Abstract
This study was conducted to evaluate the influence of alcohol consumption on the risk of ocular trauma. We retrospectively reviewed the medical records of 1,024 patients who visited emergency department and received ophthalmologic examination from January 1 to December 31, 2009. The patients were divided into 2 groups: those with ocular trauma (n = 494) and those without (n = 530); the influence of alcohol consumption was compared between these 2 groups. In the ocular trauma group, the association of the causes and types of ocular trauma with alcohol consumption was evaluated. One of 530 patients of no trauma group and 117 (23.7%) of 494 patients of trauma group were related with alcohol intake, and the difference was statistically significant (P < 0.001). Concerning the causes, physical assault was significantly more common in alcohol-associated injury (P < 0.001). Regarding the types of injury, orbital wall fracture and hyphema showed a significant association with alcohol consumption (P < 0.001). Older age and nighttime injury were significantly related to the increased risk of alcohol-associated ocular trauma (P = 0.018 and < 0.001, respectively). In conclusion, alcohol consumption significantly increases the risk of ocular trauma.
Alcohol intake has been shown to potentiate aggressive behavior as a psychomotor stimulant (1). Previous studies have demonstrated that alcohol consumption increases the risk of both trauma by physical assault and accidental trauma (2, 3). Therefore, alcohol consumption can conceivably increase the risk of ocular trauma. However, to the best of our knowledge, only a few studies have elucidated the impact of alcohol consumption on ocular trauma (4, 5). In Korea, 87.6% of adults are reported to have drunk alcohol, which is much higher compared to USA (64.9%) and Canada (72.3%) (6). Therefore, we believe that the influence of alcohol consumption on ocular trauma should be investigated. The purpose of this study was to evaluate the influence of alcohol consumption on ocular trauma in Korea.
We retrospectively reviewed the medical records of 1,024 consecutive patients who presented at the emergency department of Seoul National University Bundang Hospital for ophthalmologic examination between January 1, and December 31, 2009. Among them, the patients with ocular trauma were chosen, and the causes of the injury were studied. In each subject, whether the patient was in drunken state at the time of ocular trauma or not was documented. In the case of trauma by physical assault, it was also evaluated whether the assailant was in drunken state or not. If the patient or attacker was in an inebriated state, the case was defined as an alcohol-associated injury. Ocular trauma due to traffic accident caused by drunken driver was also defined as an alcohol-associated injury. Alcohol consumption was determined by asking to the patients or companions. The influence of alcohol was compared between patients who suffered trauma and those who did not using Fisher's exact test. Among those who suffered trauma, the association of the causes and types of ocular trauma with alcohol consumption was evaluated using Pearson's chi-square test and linear-by-linear association, as appropriate. The causes of ocular trauma were re-classified into assault and non-assault, and the association of the cause and alcohol consumption was re-analyzed; the odds ratio was calculated using chi-square test. The influence of demographic factors including gender and age, and the time of injury (nighttime [6 pm to 6 am] vs daytime [6 am to 6 pm]) on the risk of alcohol-associated ocular trauma was analyzed using chi-square test, linear-by-linear association and Student's t-test, as appropriate.
SPSS software for Windows (V15.0; SPSS Inc, Chicago, IL, USA) was used in every statistical analysis. A P value of less than 0.05 was considered statistically significant.
The study population comprised 647 (63.2%) male and 377 (36.8%) female patients. The mean age was 34.9 ± 20.5 yr (range, 0-90). Of the 1,024 patients, 494 (48.2%) sustained ocular trauma, including 373 (75.5%) male and 121 (24.5%) female patients. The mean age was 34.2 ± 19.0 yr (range, 11-81).
Of the 494 subjects with ocular trauma, 117 (23.7%) patients had alcohol-associated ocular injuries, while only one (0.2%) of 530 patients with ocular diseases other than ocular trauma was associated with alcohol drinking at presentation (P < 0.001).
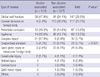
There was a significant difference in the causes of ocular trauma between groups with and without alcohol-association (P < 0.001, Table 1). Assault was the most common cause (76.1%, 89/117) of alcohol-associated ocular trauma, whereas it was the least common cause (11.1%, 42/377) of non-alcohol-associated ocular trauma (odds ratio [OR], 25.4; 95% confidence interval [CI]: 14.9-43.2; P < 0.001).
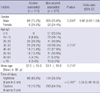
The types of ocular injuries were also different between the alcohol-associated and non-alcohol-associated groups (Table 2). Orbital wall fracture and complex injuries were more common in the alcohol-associated group than the non-alcohol-associated group (47.9% vs 24.1%; 17.9% vs 2.4%), and most of the complex injuries were the combination of orbital wall fracture and hyphema. Among 21 cases of complex injuries associated with alcohol consumption, orbital wall fracture was most frequently found (21 cases, 100%), followed by hyphema (19 cases, 90.5%). Details of the types of ocular trauma are summarized in Table 2.
Regarding the demographic factors, no significant difference in the gender ratio was observed between the alcohol-associated group and the non-alcohol-associated group. However, the mean age was significantly older in the alcohol-associated group than in the non-alcohol-associated group (37.6 ± 15.0 yr vs 33.1 ± 19.9 yr, P = 0.010). Linear-by-linear association also demonstrated the significant difference in the age distribution between the two groups (P = 0.018). The significant difference in the time of injury between the two groups was also found. Alcohol-associated ocular injuries were substantially more common in nighttime, whereas non-alcohol-associated ocular injuries occur more frequently in daytime (OR, 9.34; 95% CI: 5.48-16.0; P < 0.001). Details of the influence of demographic factors and the time of injury on the risk alcohol-associated ocular trauma are summarized in Table 3.
The known risk factors of ocular trauma include male gender, laborer, rural setting, and lower education level (5, 7-10). There has been a few reports describing the association of alcohol consumption with ocular trauma (4, 5). Smith et al. (4) demonstrated that 76.2% of all assaults were alcohol-related in Australian patients. The present study showed the similar result that 67.9% (89/131) of assaults were related with alcohol, suggesting that increased violence due to alcohol consumption is also an important cause of ocular trauma in Asians (4). Loon et al. (5) recently reported that alcohol consumption was associated with a history of having ocular injury. However, a limitation of the study was that they had only investigated a history of alcohol consumption as a lifestyle habit, and the state of inebriation at the time of injury was never documented. Besides, as the authors pointed out, alcohol consumption might have been underreported because of religious restrictions (5). In the present study, we demonstrated the direct impact of alcohol consumption on ocular trauma by investigating the state of inebriation at the time of ocular injury.
In the present study, alcohol-associated injuries were most frequently caused by assault, followed by daily activity. The finding is in good agreement with the results of the previous studies that alcohol consumption is more common in assault or intentional injury (2, 3). Overall, alcohol consumption was found to be associated with one-fourth of all ocular traumas in Korea, this may be because social drinking is very prevalent in the Korean society (6).
Alcohol-associated injuries are more frequently associated with orbital wall fractures and complex injuries, most of which are a combination of orbital wall fracture and hyphema (Table 2). This finding can be explained by the fact that most cases of physical assault involve blunt trauma inflicted by fist or foot; this is especially true in countries such as Korea where civilians cannot legally carry guns. Lee et al. (3) revealed that blunt trauma including fracture, bruises, and open wound occurs more frequently in alcohol-dependent drinkers, supporting the results of our study. In addition to physical assault because of alcohol consumption, collapse of individuals in an inebriated state or accidents while driving in drunken state can lead to ocular trauma. Lee et al. (2) demonstrated that trauma associated with alcohol consumption was significantly more common in male than female, and in nighttime injuries than daytime injuries, which corresponds well with our results that nighttime is associated with the increased risk of alcohol-associated ocular trauma (Table 3). It is probably due to the difference in the causes of the injury. Alcohol-associated ocular trauma is more frequently related to assault in drunken state, which usually occurs in the nighttime (2, 3). By contrast, non-alcohol-associated ocular trauma is more common in injuries related to sports, work or daily activities, which occurs more often in the daytime (Table 1). However, our results show that male gender does not increase the risk of alcohol-associated ocular injury (Table 3). It is conceivably because male gender increases the risk of ocular trauma by non-alcohol-associated injury as well as that by alcohol-associated injury. Male gender is a well-known risk factor of ocular trauma, as men are more frequently exposed to violence and danger in workplace or outdoor activities (11-13). The difference in the age distribution is probably due to the fact that legal drinking age is 19 yr old in Korea, thus youngsters under that age have limited chance to be exposed to alcohol. The difference in the proportion of the patients ≤ 19 yr old (6.8% in the alcohol-associated group vs 32.6% in the non-alcohol-associated group) and the significantly older mean age in the alcohol-associated group (37.6 ± 15.0 yr vs 33.1 ± 19.9 yr) support our assumption (Table 3).
In conclusion, alcohol consumption significantly increases the risk of ocular trauma, especially by violence.
Figures and Tables
Table 2
Comparison of the frequencies of different types of ocular trauma with and without alcohol consumption
*Linear-by-linear association; †complex injury-includes 29 cases of orbital wall fracture combined with hyphema (n = 25), with open globe injury (n = 1), with corneal abrasion (n = 1), with optic nerve injury (n = 1), and with hyphema and retinal damage (n = 1). The remaining one case was a combination of periorbital contusion and hyphema.
AUTHOR SUMMARY
Association of Alcohol Consumption with the Risk of Ocular Trauma
Sang Beom Han, Hee Kyung Yang, Se Joon Woo, Joon Young Hyon, and Jeong-Min Hwang
We evaluated the influence of alcohol consumption on ocular trauma in Korea. The retrospective study of 1,024 patients (494 patients with ocular trauma and 530 patients without) showed remarkable difference. One of no trauma group and 117 (23.7%) of trauma group were related with alcohol consumption. As a cause of ocular trauma, physical assault was significantly more common in alcohol-associated injury (P < 0.001). Regarding the types of injury, orbital wall fracture and hyphema showed a significant association with alcohol consumption (P < 0.001). Older age and night time injury were significantly related to the increased risk of alcohol-associated ocular trauma (P = 0.018 and < 0.001, respectively).
References
1. Pihl RO, Peterson JB, Lau MA. A biosocial model of the alcohol-aggression relationship. J Stud Alcohol Suppl. 1993. 11:128–139.
2. Lee EJ, Kim TY, Kim SC, Park HS, Suh GJ, Shin SD, You EY. Effect of alcohol consumption on the severity of blunt injury. J Korean Soc Emerg Med. 2005. 16:339–345.
3. Lee WK, Kim Y. Drinking pattern and nonfatal injuries of adults in Korea. J Korean Soc Traumatol. 2009. 22:233–241.
4. Smith AR, O'Hagan SB, Gole GA. Epidemiology of open- and closed-globe trauma presenting to Cairns Base Hospital, Queensland. Clin Experiment Ophthalmol. 2006. 34:252–259.
5. Loon SC, Tay WT, Saw SM, Wang JJ, Wong TY. Prevalence and risk factors of ocular trauma in an urban south-east Asian population: the Singapore Malay Eye Study. Clin Experiment Ophthalmol. 2009. 37:362–367.
6. Kim MJ. Analysis of the medical expense by alcohol attributed diseases. J Korean Alcohol Sci. 2003. 4:136–148.
7. Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, Ramakrishnan R. Aravind Comprehensive Eye Survey. Ocular trauma in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology. 2004. 111:1778–1781.
8. McCarty CA, Fu CL, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology. 1999. 106:1847–1852.
9. Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: the Andhra Pradesh Eye Disease Study. Ophthalmology. 2006. 113:1159–1164.
10. Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in southern India: the Andhra Pradesh Eye Disease Study. Clin Experiment Ophthalmol. 2000. 28:350–356.
11. Han SB, Yu HG. Visual outcome after open globe injury and its predictive factors in Korea. J Trauma. 2010. 69:E66–E72.
12. Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye (Lond). 2006. 20:1336–1341.
13. Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008. 115:202–209.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download