Abstract
Urodynamic evaluation is an invasive and uncomfortable procedure that can cause physical distress and is difficult to perform in uncooperative patients. The aim of this study was to evaluate the effects of consciousness on urodynamic evaluation in an animal model. Repeated cystometry, electromyogram, and measurement of serum cortisol concentrations were performed in female cats under conscious (CON), conscious sedation (CS) and deep anesthesia (DA) conditions. Urodynamic evaluation showed that there were no statistical differences in maximum detrusor pressure or bladder capacity observed among the three conditions. Under the DA condition, but not the CON and CS conditions, bladder contraction was accompanied by an un-relaxed anal sphincter. Residue urine volume significantly increased in the DA condition compared to the CON and CS conditions. The levels of serum cortisol significantly increased after performing urodynamic evaluation under the CON condition, whereas these levels were not significantly increased under the CS and DA conditions. This study showed that conscious sedation has no adverse effects on the urodynamic variables, and that it significantly reduces distress in cats undergoing the examination. These results may provide novel insights for performing urodynamic studies in uncooperative patients.
The basic aim of urodynamics is to reproduce the patient's symptomatic complaints or usual voiding pattern during urodynamics, and to provide a pathophysiological explanation by correlating the patient's symptoms with the urodynamic measurements and observations. In principle, urodynamic study should be performed when the patient is awake and not sedated (1). However, it is difficult to perform urodynamic study in uncooperative patients such as all infants and young children in the awake state, even though the specific adaptations is provided, staff training, environment, parental support, etc. In addition, the examination may induce systemic stress, and therefore can either negatively affect urodynamic results or cause difficulties to correctly analyze the data. Therefore, it is necessary to explore more suitable methodology for performing urodynamic study in uncooperative patients.
Urodynamic study is feasible in animal under awake condition (2). However, numerous studies have shown that urodynamic study, especially the cystometry, were often performed under anesthesia or sedation in various experimental animal models by using different anesthetic agents, because it is difficult to perform urodynamic study in conscious animals (3-6). These studies have demonstrated that if suitable doses and/or classes of anesthetic agents were used, the anesthesia-induced adverse effects on urodynamic results can be minimized, thereby more closely simulate normal physiological responses. In addition, such invasive and uncomfortable procedures, including voiding cystourethrography, oral and maxillofacial surgery and gastrointestinal endoscopy were successfully performed under conscious sedation (7-9). Therefore, the aims of this study were to evaluate the effects of level of consciousness on urodynamic procedure, and the feasibility of performing urodynamic study under conscious sedation by comparison of urodynamic results and the extent of examination-induced systemic stress under conscious, conscious sedation and general anesthesia using an animal model.
Five healthy 2 to 3 yr-old female adult cats weighing 3.0 to 3.5 kg were used in this study. Each of the five cats underwent repeated urodynamic evaluation weekly while conscious (CON) and under conscious sedation (CS) and deep anesthesia (DA) consecutively. While under the CON condition, the cat was placed in a narrow box with a hole for the tail and urethral catheter, and the tail was fixed to the edge of the hole to prevent catheter dislodgment. CS and DA were maintained by subcutaneous injection of 3 mg/kg or 10 mg/kg zoletil (a combination of tiletamine and zolazepam), respectively, because our preliminary study showed that these doses of zoletil effectively maintain CS and DA conditions in cats. The animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) of the Clinical Research Institute at the Seoul National University Hospital (AAALAC accredited facility; IACUC number: 08-0288).
After the cats were positioned and conscious state of each cat was achieved, two 3.5 Fr feeding tubes were inserted into the urinary bladder through the urethra. One tube was used for measuring intravesical pressure (Pves) and the other was used to fill the bladder. A rectal catheter was inserted for measuring abdominal pressure (Pabd). The free ends of the bladder and rectal catheter were connected to pressure transducers and an infusion pump, respectively. For recording the electromyogram (EMG) of the external anal sphincter, two needle electrodes were inserted into the external anal sphincter through both sides of the anus, and a needle ground was inserted subcutaneously into the tail. After the bladder was drained, sterile room temperature saline was infused into the bladder continuously at a rate of 60 mL/h. Intravesical and abdominal pressure as well as the external anal sphincter EMG were continuously recorded, and the detrusor pressure (Pdet, Pdet = Pves-Pabd) was calculated by a computerized system (PowerLab, ADInstruments, Inc., Colorado Springs, CO, USA). When bladder contraction was initiated (Pdet suddenly increased), the filling was stopped and the tube was immediately removed. The other tube connected to the pressure sensor was kept within the bladder for continuous Pves monitoring. The following urodynamic parameters were measured for analysis: bladder capacity (the infused volume immediately before the initiation of micturition), maximum detrusor pressure (Pdet max), and residual urine volume (measured by urethral catheterization).
For measuring serum cortisol concentrations, blood samples were obtained by venipuncture of the vena cephalica antebrachii and collected in a plain vacutainer tube before and immediately after the urodynamic study. Blood samples were centrifuged at 3,000 rpm for 20 min at 4℃, and the separated serum was stored frozen at -80℃ until further use. Serum cortisol levels were determined by a cortisol radioimmunoassay (RIA) kit (DSL-2000 Cortisol RIA kit, Diagnostic Systems Laboratories, Inc., Webster, TX, USA) according to the manufacturers' instructions.
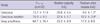
All cats exhibited bladder contractions while under the CON, CS, and DA conditions. There were no statistically significant differences in the maximum detrusor pressure or bladder capacity among animals under the three conditions. The residue urine volume was not statistically different between CON and CS conditions, whereas DA significantly increased the residue urine volume compared to the CON and CS conditions (Table 1, Fig. 1).
With the CON and CS conditions, EMG tracing showed activation of the external anal sphincter during bladder filling. During the voiding phase, the EMG tracing showed decreased and slightly delayed sphincter activity in relation to the onset of bladder contraction. At the same time, a strong urinary stream was observed. With the DA condition, EMG tracing also showed activation of the external anal sphincter during bladder filling. However, activity of the external anal sphincter did not decrease during the voiding phase. At the same time, urine was observed leaking from the urethral orifice (Fig. 1).
In the CON animals, the levels of serum cortisol were significantly increased after performing urodynamic study compared to those observed before the urodynamic study. However, no significant difference was observed when comparing the serum cortisol levels before and after the urodynamic study in cats under the CS and DA conditions (Fig. 2).
Urodynamic study is an invasive and uncomfortable procedure that can initiate physical distress due to discomfort, patient embarrassment, and/or pain induced by genital examination and urethral catheterization (10, 11). The novel finding of the present study is that implementation of urodynamic study on reluctant, conscious subjects or performing the examination on uncooperative patients under DA is inappropriate because these conditions can induce significant systemic stress or detrusorsphincter dyssynergia (DSD). In addition, performing urodynamic evaluation on subjects under CS can minimize examination-induced stress while closely simulating normal physiological responses. The present study demonstrated that performing urodynamic studies on reluctant, conscious subjects induces significant increases in systemic stress as shown by increased serum cortisol levels. Cortisol is an important hormone in the body that is secreted by adrenal glands. It is frequently used in various experimental settings as an objective marker when evaluating psychological and laboratory stress (12, 13). Although it remains unclear whether systemic stress induced by urodynamic evaluation adversely influences the examination results, it is necessary to reduce examination-induced systemic stress from an ethical point of view. In the present study, the serum cortisol levels were unchanged under the CS and DA conditions. These results suggest that CS and DA are useful approaches for reducing stress induced by urodynamic evaluation.
Physiologically, the micturition reflex is coordinated by the central, autonomic, and somatic nervous systems. The muscles involved in micturition are controlled by the autonomic and somatic nervous systems. During the storage phase, the urethral sphincter contracts and the detrusor muscle is relaxed by sympathetic stimulation. During micturition, the detrusor muscle contracts and the urethral sphincter is relaxed by parasympathetic stimulation. The micturition reflex is altered by anesthetics, which could cause inhibition of micturition, direct loss of coordination between the detrusor muscle and urethral sphincter, and an imbalance of sympathetic and parasympathetic control of micturition (6). However, several studies have demonstrated that the influence of anesthesia on urodynamic evaluation is dependent on the class of anesthetic agents and degree of anesthesia (3-5). The present study supported these findings and provided new data on the feasibility of performing urodynamic studies of CS subjects. In the present study, the urodynamic evaluation showed that there were no statistical differences in the maximum detrusor pressure and bladder capacity among animals under the three conditions. In addition, bladder contraction accompanied by un-relaxed sphincter activity occurred under the DA condition, whereas the CS condition did not affect the coordination between bladder contraction and external anal sphincter activation. As a result, the residual urine volume was significantly increased under the DA condition. In contrast, the residual urine volume was similar under the CON and CS conditions. These results suggest that CS has no significant adverse effect on urodynamic variables. We also believe that the large residual urine volume observed under CON condition was due to the obstructive effect of the catheter even though a smaller-sized catheter was used.
The American Society of Anesthesiologists has defined four levels of sedation: minimal, moderate, deep, and general anesthesia (14). In the first two categories, cardiorespiratory function is maintained, the cognitive function and coordination are somewhat impaired, and patients can cooperate with the examiner and respond normally to verbal stimulation. The selection of a suitable anesthetic agent is important for the induction and maintenance of sedation. Zoletil, a combination of tiletamine and zolazepam, produces dose-dependent sedation up to general anesthesia (15). It is used for anesthesia in various species of animals such as dogs, cats, and wild and captive animals, and provides rapid induction, excellent muscle relaxation with a wide safety margin, and a smooth recovery. In the present study, subcutaneous injection of 3 mg/kg zoletil provided a sufficient period to perform the urodynamic study. This dose of zoletil produced hypnosis within 3 min of injection, and the cats recovered approximately 30 min after the injection. In addition, 10 mg/kg zoletil induced DA during which continuous regular breathing pattern was maintained without intubation within 5 min of injection and lasted for approximately 2 hr. These findings along with the results of the urodynamic study suggest that zoletil is an appropriate anesthetic agent for urodynamic studies conducted in female cats.
There are limitations associated with the present study. First, a complete urodynamic evaluation was not performed in this study. Therefore, whether other factors of a complete urodynamic study such as pressure flow and a urethral pressure profile could be evaluated in subjects under the CS condition remains to be elucidated. Another limitation of this study is that a single anesthetic agent was used. The suitability of other anesthetic agents, especially the most commonly administered sedatives such as propofol and midazolam, remain unclear. Further studies are required to address these issues.
In conclusion, the results of this study provide evidence that CS has no adverse effects on urodynamic variables, and that it significantly reduces distress in cats undergoing examination. These results may provide novel insights for performing urodynamic studies in uncooperative patients.
Figures and Tables
 | Fig. 1Urodynamic study. Representative traces of cystometrogram and electromyogram (EMG) of the external anal sphincter under conscious, conscious sedation and deep anesthesia conditions. Pves, intravesical pressure; Pabd, abdominal pressure; Pdet, detrusor pressure. |
AUTHOR SUMMARY
Effects of Level of Consciousness on Urodynamic Procedure in Female Cats
Wen Ji Li, Jong Min Kim and Seung-June Oh
Urodynamic evaluation is an invasive and uncomfortable procedure that can cause physical distress and is difficult to perform in uncooperative patients. Therefore, it is necessary to explore suitable methodology for performing urodynamic study in uncooperative patients. In this study, we investigated whether performing urodynamic evaluation is appropriate under conscious sedation in female cat model. We found that conscious sedation has no adverse effects on the urodynamic variables, and that it significantly reduces distress in cats undergoing the examination. Our results may provide novel insights for performing urodynamic studies in uncooperative patients in real clinical setting.
References
1. Blaivas J, Chancellor MB, Weiss J, Verhaaren M. Atlas of Urodynamics. 2007. 2nd ed. Blackwell;25.
2. Park SH, Jin LH, Kwon YH, Yoon SM, Ryu JK, Lee T. Application and limitations of awake cystometry in Sprague-Dawley rats with partial bladder outlet obstruction as a model of overactive bladder or obstruction. Korean J Urol. 2009. 50:486–492.
3. Cohen TA, Westropp JL, Kass PH, Pypendop BH. Evaluation of urodynamic procedures in female cats anesthetized with low and high doses of isoflurane and propofol. Am J Vet Res. 2009. 70:290–296.
4. Chang HY, Havton LA. Differential effects of urethane and isoflurane on external urethral sphincter electromyography and cystometry in rats. Am J Physiol Renal Physiol. 2008. 295:F1248–F1253.
5. Cannon TW, Damaser MS. Effects of anesthesia on cystometry and leak point pressure of the female rat. Life Sci. 2001. 69:1193–1202.
6. Ghoniem GM, Shoukry MS, Monga M. Effects of anesthesia on urodynamic studies in the primate model. J Urol. 1996. 156:233–236.
7. Merguerian PA, Corbett ST, Cravero J. Voiding ability using propofol sedation in children undergoing voiding cystourethrograms: a retrospective analysis. J Urol. 2006. 176:299–302.
8. Tosun Z, Aksu R, Guler G, Esmaoglu A, Akin A, Aslan D, Boyaci A. Propofol-ketamine vs propofol-fentanyl for sedation during pediatric upper gastrointestinal endoscopy. Paediatr Anaesth. 2007. 17:983–988.
9. Lee JS, Gonzalez ML, Chuang SK, Perrott DH. Comparison of methohexital and propofol use in ambulatory procedures in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2008. 66:1996–2003.
10. Ku JH, Kim SW, Kim HH, Paick JS, Son H, Oh SJ. Patient experience with a urodynamic study: a prospective study in 208 patients. J Urol. 2004. 171:2307–2310.
11. Doshani A, Mayne C, Tincello D. Anxiety among women attending urodynamic investigation: scoping study for a randomized trial of psychometric intervention. Neurourol Urodyn. 2009. 28:177–178.
12. Willemse T, Vroom MW, Mol JA, Rijnberk A. Changes in plasma cortisol, corticotropin, and alpha-melanocyte-stimulating hormone concentrations in cats before and after physical restraint and intradermal testing. Am J Vet Res. 1993. 54:69–72.
13. Yoder B, Wolf JS Jr. Canine model of surgical stress response comparing standard laparoscopic, microlaparoscopic, and hand-assisted laparoscopic nephrectomy. Urology. 2005. 65:600–603.
14. Committee on Drugs. American Academy of Pediatrics. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: addendum. Pediatrics. 2002. 110:836–838.
15. Lee CC, Lin YY, Hsu CW, Chu SJ, Tsai SH. Movement disorder caused by abuse of veterinary anesthesia containing tiletamine. Am J Emerg Med. 2009. 27:1022e5–e6.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download