dome to the pelvic floor. Each patient drank 200 mL of water just before undergoing CECT. Scanning was started 45 sec after the intravenous injection of 100-120 mL of iopromide (Ultravist 300, Schering Korea, Seoul, Korea) at a rate of 3 mL/sec. A slice collimation of 1.2 mm and a table pitch of 1:1 were used. Images were reconstructed at 5 mm intervals.
FDG was prepared using a cyclotron (RDS-111, CTI Cyclotron Systems, Inc., Daejeon, Korea) and automated synthesis apparatus. The radiochemical and chemical purity of the product was assayed by analytic high-performance liquid chromatography and thin-layer chromatography and was consistently > 99% by both assays. The measured specific activity of the FDG was > 740 GBq/mM at the end of synthesis. Patients fasted for at least 8 hr and drank 300 mL of water just before undergoing FDG PET/CT. The PET/CT scan was started 55-60 min after the administration of 296-444 MBq FDG using an integrated PET/CT system (Biograph Sensation 16, Siemens Medical Systems, Munich, Germany). The axes of both systems are mechanically aligned to coincide optimally. CT data were acquired first and the following parameters were used: tube rotation time 0.5 sec per revolution, 120 kV, 140 mAs, reconstructed slice thickness 5 mm. No contrast medium was used for the CT examination. After the CT data had been completely acquired, the table top with the patient automatically advanced into the PET sensitive field of view and acquisition of PET data was started in three-dimensional mode with the patient in exactly the same position on the table. Scanning was performed in one bed position for 3 min. The attenuation correction was automatically completed using corresponding CT data.
All recurrent lesions were classified into 5 categories: 1) locoregional recurrence, the recurrence in remnant stomach or anastomotic site, 2) regional lymph node (RegLN) recurrence, the recurrence in pancreatic, splenic and perigastric lymph nodes along the lesser and greater curvatures, 3) liver, the recurrence of hepatic metastasis form, 4) peritoneal carcinomatosis, and 5) distant recurrence, the recurrence in lymph node or organ excepting the liver. Multiple lesions within one category were considered as a one lesion.
All CECT images were analyzed retrospectively by two experienced abdominal radiologists by means of consensus, who were aware that the patient had curative resection due to gastric cancer. The lesion at anastomotic site showing mucosal and/or wall thickening with contrast enhancement was considered as locoregional recurrence. Enlarged lymph node (short axis ≥ 10 mm) or contrast enhancing mass was considered as regional, liver or distant recurrence according to the location of lesion. The nodules, loculated fluid collections, or irregular, beaded thickening and stranding of the mesentery or omentum on CECT scans, were considered as findings of peritoneal carcinomatosis.
PET/CT images also were reviewed retrospectively by two experienced nuclear medicine physicians, who were aware that the patient had curative resection due to gastric cancer. The reviewers reached a consensus in cases of discrepancy. FDG PET/CT scans were interpreted visually, and maximum standardized uptake value (SUV) was recorded when abnormal non-physiologic metabolic activity was identified. Quantification of tumor metabolic activity was obtained using the SUV normalized to body weight. Focal hypermetabolic activity of anastomotic site or remnant stomach was considered locoregional tumor recurrence. Focal hypermetabolic activity within the liver which was greater than adjacent normal liver tissue was considered abnormal. Multinodular or diffuse hypermetabolic activities along the intestine or mesentery were considered as findings of peritoneal carcinomatosis. Diffuse or segmental hypermetabolism with mild activity in the intestinal tract was interpreted as a normal physiologic uptake. When abnormal hypermetabolic lesions suggesting secondary malignancy were detected, further evaluations including radiologic and histopathologic examinations were recommended.
Patient and organ based sensitivity, specificity and accuracy were calculated using crosstab tables. McNemar's test was used to analyze the difference between PET/CT and CECT in diagnostic performances. Where applicable, data are presented as mean ± SD. Data were analyzed using descriptive statistics, and changes in continuous variables were analyzed using the independent-samples T test. Tests with P value < 0.05 were considered significant.
During follow-up periods, 28 patients (20.1%) were confirmed having recurrent disease. Thirty-six lesions were confirmed as recurrence (locoregional, n = 7; RegLN, n = 7; liver, n = 4; peritoneal carcinomatosis, n = 11; distant, n = 7).
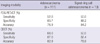
On the patient based analysis, there was no statistically significant difference in the sensitivity, specificity and accuracy of PET/CT (53.6%, 84.7%, and 78.4%, respectively) and those of CECT (64.3%, 86.5%, and 82.0%, respectively) for detecting tumor recurrence except in detection of peritoneal carcinomatosis. On the organ based analysis, PET/CT was more accurate to detect the liver and distant recurrence, but it was not statistically significant. CECT was more sensitive to detect peritoneal carcinomatosis, and it was statistically significant (P = 0.021). The diagnostic performances between two methods were not statistically different except in detection of peritoneal carcinomatosis. The sensitivity, specificity and accuracy according to the recurrent organs are described in Table 1.
Among 36 recurrence lesions, 8 lesions (22.2%) were detected only on PET/CT, and 10 lesions (27.8%) only on CECT (Table 2). Nine lesions (25%) were detected on both PET/CT and CECT, and both methods could not detect the remaining 9 lesions (25%). The mean SUV of gastric anastomotic site was significantly higher in patients with locoregional recurrence (3.4 ± 3.1) than those without locoregional recurrence (1.9 ± 0.7, P < 0.05).
PET/CT had detected 15 lesions which were not related to the recurrence of gastric cancer. Radiologic, endoscopic and histopathologic evaluations had revealed secondary malignancy in 8 patients (colon cancer, n = 4; thyroid cancer, n = 3; prostatic cancer, n = 1) and other benign pathology in 7 patients (active pulmonary tuberculosis, n = 4; chronic thyroiditis, n = 3).
The diagnostic accuracy of PET/CT for detecting the recurrence was not compromised in the patients with histopathologic type of signet-ring cell carcinoma, compared to the patients of adenocarcinoma (Table 3).
The present study showed that PET/CT was as sensitive and specific as CECT in the detection of gastric cancer recurrence except for peritoneal carcinomatosis. Considering that eight recurrent lesions (22.2%) were detected only on PET/CT and secondary malignancy was revealed in 8 patients, additional value of PET/CT was also evident.
The optimal method for assessing early recurrence in patients with gastric cancer is unknown (15). Conventional imaging (ultrasonography, CECT and magnetic resonance imaging) has represented the standard for staging and restaging of gastric cancer (16, 17). Conventional imaging is noninvasive and is the least costly of the available methods, although it has limited value in differentiating post-surgical changes from local tumor recurrence. Therefore, these techniques have limitations for accurate restaging (15, 18).
There have been some reports about the role of FDG PET or integrated PET/CT in the evaluation of gastric cancer recurrence after curative resection. However, their results were inconsistent. Jadvar et al. (10) reported that FDG PET might be useful in the post-therapy evaluation of recurrent disease. Sim et al. (12) and Park et al. (13) also suggested that PET/CT might have a role for detecting recurrence in post-operative patients with gastric cancer. On the other hand, De Potter et al. (19) reported that FDG PET might not be suitable as a primary tool for follow up due to its moderate accuracy.
The diagnostic performance of PET/CT might be compromised for several reasons. First, due to physiological uptake in the bowel, a sufficient tumor-to-background ratio cannot be obtained, especially in small lesions located in the lumen of the alimentary tract, which can be evaluated only by endoscopy. Second, PET/CT has relatively lower sensitivity in detecting peritoneal carcinomatosis because of the small size of the lesions (19, 20). Peritoneal carcinomatosis which is flat and smaller than 1 cm, is very difficult to detect when using the currently available PET hardware with a spatial resolution of 6-8 mm (19). Moreover, the number of patients with peritoneal carcinomatosis was relatively large. In this study population, it was 11/28 (39.3%). Third, it has been reported that signet ring cell carcinoma and mucinous adenocarcinoma showed significantly low FDG uptake (21). As a result, lower sensitivity and accuracy in patients with signet cell carcinoma and mucinous adenocarcinoma, was reported from the studies evaluating primary lesion of gastric malignancy. However, our results were not consistent with these findings, although the number of patients was not large (n = 20).
On the other hand, many metabolically active conditions can cause FDG uptake, thus decreasing the specificity of PET in detecting malignant lesions. These false positive conditions in the abdomen encompass various kinds of physiologic uptakes in the abdominal organs as well as benign pathologic conditions. Physiologic uptakes are commonly found in the gastrointestinal and urinary tracts. Physiologic uptake in the gastrointestinal tract is due to smooth muscle contraction and metabolically active mucosa, whereas that in the urinary tract may be explained by the fact that FDG is not reabsorbed by the renal tubules after glomerular filtration (22).
In spite of these disadvantages of PET/CT, results of this study could encourage the routine use of additional PET/CT on CECT in the evaluation of gastric cancer recurrence after curative resection. In this study, among 36 recurrence lesions, 8 lesions (22.2%) were detected only on PET/CT, and 10 lesions (27.8%) only on CECT. Only 9 lesions (25%) were detected on both PET/CT and CECT. Moreover, PET/CT had revealed unexpected secondary malignancy in 8 patients (colon cancer, n = 4; thyroid cancer, n = 3; prostatic cancer, n = 1) and other benign pathology in 7 patients. These results might be enough to justify clinical role of PET/CT in the detection of gastric cancer recurrence.
This study had enrolled patients whose interval between curative surgical resection and study inclusion was less than 3 yr. This criterion was based on the report of Wu et al. (23). They reported that most (73.5%) recurrences of gastric cancer took place within the first 18 months after surgery, with continued but markedly decreased attribution in the third year. Nearly 90% of the recurrences occurred within 3 yr, and only 7.3% occurred between the third and fifth years. These data suggest that an intense surveillance of recurrence might be needed in the initial 3 yr after surgery.
Our study had several limitations. The first was the retrospective nature of our study. Because of this nature, we were unable to standardize the interval and methods of follow-up imaging studies and gastroscopy. This nature also could cause selection bias, because the patients who had not undergone CECT or PET/CT were excluded. Second, recurrent lesions were not always evaluated histopathologically. Therefore, there was the possibility of including cases in which false-positive lesions were considered as true-positive lesions by imaging follow-up. Finally, our image analysis method was conducted by radiologists and nuclear medicine physicians independently. If additional image analysis using a consensus of both radiologist and nuclear medicine physician was conducted, the clinical role of PET/CT could be revealed more clearly.
In conclusion, despite several limitations, our results revealed that PET/CT is as accurate as CECT in the detection of gastric cancer recurrence after curative resection, except for detecting peritoneal carcinomatosis. Moreover, additional use of PET/CT on CECT could improve detection rate of tumor recurrence and provide other critical information such as unexpected secondary malignancy.
Figures and Tables
Table 1
The diagnostic performance of FDG PET/CT and contrast-enhanced abdominal CT (CECT) according to the recurrence sites

AUTHOR SUMMARY
Detecting the Recurrence of Gastric Cancer after Curative Resection: Comparison of FDG PET/CT and Contrast-Enhanced Abdominal CT
Dae-Weung Kim, Soon-Ah Park and Chang Guhn Kim
In a retrospective review of 139 patients underwent curative resection of gastric cancer, we compared fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) with contrast-enhanced abdominal CT (CECT) for detecting the recurrence of gastric cancer. There was no significant difference in the diagnostic accuracy of PET/CT and that of CECT for detecting tumor recurrence except in detection of peritoneal carcinomatosis (CECT>FDG PET/CT). Among 36 recurrent lesions of 28 patients, 8 lesions and 10 lesions were detected only on PET/CT and CECT, respectively. PET/CT had detected secondary malignancy in 8 patients. PET/CT is as accurate as CECT in the detection of gastric cancer recurrence. Combined application of PET/CT and CECT could improve detection rate and provide other critical information such as unexpected secondary malignancy.
References
1. Sun L, Su XH, Guan YS, Pan WM, Luo ZM, Wei JH, Wu H. Clinical role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in post-operative follow up of gastric cancer: initial results. World J Gastroenterol. 2008. 14:4627–4632.
2. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.
3. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007. 57:43–66.
4. Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y, Okajima K. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy-Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004. 22:2767–2773.
5. Kim KW, Choi BI, Han JK, Kim TK, Kim AY, Lee HJ, Kim YH, Choi JI, Do KH, Kim HC, Lee MW. Postoperative anatomic and pathologic findings at CT following gastrectomy. Radiographics. 2002. 22:323–336.
6. Ha HK, Kim HH, Kim HS, Lee MH, Kim KT, Shinn KS. Local recurrence after surgery for gastric carcinoma: CT findings. AJR Am J Roentgenol. 1993. 161:975–977.
7. Keidar Z, Haim N, Guralnik L, Wollner M, Bar-Shalom R, Ben-Nun A, Israel O. PET/CT using 18F-FDG in suspected lung cancer recurrence: diagnostic value and impact on patient management. J Nucl Med. 2004. 45:1640–1646.
8. Kitajima K, Murakami K, Yamasaki E, Domeki Y, Kaji Y, Sugimura K. Performance of FDG-PET/CT for diagnosis of recurrent uterine cervical cancer. Eur Radiol. 2008. 18:2040–2047.
9. Nogami M, Nakamoto Y, Sakamoto S, Fukushima K, Okada T, Saga T, Higashi T, Senda M, Matsui T, Sugimura K. Diagnostic performance of CT, PET, side-by-side, and fused image interpretations for restaging of non-Hodgkin lymphoma. Ann Nucl Med. 2007. 21:189–196.
10. Jadvar H, Tatlidil R, Garcia AA, Conti PS. Evaluation of recurrent gastric malignancy with [F-18]-FDG positron emission tomography. Clin Radiol. 2003. 58:215–221.
11. Nakamoto Y, Togashi K, Kaneta T, Fukuda H, Nakajima K, Kitajima K, Murakami K, Fujii H, Satake M, Tateishi U, Kubota K, Senda M. Clinical value of whole-body FDG-PET for recurrent gastric cancer: a multicenter study. Jpn J Clin Oncol. 2009. 39:297–302.
12. Sim SH, Kim YJ, Oh DY, Lee SH, Kim DW, Kang WJ, Im SA, Kim TY, Kim WH, Heo DS, Bang YJ. The role of PET/CT in detection of gastric cancer recurrence. BMC Cancer. 2009. 9:73.
13. Park MJ, Lee WJ, Lim HK, Park KW, Choi JY, Kim BT. Detecting recurrence of gastric cancer: the value of FDG PET/CT. Abdom Imaging. 2009. 34:441–447.
14. Yoshioka T, Yamaguchi K, Kubota K, Saginoya T, Yamazaki T, Ido T, Yamaura G, Takahashi H, Fukuda H, Kanamaru R. Evaluation of 18F-FDG PET in patients with advanced, metastatic, or recurrent gastric cancer. J Nucl Med. 2003. 44:690–699.
15. Jensen EH, Tuttle TM. Preoperative staging and postoperative surveillance for gastric cancer. Surg Oncol Clin N Am. 2007. 16:329–342.
16. Chen CY, Hsu JS, Wu DC, Kang WY, Hsieh JS, Jaw TS, Wu MT, Liu GC. Gastric cancer: preoperative local staging with 3D multi-detector row CT-correlation with surgical and histopathologic results. Radiology. 2007. 242:472–482.
17. Kang BC, Kim JH, Kim KW, Lee DY, Baek SY, Lee SW, Jung WH. Value of the dynamic and delayed MR sequence with Gd-DTPA in the T-staging of stomach cancer: correlation with the histopathology. Abdom Imaging. 2000. 25:14–24.
18. Shinya S, Sasaki T, Nakagawa Y, Guiquing Z, Yamamoto F, Yamashita Y. The usefulness of diffusion-weighted imaging (DWI) for the detection of gastric cancer. Hepatogastroenterology. 2007. 54:1378–1381.
19. De Potter T, Flamen P, Van Cutsem E, Penninckx F, Filez L, Bormans G, Maes A, Mortelmans L. Whole-body PET with FDG for the diagnosis of recurrent gastric cancer. Eur J Nucl Med Mol Imaging. 2002. 29:525–529.
20. Lim JS, Yun MJ, Kim MJ, Hyung WJ, Park MS, Choi JY, Kim TS, Lee JD, Noh SH, Kim KW. CT and PET in stomach cancer: preoperative staging and monitoring of response to therapy. Radiographics. 2006. 26:143–156.
21. Kim SK, Kang KW, Lee JS, Kim HK, Chang HJ, Choi JY, Lee JH, Ryu KW, Kim YW, Bae JM. Assessment of lymph node metastases using 18F-FDG PET in patients with advanced gastric cancer. Eur J Nucl Med Mol Imaging. 2006. 33:148–155.
22. Kostakoglu L, Hardoff R, Mirtcheva R, Goldsmith SJ. PET-CT fusion imaging in differentiating physiologic from pathologic FDG uptake. Radiographics. 2004. 24:1411–1431.
23. Wu CW, Lo SS, Shen KH, Hsieh MC, Chen JH, Chiang JH, Lin HJ, Li AF, Lui WY. Incidence and factors associated with recurrence patterns after intended curative surgery for gastric cancer. World J Surg. 2003. 27:153–158.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download