Abstract
Intestinal metaplasia (IM) has been regarded as a premalignant condition. However, the pathogenesis of IM is not fully understood. The aim of this study was to evaluate the role of CDX1 and CDX2 in the formation of IM and the progression to dysplasia and gastric cancer (GC). A total of 270 subjects included 90 with GC, dysplasia and age- and sex-matched controls. Real-time PCR (RT-PCR) was performed with body specimens for CDX1 and CDX2. The expression of CDX2 was significantly higher in H. pylori positive group than H. pylori negative group (P = 0.045). CDX1 and CDX2 expression increased proportional to the IM grade of the body (P < 0.001). CDX2 expression was significantly higher in incomplete type of IM than in complete type (P = 0.045). The expression of CDX1 in dysplasia group was significantly higher than in the control group (P = 0.001); in addition, CDX1 and CDX2 in cancer group was significantly higher than control group (P < 0.001, and P < 0.001, respectively). Aberrant expression of CDX1 and CDX2 correlated with H. pylori infection and grade of IM in the body. Furthermore, the results suggest that CDX1 and CDX2 play a role in the progression to GC and dysplasia.
Gastric cancer (GC) is one of the most common malignancies in Korea. Correa (1) has suggested that intestinal GC develops through a sequence of histological changes, including diffuse chronic gastritis, mucosal atrophy, intestinal metaplasia (IM), dysplasia, and finally invasive carcinoma. Infection with Helicobacter pylori typically produces a chronic inflammatory condition that gives rise to IM. Gastric IM has been classified as complete (small intestine) or incomplete (colon) using immunohistochemical staining techniques. Another classification categorizes IM into three types: I (complete), II and III (incomplete) (2). For type I, the morphology is similar to the small intestinal mucosa where goblet cells secrete sialomucins, and Paneth cells are observed. For types II and III columnar cells are present where goblet cells secrete sulfomucins, but Paneth cells are not present. Type II IM typically exhibits the most extensive genetic changes. Many prior studies have evaluated the significance of type III IM as a risk factor for the development of the intestinal-type of GC (3, 4). However, the development of IM in relationship to GC remains unclear.
CDX1 and CDX2 are members of the caudal-related homeobox gene family and are intestine-specific transcriptional factors (5, 6). In adult mice and humans, expression of CDX1 and CDX2 is strictly confined to the gut, from the duodenum to the rectum. While normal gastric mucosa does not express the transcriptional factors CDX1 and CDX2, aberrant expression of CDX1 and CDX2 is observed in animal and human gastric IM (7-10). These findings suggest that CDX1 and CDX2 may play a pivotal role in the development of IM in the human stomach. With regard to GC, CDX2 is expressed in adenocarcinomas from various organs such as the stomach, colon, pancreas, gallbladder and lungs, and may be clinically useful for improved prediction of the outcome of patients with advanced cancer (11, 12). In addition, expression of CDX2 showed a significant positive correlation with dysplasia and cancer (13). By contrast, several studies from surgical specimens reported a reduction of CDX1 and CDX2 in the GC compared to IM (7, 9, 14). Therefore, the role of CDX1 and CDX2 in GC remains unclear. Furthermore, no study has investigated the expression of both CDX1 and CDX2 on a background mucosa of dysplasia and cancer in human gastric epithelium with respect to H. pylori infection, a main cause of IM.
Therefore both CDX1 and CDX2 expression in control subjects with dysplasia and patients with GC were studied. Furthermore, the relationship between the expression of these two proteins and the IM grade and subtype associated with H. pylori infection was investigated.
This study was performed at Seoul National University Bundang Hospital as a case-control study. Ninety patients with gastric cancer and 90 patients with dysplasia were enrolled from September 2003 to March 2007. Dysplasia includes low- and high-grade adenoma. Pathological diagnosis beyond adenocarcinoma in situ was classified into cancer group. Age- and sex-matched controls that underwent endoscopy for health screening or evaluation of upper gastrointestinal symptoms were eligible for participation. Subjects with a history of gastric surgery, H. pylori eradication therapy, medication of antisecretory drugs or non-steroidal anti-inflammatory drugs (NSAIDs), or systemic diseases requiring chronic medication were excluded. Smoking was defined as "current" when consumption was more than 5 cigarettes per day.
To determine the presence of current H. pylori infection, three types of H. pylori testing (histology, Campylobacter like organism [CLO] test [Delta West, Bentley, Australia] and culture) were used. One specimen from each of the lesser curvature of the antrum and the body was used for rapid urease testing (CLO test). Two specimens from the antrum and body were used for culture. The antral and body biopsy specimens were evaluated separately, and organisms were identified as H. pylori by Gram staining, colony morphology, and positive oxidase, catalase and urease reactions. If any one of these three H. pylori tests were positive then the host was regarded as having an ongoing H. pylori infection. The anti-H. pylori immunoglobulin G was also determined qualitatively using an enzyme-linked immunosorbent assay (Genedia H. pylori ELISA; Green Cross Medical Science Corp, Eumseong, Korea), especially when the three above-mentioned H. pylori tests were negative. When the H. pylori serology was positive but no bacteria were found on histology, CLO test or culture, these subjects were regarded as having past H. pylori infection without an ongoing infection, and classified as H. pylori-positive.
Two specimens (one from the greater curvature and one from the lesser curvature) were obtained from the antrum and body, respectively, and assessed for the degree of IM (all determined by hematoxylin-eosin staining). The histological features of the gastric mucosa were recorded using the updated Sydney scoring system (i.e., 0, none; 1, slight; 2, moderate; and 3, marked). The average of the score in the greater curvature and the lesser curvature were used for comparison between the groups. All biopsies were examined independently by two experienced pathologists, who were unaware of the patient details. In the event of disagreement, the biopsies were reexamined by these two pathologists until agreement was reached.
Samples were also stained with alcian blue (AB) and high iron diamine (HID) to categorize IM as the complete (Type I) or incomplete (Type II and II). Slides were immersed in HID solution for 20 hr at room temperature, then rinsed with deionized water and stained with 1% AB for 2 min. IM subtyping was performed according to the system reported by Filipe et al. (2) and Shiotani et al. (15). If more than one HID subtype of IM was present, the dominant IM phenotype was used for classification. In addition, the pathologists were blinded to the clinical information of the patients.
Total RNA was extracted from body specimens (one from the greater curvature and one from the lesser curvature) of the gastric mucosa using Trizol Reagent (Invitrogen, Carlsbad, CA, USA). RNA samples were diluted to a final concentration of 0.5 mg/mL in RNase-free water and stored at -80℃ until use. Synthesis of the cDNA was performed with 1 mg of total RNA with M-MLV reverse transcription reagents (Invitrogen), and real-time PCR reaction was carried out on the ABI PRISM 7000 Sequence Detection System (Applied Biosystems, Foster City, CA, USA) in 20 µL TaqMan Gene Expression Master Mix (Applied Biosystems) using 200 ng cDNA. Target genes for CDX1 and CDX2 were tested using Assay-on-Demand Gene Expression products. The pre-designed primer sets were ordered according to http://www.appliedbiosystems.com/ (CDX1 assay ID number: Hs00156451_m1; CDX2 assay ID number: Hs01078080_m1; β-actin assay ID number: Hs99999903_m1) and used according to their protocols. The reaction conditions were 50℃ for 2 min and 95℃ for 10 min followed by 40 cycles of 95℃ for 15 sec and 60℃ for 1 min. The human beta-actin gene was used as an endogenous reference to control for the independent expression of sample-to-sample variability. The relative expression of target genes was normalized by dividing the target Ct values by the endogenous Ct values. All equipment was purchased from Applied Biosystems and used according to their protocols.
All statistical analyses were performed using SPSS software ver. 15.0 (SPSS Software, Chicago, IL, USA). The Student's t-test or the Pearson chi-square test were used to compare two groups. Correlations between IM grade and CDX1 and CDX2 expressions were performed using the Pearson correlation test and partial correlation coefficients adjusted for disease group.
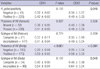
A total of 270 patients in the study group included 90 with GC and 90 age- and sex-matched controls in addition to 90 patients with dysplasia. The gastric dysplasia biopsies were diagnosed as 60 low-grade and 30 high-grade dysplasia. The baseline characteristics are shown in Table 1. The H. pylori positivity and proportion of current smoker in patients with cancer and dysplasia did not differ from the control group. The grade of IM in the antrum was significantly higher in the dysplasia group compared to the control group (P = 0.016). The grade of IM in the body was significantly higher in the dysplasia and cancer group compared to the control group (P < 0.001 and P < 0.001, respectively) (Table 1). However, the subtype of IM was not different among the three different study groups.
The expression of CDX1 and CDX2 in the body specimens were positively correlated with the grade of IM not only before (r = 0.414, P < 0.001 and r = 0.380, P < 0.001, respectively) and but also after adjustment for 3 disease groups (partial r = 0.377, P < 0.001 and partial r = 0.346, P < 0.001, respectively) (Fig. 1B, D). However, there was no significant correlation between the expression of CDX1/CDX2 and the grade of IM in the antrum not only before (r = 0.106, P = 0.081 and r = 0.067, P < 0.273, respectively) but also after adjustment for 3 disease groups (partial r = 0.091, P = 0.136 and partial r = 0.052, P = 0.392, respectively) (Fig. 1A, C).
The expression of CDX1 but not CDX2 in the dysplasia group was significantly higher than control group (P < 0.001, Fig. 2). When it comes to cancer group, the expression of CDX1 and CDX2 was significantly higher than the control group (P < 0.001 and P < 0.001, respectively, Fig. 2). However, the expression of CDX1 and CDX2 between dysplasia group and cancer was not different.
A comparison of the expression of CDX1 and CDX2 with respect to the presence of H. pylori and IM is shown in Table 2. With regard to H. pylori positivity, the expression of CDX2 but not CDX1 was significantly higher in the H. pylori positive group than the H. pylori negative group (P = 0.045). The expression of CDX1 and CDX2 was higher with IM than without IM in the body (P < 0.001 and P < 0.001, respectively). Furthermore, expression of CDX2 but not CDX1 was higher in the incomplete type of IM in the body (0.64 ± 0.04) compared to the complete type (0.46 ± 0.08) (P = 0.045) (Table 2). However, the expression of CDX1 and CDX2 was not different with respect to the presence or the subtype of IM in the antrum.
In IM of the human stomach, normal gastric mucosa is replaced by an intestinalized epithelium; the progression of H. pylori-infected chronic gastritis facilitates the development of IM. IM of the human stomach has been extensively studied as a premalignant condition of gastric carcinoma (16). However, the formation and progression of IM is not completely understood; there is limited information on the biology of IM in the medical literature (10, 17). Furthermore, the role of IM in the progression to GC is unclear.
The intestine-specific homeobox genes CDX1 and CDX2 have been shown to be aberrantly expressed in human IM (9, 10, 18). In the present study, CDX1 and CDX2 expression was strongly correlated with the grade of IM in the body, consistent with previous studies (14, 18, 19). However, there was no significant correlation between the expression of CDX1/CDX2 and the grade of IM in the antrum. In addition, there was no significant difference in the expression of CDX1 and CDX2 according to the presence of IM in the antrum. This might be originated from the fact that RT-PCR for CDX1 and CDX2 was only performed using specimens from the body but not from antrum in the present study. Previous study showed that CDX2 expression tended to be positive in the antrum but was negative in the fundic mucosa in stomach lacking features of IM, whereas CDX2 tended to be positive in both antral and fundic mucosa in stomach with IM (10). Consequently, CDX2 expression may be evoked in the antrum before expression occurs in the fundic gland mucosa. Thus CDX2 expression in the body might reflect the status of gastric IM more closely than that in the antrum although we did not measure CDX2 expression in the antrum. These findings suggest that CDX1 and CDX2 may play a pivotal role in the development of IM in the body but not the antrum, which is more strongly associated with development of GC than that in the antrum. However, the specific role of CDX1 and CDX2 in the determination of the IM subtype appears to be different. That is, IM in CDX1 transgenic mice show all of the cell types of IM including Paneth cells similar to the complete type of IM; on the other hand, IM in CDX2 transgenic mice have similar features with the incomplete type of IM (20). In the present study, CDX2 expression was significantly higher in the incomplete type of corpus IM compared to the complete type, consistent with the findings of a previous study (21). However, the CDX1 expression was not different according to the subtype of IM. These results suggest that CDX2 plays a major role than CDX1 in the determination of the incomplete type of IM.
Previous studies have suggested that CDX2 expression is associated not only with IM but also with early stage GC (11, 22, 23). Recently, Mutoh et al. (24) reported that gastric polyps that develop from intestinal metaplastic mucosa of the stomach of CDX2 transgenic mice had intestinal type adenocarcinoma containing p53 and APC gene mutations. On the other hand, some reports have suggested that CDX2 functions as a tumor suppressor gene because of its role in the colon as a tumor suppressor gene (25). Furthermore, a decreased expression of CDX2 was associated with the progression of IM to dysplasia and cancer (17). However, induction of GC has also been observed in CDX2 transgenic mice (24, 26). To date, the information on CDX2 expression in gastric epithelial dysplasia is limited and inconsistent (13, 17, 27) and there is no study regarding CDX1 expression in gastric dysplasia. In the present study, aberrant expression of CDX1 and CDX2 was frequently observed in patients with GC and dysplasia although expression of CDX2 in dysplasia did not reach statistical significance (P = 0.10). These results were further supported by additional findings that the grade of IM in the body was significantly higher in the dysplasia and cancer groups than in the control group. Taken together these findings might suggest that CDX2 is involved in the development of cancer from dysplasia, which is different from CDX1. However, further molecular based studies are needed in the larger population to elucidate the changes in the expression of CDX1 and CDX2 in the carcinogenesis from dysplasia to cancer.
Chronic H. pylori infection has been shown to induce CDX2 expression in the human stomach prior to the development of IM (10, 18). In addition, in vitro H. pylori infection increased the expression of CDX2 in a gastric carcinoma cell line (AGS) (28). Furthermore, several studies have demonstrated that the expression of CDX2 was decreased after H. pylori eradication (29, 30). However, there has been no study on the effects of H. pylori infection on CDX1 expression. In the present study, the expression of CDX2 was significantly higher in the H. pylori positive group than the H. pylori negative group consistent previous report. Meanwhile, expression of CDX1 in H. pylori positive group tend to be higher than the H. pylori negative group without statistical significance (P = 0.191). From these results we can suggest that CDX2 is closely related with H. pylori infection as well as IM grade but in case of CDX1 the trend is weak in terms of H. pylori infection. However, these might be originated from the small number of H. pylori negative group in the present study. Thus further study is needed to elucidate whether H. pylori-associated IM might be correlated with CDX1 in the larger population without H. pylori.
The present study had several advantage compared to the previous studies. First, it investigated CDX1 as well as CDX2 by quantitative analysis using real-time PCR. Second, in order to evaluate the effect of H. pylori infection on the expression of CDX1 and CDX2, four kinds of H. pylori tests (histology, CLOtest and culture from antrum and body, and serology to exclude the past infection) were used. Third, most of previous studies covered only gastric cancer patients but we evaluated cancer group as well as dysplasia group, and which age and sex were matched with control group. The number was 90 patients for each group. From this design we tried to provide a clue whether there is a difference of CDX1 and CDX2 in the role of gastric carcinogenesis. However, the study had limitation that RT-PCR for CDX1 and CDX2 was only performed using specimens from the body but not from the antrum mainly from the availability of RNA. As the analysis of CDX1 and CDX2 was not performed in the antrum the levels of expression of CDX1 and CDX2 regarding to the presence of IM or subtype of IM were not clearly shown in the antrum as in the body.
In conclusion, aberrant expression of CDX1 and CDX2 is correlated with H. pylori infection and grade of IM in the body. It is suggested that CDX1 and CDX2 play a role in the carcinogenesis of the stomach.
Figures and Tables
 | Fig. 1Correlation between CDX1 and CDX2 expression and grade of intestinal metaplasia. CDX1 in the antrum (A) and body (B), CDX2 in the antrum (C) and body (D). r, correlation coefficient. |
 | Fig. 2The comparison of the CDX1 and CDX2 expression according to disease group. The relative mRNA expression of the CDX1 (A) and CDX2 (B) of dysplasia and gastric cancer groups with the control group. Data are presented as means ± standard error. |
AUTHOR SUMMARY
CDX1 and CDX2 Expression in Intestinal Metaplasia, Dysplasia and Gastric Cancer
Jung Mook Kang, Byoung Hwan Lee, Nayoung Kim, Hye Seung Lee, Hee Eun Lee, Ji Hyun Park, Joo Sung Kim, Hyun Chae Jung, and In Sung Song
The aim of this study was to evaluate the role of CDX1 and CDX2 in the formation of intestinal metaplasia (IM) and the progression to dysplasia and gastric cancer (GC). A total of 270 subjects included 90 with GC, dysplasia and age- sex-matched controls, respectively. The expression of CDX2 was significantly higher in H. pylori positive group than H. pylori negative group. CDX1 and CDX2 expression increased proportional to the IM grade of the body. CDX2 expression was significantly higher in incomplete type of IM than in complete type. The expression of CDX1 in dysplasia group was significantly higher than in the control group; in addition, CDX1 and CDX2 in cancer group was significantly higher than control group. Aberrant expression of CDX1 and CDX2 correlated with H. pylori infection and grade of IM in the body. Furthermore, the results suggest that CDX1 and CDX2 play a role in the progression to GC and dysplasia.
References
1. Correa P. A human model of gastric carcinogenesis. Cancer Res. 1988. 48:3554–3560.
2. Filipe MI, Potet F, Bogomoletz WV, Dawson PA, Fabiani B, Chauveinc P, Fenzy A, Gazzard B, Goldfain D, Zeegen R. Incomplete sulphomucin-secreting intestinal metaplasia for gastric cancer. Preliminary data from a prospective study from three centres. Gut. 1985. 26:1319–1326.
3. El-Zimaity HM, Ota H, Graham DY, Akamatsu T, Katsuyama T. Patterns of gastric atrophy in intestinal type gastric carcinoma. Cancer. 2002. 94:1428–1436.
4. Iida F, Kusama J. Gastric carcinoma and intestinal metaplasia. Significance of types of intestinal metaplasia upon development of gastric carcinoma. Cancer. 1982. 50:2854–2858.
5. Silberg DG, Swain GP, Suh ER, Traber PG. Cdx1 and cdx2 expression during intestinal development. Gastroenterology. 2000. 119:961–971.
6. Suh E, Chen L, Taylor J, Traber PG. A homeodomain protein related to caudal regulates intestine-specific gene transcription. Mol Cell Biol. 1994. 14:7340–7351.
7. Almeida R, Silva E, Santos-Silva F, Silberg DG, Wang J, De Bolós C, David L. Expression of intestine-specific transcription factors, CDX1 and CDX2, in intestinal metaplasia and gastric carcinomas. J Pathol. 2003. 199:36–40.
8. Silberg DG, Sullivan J, Kang E, Swain GP, Moffett J, Sund NJ, Sackett SD, Kaestner KH. Cdx2 ectopic expression induces gastric intestinal metaplasia in transgenic mice. Gastroenterology. 2002. 122:689–696.
9. Silberg DG, Furth EE, Taylor JK, Schuck T, Chiou T, Traber PG. CDX1 protein expression in normal, metaplastic, and neoplastic human alimentary tract epithelium. Gastroenterology. 1997. 113:478–486.
10. Eda A, Osawa H, Yanaka I, Satoh K, Mutoh H, Kihira K, Sugano K. Expression of homeobox gene CDX2 precedes that of CDX1 during the progression of intestinal metaplasia. J Gastroenterol. 2002. 37:94–100.
11. Seno H, Oshima M, Taniguchi MA, Usami K, Ishikawa TO, Chiba T, Taketo MM. CDX2 expression in the stomach with intestinal metaplasia and intestinal-type cancer: prognostic implications. Int J Oncol. 2002. 21:769–774.
12. Kim MJ. The usefulness of CDX-2 for differentiating primary and metastatic ovarian carcinoma: an immunohistochemical study using a tissue microarray. J Korean Med Sci. 2005. 20:643–648.
13. Kim HS, Lee JS, Freund JN, Min KW, Kim W, Juhng SW, Park CS. CDX-2 homeobox gene expression in human gastric carcinoma and precursor lesions. J Gastroenterol Hepatol. 2006. 21:438–442.
14. Bai YQ, Yamamoto H, Akiyama Y, Tanaka H, Takizawa T, Koike M, Kenji Yagi O, Saitoh K, Takeshita K, Iwai T, Yuasa Y. Ectopic expression of homeodomain protein CDX2 in intestinal metaplasia and carcinomas of the stomach. Cancer Lett. 2002. 176:47–55.
15. Shiotani A, Haruma K, Uedo N, Iishi H, Ishihara R, Tatsuta M, Kumamoto M, Nakae Y, Ishiguro S, Graham DY. Histological risk markers for non-cardia early gastric cancer. Pattern of mucin expression and gastric cancer. Virchows Arch. 2006. 449:652–659.
16. Correa P. Human gastric carcinogenesis: a multistep and multifactorial process--First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res. 1992. 52:6735–6740.
17. Liu Q, Teh M, Ito K, Shah N, Ito Y, Yeoh KG. CDX2 expression is progressively decreased in human gastric intestinal metaplasia, dysplasia and cancer. Mod Pathol. 2007. 20:1286–1297.
18. Satoh K, Mutoh H, Eda A, Yanaka I, Osawa H, Honda S, Kawata H, Kihira K, Sugano K. Aberrant expression of CDX2 in the gastric mucosa with and without intestinal metaplasia: effect of eradication of Helicobacter pylori. Helicobacter. 2002. 7:192–198.
19. Mizoshita T, Inada K, Tsukamoto T, Kodera Y, Yamamura Y, Hirai T, Kato T, Joh T, Itoh M, Tatematsu M. Expression of Cdx1 and Cdx2 mRNAs and relevance of this expression to differentiation in human gastrointestinal mucosa--with special emphasis on participation in intestinal metaplasia of the human stomach. Gastric Cancer. 2001. 4:185–191.
20. Mutoh H, Sakurai S, Satoh K, Osawa H, Hakamata Y, Takeuchi T, Sugano K. Cdx1 induced intestinal metaplasia in the transgenic mouse stomach: comparative study with Cdx2 transgenic mice. Gut. 2004. 53:1416–1423.
21. Shiotani A, Iishi H, Uedo N, Ishihara R, Ishiguro S, Tatsuta M, Nakae Y, Kumamoto M, Hinoi T, Merchant JL. Helicobacter pylori-induced atrophic gastritis progressing to gastric cancer exhibits sonic hedgehog loss and aberrant CDX2 expression. Aliment Pharmacol Ther. 2006. 24:Suppl 4. 71–80.
22. Kim GH, Song GA, Park DY, Lee SH, Lee DH, Kim TO, Jo HJ, Heo J, Kang DH, Cho M. CDX2 expression is increased in gastric cancers with less invasiveness and intestinal mucin phenotype. Scand J Gastroenterol. 2006. 41:880–886.
23. Mizoshita T, Tsukamoto T, Nakanishi H, Inada K, Ogasawara N, Joh T, Itoh M, Yamamura Y, Tatematsu M. Expression of Cdx2 and the phenotype of advanced gastric cancers: relationship with prognosis. J Cancer Res Clin Oncol. 2003. 129:727–734.
24. Mutoh H, Sakurai S, Satoh K, Tamada K, Kita H, Osawa H, Tomiyama T, Sato Y, Yamamoto H, Isoda N, Yoshida T, Ido K, Sugano K. Development of gastric carcinoma from intestinal metaplasia in Cdx2-transgenic mice. Cancer Res. 2004. 64:7740–7747.
25. Bonhomme C, Duluc I, Martin E, Chawengsaksophak K, Chenard MP, Kedinger M, Beck F, Freund JN, Domon-Dell C. The Cdx2 homeobox gene has a tumour suppressor function in the distal colon in addition to a homeotic role during gut development. Gut. 2003. 52:1465–1471.
26. Witek ME, Nielsen K, Walters R, Hyslop T, Palazzo J, Schulz S, Waldman SA. The putative tumor suppressor Cdx2 is overexpressed by human colorectal adenocarcinomas. Clin Cancer Res. 2005. 11:8549–8556.
27. Rugge M, Ingravallo G, Farinati F, Russo VM, Zaninotto G, Alvisi V. Re: CDX2 homeotic gene expression in gastric noninvasive neoplasia. Am J Surg Pathol. 2004. 28:834–835.
28. Barros R, Marcos N, Reis CA, De Luca A, David L, Almeida R. CDX2 expression is induced by Helicobacter pylori in AGS cells. Scand J Gastroenterol. 2009. 44:124–125.
29. Vauhkonen M, Vauhkonen H, Sipponen P. Helicobacter pylori infection induces a reversible expression of the CDX2 transcription factor protein in human gastric epithelium. Scand J Gastroenterol. 2008. 43:915–921.
30. Shiotani A, Uedo N, Iishi H, Tatsuta M, Ishiguro S, Nakae Y, Kamada T, Haruma K, Merchant JL. Re-expression of sonic hedgehog and reduction of CDX2 after Helicobacter pylori eradication prior to incomplete intestinal metaplasia. Int J Cancer. 2007. 121:1182–1189.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download