Abstract
This study aimed to assess the immune status of the Korean population against hepatitis A virus (HAV). Residual serum samples from 2008 to 2010 were collected from diagnostic laboratories and a total of 1,872 samples were analyzed. Anti-HAV seroprevalence was 57.3% in subjects aged 1-4 yr, 69.8% at 5-9 yr and decreased to 38.8% at 10-14 yr, 13.0% at 15-19 yr, and 11.7% at 20-29 yr. Seroprevalence increased with increasing age: 52.2% at 30-39 yr, 83.2% at 40-49 yr, 81.4% at 50-59 yr, 93.2% at 60-69 yr, and 95.1% at 70-79 yr. The most susceptible age group consisted of subjects aged 10-29 yr, especially those aged 20-29 yr. This pattern is markedly different from that in the past 3 decades, where the most susceptible group had consisted of children aged less than 10 yr and almost all subjects aged more than 20 yr had developed anti-HAV antibodies. Because of improvements in hygiene and introduction of hepatitis A vaccine, the age demographic of the susceptible population has shifted. These data are important for creating new prevention measures, including vaccination policies, to prevent and control outbreaks of hepatitis A in Korea.
Hepatitis A occurs throughout the world with major differences in geographical endemicity and clinical characteristics (1). The patterns of hepatitis A virus (HAV) infection are closely related with hygiene and socioeconomic status. Over the past several decades, the epidemiology of hepatitis A has shown dynamic changes in Korea. Up to the early 1980s, Korea was classified as a high endemic country, with most cases occurring in young children (2-4). With improvements in sanitation and socioeconomic conditions, opportunities for exposure decreased, leading to an increase in susceptible populations among adolescents and young adults. This resulted in several outbreaks since 1996 (5-7). Korea is currently at a transitional status from a high to low endemicity, resulting in an increase of disease burden on public health.
Fortunately, a safe and highly efficacious vaccine exists for hepatitis A, providing an opportunity to lower disease incidence and potentially eliminate infection (3). In Korea, the vaccine was first introduced in 1997 and has been recommended for high-risk groups and is currently recommended in children over 12 months of age. Although hepatitis A vaccine is not yet included in the national immunization program, the number of vaccinated people is increasing with the growing social recognition of the disease.
To develop appropriate immunization strategies an integrated evaluation of the epidemiology of hepatitis A is important. In this study, we aimed to evaluate the seroprevalence of hepatitis A in Korea in order to assess the immune status of the Korean population and find susceptible age groups. We also reviewed previous seroprevalence studies performed in the past 30 yr to enhance our understanding of the dynamics of these changing epidemiology.
Sera were collected from two diagnostic laboratories located in Seoul, Korea. One laboratory has a network of laboratories located in provinces throughout Korea. Residual serum samples after diagnostic testing, which would otherwise have been discarded were collected. Sera referred for the diagnosis of infectious diseases such as measles, mumps, rubella, hepatitis A and HIV were excluded.
Samples were collected from February 2008 to March 2010. In order to keep anonymity, subject information was deleted and sera were assigned with a new code number. The only demographic characteristics available were age, gender, district of laboratory and date of sampling.
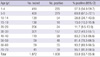
Serum samples were collected from subjects aged 1-79 yr. Samples were stratified into the following age groups: 1-4, 5-9, 10-14, 15-19, 20-29, 30-39, 40-49, 50-59, 60-69, and 70-79 yr. Subjects from 1-9 yr of age were also analyzed in 1 yr unit, and seroprevalence was analyzed by 2 yr unit in subjects 10-29 yr.
The sample size was calculated using the following equation:
n=z2α/2p(1-p)/d2
zα/2: 1.96 standard deviation, d: precision (=confidence interval/2), p: prevalence, α: type I error.
Prevalence was based on a previous report of seroprevalence of hepatitis A antibodies in Korea (8).
Serum samples were tested to detect anti-HAV (Elecsys® 2010/Modular analytics E170, Roche Diagnostics GmbH, Indianapolis, IN, USA).
We searched the MEDLINE, KoreaMed, and the Korean Medical Database for studies of hepatitis A seroprevalence in Korea. The search included terms in the title or key words 'Hepatitis A', 'Seroprevalence', and 'Hepatitis A vaccine'. A manual search was also done on studies referenced in publications identified through the initial search.
We reviewed all studies that reported seroprevalence against hepatitis A in Korean subjects. Studies of seroprevalence in selected age groups or populations such as soldiers, police officers, hospital personnel etc. were excluded. Studies regarding patients with acute or chronic liver disease were also excluded. Data from each of the studies with a similar age classification of our study were extracted by age group for comparison.
A total of 2,061 sera were collected; of these, 1,872 of sufficient amount were tested. Among the sera tested, 43.7% (818/1,872) were from male patients, and there was no difference in seroprevalence between gender groups (male 54.4%, female 52.0%). Seropositivity according to age group is shown in Table 1. The total seroprevalence against HAV was 53.8%. When analyzed according to age, the seroprevalence showed a sinusoidal wave pattern (Fig. 1). In subjects aged less than 10 yr, seropositivity was also separately analyzed by 1 yr unit. Seropositivity in infants was 26.3% and increased to 56.3%-83.9% in children 2-9 yr of age. The seropositivity in subjects aged 10-11 yr was 38.8% and decreased to 9.5% in subjects of the early twenties. Seropositivity then gradually increased from 43.3% in subjects aged 30-34 yr to 60.9% in subjects aged 35-39 yr, 83.2% in subjects aged 40-49 yr, and 95.1% in subjects aged 70-79 yr.
The data from studies performed in Korea were reviewed (Table 2) (7-21). Patterns in seroprevalence according to age groups showed distinct changes over the past 30 yr (Fig. 2) (8, 9, 15). Fig. 2A shows changes in seroprevalence over different periods of time (10-yr intervals) according to age group. From 1979 to 1981, almost all subjects over 20 yr of age were seropositive against HAV. At that time, in subjects younger than 20 yr of age, seroprevalence increased with age: 22% at 1-4 yr old, 59.1% at 5-9 yr old and 87% at 10-19 yr of age. Ten years later, from 1988 to 1989, the seropositive rate gradually decreased in children and adolescents under 20 yr of age. This decrease in seroprevalence continued during the following 10 yr in 1996-1997 along with a subtle decrease in seropositive rates in subjects 20-29 yr of age. In 2006, the seroprevalence pattern showed changes in the 1-4 and 5-9 yr old age groups: an increase from 7% to 55.6% in subjects aged 1-4 yr and from 2% to 47.2% in subjects aged 5-9 yr. However, in subjects older than 10 yr old, the decreasing trend in seroprevalence continued with an especially sharp decline in seroprevalence among subjects 20-29 yr of age.
The differences in seroprevalence among age groups over the past 30 yr are shown in Fig. 2B. The seroprevalence curve in 1979-1981 shows a steep increase in seropositivity among subjects aged 1-4 yr up to 20 yr. In 1988-1989, subjects in the 1-4 and 5-9 yr age groups showed a subtle increase in seropositivity compared with that 10 yr before (in 1979-1981); however seropositivity again showed significant increase in the 10-19 yr old group. In 1996-1997, seropositivity among subjects 5-9 yr of age was lower than that among subjects 1-4 yr of age, and the seroprevalence curve showed a U pattern. This pattern changed to a sinusoidal shape in 2006 and again in 2008-2010. Another important finding is that over the past 30 yr, the seroprevalence curve shifted toward the right, showing a change in susceptible age group for infection from children under 10 yr of age to subjects 10-29 yr of age.
There has been a clear change in seroprevalence patterns in Korea over the past 30 yr. The susceptible population has changed from subjects under 10 yr of age to subjects 10-29 yr of age. The susceptible proportion of subjects aged 30-39 yr and 40-49 yr is also gradually increasing. The changes in seroprevalence coincide with several environmental factors. A main influencing factor is that the socioeconomic status of Korea has shown steady improvement over the past 30 yr, accompanied by an improvement in individual and social hygiene. Considering that hepatitis A is transmitted through the fecal-oral route, either by person-to-person contact or by ingestion of contaminated food or water, improvements in sanitation has led to big changes in the epidemiology of this disease in Korea. The epidemiology of hepatitis A can be classified into high, intermediate, low, and very low endemicity (1, 3). In areas of high endemicity, infection generally occurs in early childhood, when most cases can be asymptomatic or unrecognized, and most of the population is infected before reaching adolescence (22). The seroprevalence pattern in 1979-1981 in Korea represents typical characteristics of a high endemic area. In areas of intermediate endemicity, improvements in sanitation and living conditions leads to lower transmission of HAV and the predominant age group of infection consists of school-aged children, adolescents, and young adults. Paradoxically, the overall incidence of reported cases is often higher than that in highly endemic areas because the susceptible population is more likely to develop symptoms of HAV infection. Large outbreaks occur because of high rates of virus transmission and large numbers of susceptible persons. Seroprevalence curves from 1996 to 1997 and afterwards in Korea reflect changes toward an intermediate endemic area. In low endemic countries, disease incidence is generally low, and many cases are associated with travelers from regions of high or intermediate endemicity.
Another important factor regarding the change in prevalence patterns is the introduction of the hepatitis A vaccine in Korea. The seroprevalence pattern changed from a U shape to a sinusoidal shape with an increase in percentage of children under 10 yr old with anti-hepatitis A antibody. After introduction of the hepatitis A vaccine in Korea in 1997, high-risk groups were vaccinated, and children over 12 months of age were immunized on a private basis. With the introduction of the hepatitis A vaccine, seroprevalence increased from 7% to 57.3% in subjects 1-4 yr of age and from 2% to 69.8% in subjects 5-9 yr of age from 1996-1997 to 2008-2010.
The changes observed in hepatitis A seroprevalence patterns reflect the changes in hepatitis A disease patterns in Korea. Since the large epidemic in Daejeon (13), outbreaks are continuing in the country. Data regarding population-based incidence is limited in Korea; however hepatitis A is included in the national sentinel surveillance system which was started in 2001. According to the surveillance system, 312-355 cases were reported in 2002-2004. The number of cases doubled to 798 in 2005, increased to 2,081-2,233 in 2006-2007, 7,895 in 2008, and 15,231 in 2009. When stratified by age group, cases increased throughout all age groups with only a subtle increase in children 0-9 yr of age. However, the number of cases involving 20- to 29-yr-olds increased from 147 (2002) to 5,665 (2009) and those involving 30- to 39-yr-olds increased from 77 (2002) to 6,608 (2009). In 2009, the number of cases in 40- to 49-yr-old patients also increased from 21 cases (2002) to 1,605 cases. In our seroprevalence study, we found that 88.3% of subjects 20-29 yr of age were antibody negative. In addition, almost 50% of patients 30-39 yr of age and nearly 20% of subjects in the 40-49 and 50-59 age groups were also antibody negative. Therefore, public health measures are required for not only the young population but also subjects over 40 yr of age.
The present study has some limitations. First, sera from diagnostic laboratories were collected anonymously; therefore, demographic factors, including socioeconomic status, education, high-risk activities (alcoholic or drug history, sexual activity, etc.), nationality, and crowding index, were not collected. It is necessary to conduct a seroprevalence study on hepatitis A with these information included because to the best of our knowledge, no studies, including demographic analyses, have been performed in Korea. In addition, 75% of the samples were retrieved from urban centers in Seoul, Incheon, and Gyeonggi-do. Most laboratory institutions from other provinces are located in an urban area, not in a rural district. Hepatitis A seroprevalence reflects immunity acquired either through infection or immunization, which can differ between regional areas; therefore, these factors should be considered when interpreting the results. In a national survey conducted in 2007 among children 12 months to 6 yr of age, the overall vaccination rate for hepatitis A vaccine was 39.4%, with a regional range from 12% (Chungcheongbuk-do) to 59.5% (Ulsan Metropolitan City) according to district (unpublished data). Considering that most of the samples were collected from urban districts, the seroprevalence data might be underestimated in older age groups (which reflects previous infection) or overestimated in younger age groups (which reflects an opportunity of or interest in vaccination) compared to the general population. In addition, differences between regional areas were not analyzed because of limited availability of samples from various regions. However, the present study included subjects 1-79 yr of age and samples were collected randomly. Therefore, although the data of this study might not be representative of the general population, it provides insight into the current pattern of immunity against hepatitis A. In previous studies performed in Korea, data differed according to study population and age classification. However, a review of the data showed a distinct shift in seroprevalence patterns; this enhances the comprehension of epidemiologic changes among subjects from 1 to over 40 yr (up to the late 70s) and through the decades by comparing studies performed at different periods of time. Moreover, we could see the impact of the hepatitis A vaccine by comparing data from the pre- and post-vaccine period.
To control a vaccine-preventable disease, it is important to identify the population groups susceptible to infection. This can be done by surveillance of the disease, including the incidence, age distribution of patients, and regional differences. In addition, identifying the characteristics and risk factors of the disease population is important in disease control and prevention. Another important method is conducting a seroprevalence study comparing age groups and regions, in which patterns of particularly susceptible groups can be observed. A seroprevalence study reflects current and previous vaccination policies, and by confirming susceptible age groups, seroprevalence studies provide invaluable information required for determining national immunization policies and preventing continuous epidemics. In high endemic areas, universal immunization is not recommended because clinical hepatitis A is usually a minor public health problem and most children under 10 yr of age experience asymptomatic infections. In areas of intermediate endemicity, widespread vaccination in children and adolescents controls hepatitis A infections, whereas in low endemic areas, vaccination in high-risk populations is recommended (23). Through this seroprevalence study, it is found that Korea is at a status of intermediate endemicity; therefore, a universal vaccination program would be advisable.
Figures and Tables
 | Fig. 2Changes of seroprevalence against hepatitis A in Korea from 1979 to 2010 (data from reference no. 8, 9, 15). (A) Changes over different periods (10-yr intervals) according to age group, (B) Changes among age groups over the past 30 yr. |
AUTHOR SUMMARY
Seroepidemiology of Hepatitis A in Korea: Changes over the Past 30 Years
Hyunju Lee, Hye Kyung Cho, Jong-Hyun Kim and Kyung-Hyo Kim
We evaluated the seroprevalence of hepatitis A (HAV) to assess the immune status of the Korean population and find susceptible age groups. Residual serum samples from diagnostic laboratories were collected from 2008 to 2010. The seroprevalence of anti-HAV was 57.3% in subjects 1-4 yr, 69.8% in 5-9 yr and decreased to 38.8% in 10-14 yr, 13.0% in 15-19 yr and was lowest in the 20-29 yr age group by 11.7%. Seroprevalence increased with advancing age; 52.2% in 30-39 yr, 83.2% in 40-49 yr, 81.4% in 50-59 yr, 93.2% in 60-69 yr and 95.1% in 70-79 yr. The susceptible age group proved to be 10-29 yr age, especially 20-29 yr age. Related with improvements in hygiene and introduction of hepatitis A vaccine, there has been a shift in age groups of the target susceptible population.
References
1. Bell BP, Feinstone SM. Plotkin SA, Oreinstein WA, editors. Hepatitis A Vaccine. Vaccines. 2004. 4th ed. Philadelphia, PA: Saunders;269–297.
2. Kim JH. Recent epidemiological status and vaccination of hepatitis A in Korea. J Korean Med Assoc. 2008. 51:110–118.
3. Center for Disease Control and Prevention (CDC). Prevention of hepatitis A through active or passive immunization: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1999. 48:1–37.
4. Lee BC, Lee DB. Clinical observation of type A hepatitis in children. J Korean Pediatr Soc. 1979. 22:213–222.
5. Kim NJ, Sung JK, Lee SW, Lee KT, Lee SM, Kim SH, Lee BS, Kim JH, Yu JH, Lee HY. An outbreak of hepatitis A in Taejeon city. Korean J Gastroenterol. 1999. 34:205–212.
6. Han SH, Lee SH, Roh BJ, Shim SC, Cho SC, Sohn JH, Lee DH, Kee CS. An outbreak of hepatitis A in South Korean military personnel: a clinical and epidemiologic study. Korean J Hepatol. 2001. 7:392–400.
7. Choi W, Eom HS, Kim IH, Lee DH, Kim PS, Kim HG, Kwon KS, Cho HG, Shin YW, Kim YS. Patterns of acute hepatitis A and anti-HAV seroprevalence of Kyungin province. Korean J Gastroenterol. 1999. 34:69–75.
8. Kim JH, Kang JH, Lee SY, Choi HA, Kim HM, Seoh K, Choi JY, Park SK, Bae GR, Goh EY. A study for seroprevalence of antibody to hepatitis A in Korea. Korean J Hepatol. 2007. 13:Suppl 3. S27.
9. Hong WS, Kim CY. Seroepidemiology of type A and type B hepatitis in Seoul area. Korean J Intern Med. 1982. 25:19–26.
10. Kim TW, Lee KJ. Antibody to hepatitis A antigen in children and adolescents in Korea. J Korean Pediatr Soc. 1982. 25:36–40.
11. Lee JI, Kim JY, Kim ST, Yoo SY, Chung SM, Kim YK, Lee BH. Epidemiologic study of antibody to hepatitis A antigen in Choong Chung area. Korean J Gastroenterol. 1982. 14:87–91.
12. Lim DS, Cho KH, Kim HC. Seroepidemiological study of anti-HAV antibody in Cheon-Buk province in 1989. Korean J Intern Med. 1992. 43:57–65.
13. Lee KY, Song KH, Kang JH. Seroepidemiology of hepatitis A in Taejon, Korea 1996. J Korean Pediatr Soc. 1998. 41:53–61.
14. Sohn YM, Rho HO, Park MS, Park JH, Choi BY, Ki M, Jang WI. The changing epidemiology of hepatitis A in children and the consideration of active immunization in Korea. Yonsei Med J. 2000. 41:34–39.
15. Park CH, Cho YK, Park JH, Jun JS, Park ES, Seo JH, Lim JY, Woo HO, Youn HS, Ko GH, Kang HL, Baik SC, Lee WK, Cho MJ, Rhee KH. Changes in the age-specific prevalence of hepatitis A virus antibodies: a 10-year cohort study in Jinju, South Korea. Clin Infect Dis. 2006. 42:1148–1150.
16. Kim TY, Sohn JH, Ahn SB, Son BK, Lee HL, Eun CS, Jeon YC, Han DS. Comparison of recent IgG anti-HAV prevalence between two hospitals in Seoul and Gyeonggi area. Korean J Hepatol. 2007. 13:363–369.
17. Kwon YO, Choi IJ, Jung JW, Park JH. An epidemiologic study on the seropositive rate of hepatitis A virus among a selected group of children and adults in Busan. Korean J Pediatr. 2007. 50:262–267.
18. Choi HJ, Lee SY, Ma SH, Kim JH, Hur JK, Kang JH. Age related prevalence of antibodies to hepatitis A virus performed in Korea in 2005. Korean J Pediatr Infect Dis. 2005. 12:186–194.
19. Song YB, Lee JH, Choi MS, Koh KC, Paik SW, Yoo BC, Choi YH, Sohn HJ, Lee KH, Rhee JC. The age-specific seroprevalence of hepatitis A virus antibody in Korea. Korean J Hepatol. 2007. 13:27–33.
20. Lee D, Ki M, Lee A, Lee KR, Park HB, Kim CS, Yoon BY, Kim JH, Lee YS, Jeong SH. A nationwide seroprevalence of total antibody to hepatitis A virus from 2005 to 2009: age and area-adjusted prevalence rates. Korean J Hepatol. 2011. 17:44–50.
21. Moon HW, Cho JH, Hur M, Yun YM, Choe WH, Kwon SY, Lee CH. Laboratory characteristics of recent hepatitis A in Korea: ongoing epidemiological shift. World J Gastroenterol. 2010. 16:1115–1118.
22. Smith PF, Grabau JC, Werzberger A, Gunn RA, Rolka HR, Kondracki SF, Gallo RJ, Morse DL. The role of young children in a community-wide outbreak of hepatitis A. Epidemiol Infect. 1997. 118:243–252.
23. Hepatitis A vaccines. Wkly Epidemiol Rec. 2000. 75:38–44.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download