Abstract
Prevalence of erosive esophagitis (EE) has been increasing in Korea. The purpose of this study was to estimate prevalence of EE among low socioeconomic population in Korea and to investigate risk factors for EE. We reviewed the medical records of 7,278 subjects who were examined by upper endoscopy in the Korean National Cancer Screening Program at Chung-Ang University Yong-san Hospital from March 2003 to March 2008. The study population included subjects ≥ 40 yr of age who were Medicaid recipients and beneficiaries in the National Health Insurance Corporation. Multivariate analysis was used to determine risk factors for EE. Prevalence of EE was 6.7% (486/7,278). According to the LA classification system, LA-A in 344 subjects, LA-B in 135 subjects, and LA-C and D in 7 subjects. In multivariate analysis, age ≥ 60 yr, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, and endoscopic hiatal hernia were significant risk factors for EE. The prevalence of EE in low socioeconomic Korean population is similar to that in personal annual medical check-ups. Risk factors for EE among them include old age, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, and hiatal hernia.
Gastroesophageal reflux disease (GERD) is a condition that develops when reflux of stomach contents causes troublesome symptoms and complications, such as reflux esophagitits, hemorrhage, stricture, Barrett's esophagus, and adenocarcinoma (1). According to the Montreal workshop report, reflux esophagitis is defined endoscopically by visible breaks in the distal esophageal mucosa (1). In clinical practice, endoscopic esophagitis is seen in less than 50% of patients with typical GERD symptoms (2). Several recent endoscope-based studies have suggested that overall prevalence of reflux esophagitis in Western Europe and North America was around 10%-20% (3, 4). In contrast, GERD has traditionally been considered less common in Asia (5-7). However, more recent studies suggest that prevalence of GERD in Asia is increasing (3, 8). In Japan, the overall prevalence of reflux esophagitis among the adult population is roughly 10%-15% (9). Incidence of erosive esophagitis (EE) is also increasing in the Korean population (10-12). For example, prevalence of EE in subjects undergoing a routine check up was reported at around 2% in the early 1990s, and 5% in the late 1990s (4). In 2006, the prevalence of EE was found to be 8% (13). Incidence is expected to increase, not only due to developments in endoscopic examination and increasing awareness of the condition, but also because of changes in preference to a more westernized diet and lifestyle (4).
Up to now, many epidemiologic studies of EE, particularly those from Korea, have had a potential limitation, in that most did not fully represent population-based results. Subjects who attended personal annual medical check-ups had a higher income and higher educational level than average population (14, 15). Thus, the chance of selection bias exists.
Therefore, we attempted to estimate the prevalence of EE in Koreans, including those of low socio-economic status. Actually, the study population included subjects ≥ 40 yr of age who were Medicaid recipients and beneficiaries in the National Health Insurance Corporation. In addition, we attempted to investigate risk factors for EE among them.
The present study was conducted by medical record review. A total of 7,278 subjects underwent upper endoscopy as a part of National Cancer Screening Program at Chung-Ang University Yongsan Hospital in Korea during the 5-yr period from March 2003 to March 2008. The study population was comprised of subjects over the age of 40 yr who were Medicaid recipients and beneficiaries of the National Health Insurance Corporation. Information on age, gender, current smoking status, and alcohol consumption habits were all collected from a standardized questionnaire based on medical check-up results from the National Health Insurance Corporation. Height and body weight were measured for each subject. Blood was drawn, and fasting glucose and total cholesterol were measured.
Esophagoduodenoscopy (EGDs) were performed by 4 well-trained gastroenterologists with at least 5 yr of endoscopy experience using a flexible endoscope (Q260 or Q240, Olympus Optical Co., Tokyo, Japan), providing pharyngeal anesthesia with 2% xylocaine spray. Severities of EE were defined based on endoscopic findings according to the LA classification from grade A to D. Endoscopically suspected esophageal metaplasia (ESEM) was defined as an endoscopic abnormality suggestive of Barrett's esophagus, which indicated a tongue-like extension of salmon-colored mucosa from the esophagogastric junction (EGJ; defined as the point where the proximal end of the gastric folds meet the tubular esophagus) (10). Hiatal hernia (HH) was defined as present when the distance from the proximal end of the gastric folds to the diaphragm was greater than 1 cm (16). Endoscopic findings, such as gastric ulcer, duodenal ulcer, ESEM, and HH, as well as esophageal erosion were assessed.
The following variables were included: age and sex, blood pressure, body mass index (BMI), fasting glucose, total cholesterol, current smoking status, and alcohol consumption habits (≥ 80 g/day). BMI was classified according to World Health Organization BMI criteria as normal (< 23 kg/m2), overweight (23-24.9 kg/m2), and obese (≥ 25 kg/m2). The categorized cut-off value of blood pressure, fasting glucose, and total cholesterol was 140/90 mmHg, 126 and 200 mg/dL, respectively.
Statistical analyses in this study were conducted using the SPSS version 12.0 software package (SPSS, Chicago, IL, USA). Statistical analysis was performed using the chi-square test for comparison of discrete variables, and the t-test was used for comparison of continuous variables. Continuous variables measured in this study are expressed as the mean ± SD. Multivariate analysis was performed using logistic regression. To examine the risks of potential confounders for erosive esophagitis, multivariate models included adjustment for age, sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose (≥ 126 mg/dL), ESEM, and HH. The odds ratio (OR) and 95% confidence interval (95% CI) are given for each variable. A two-tailed P value < 0.05 was considered statistically significant.
Among a total of 7,278 subjects, 486 subjects were found to have erosive esophagitis, and the overall prevalence was 6.7%. Most of these showed a mild grade of EE, 71% of whom presented with grade A, followed by 28% with grade B, and 1% with grades C and D.
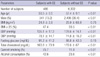
Demographics between subjects with and without EE are summarized in Table 1. Mean age of subjects with EE was 60 yr, compared with 57 yr in those without EE (P < 0.01). When age group was stratified by 40-49, 50-59, 60-69, and ≥ 70 yr old, prevalence of EE ranged from 5.1% to 9.3%. Male sex was predominant in subjects with EE compared to those without EE (P < 0.01). Prevalence of EE in males was 10.9%, and prevalence of EE in females was only 3.5%. BMI was not significantly different between subjects with and without EE (P = 0.75); however, the percentage of BMI ≥ 25 was found to be higher in subjects with EE than in those without EE (P < 0.01). Current smoking and alcohol consumption were significantly higher in subjects with EE than those without EE (P < 0.01, respectively). However, fasting glucose was not significantly different between the two groups (P = 0.15).
Endoscopic findings were compared between the two groups (Fig. 1). Prevalence of gastric ulcer and duodenal ulcer was not significantly different between the two groups. However, prevalence of ESEM and HH was significantly higher in subjects with EE than in those without EE.
Risk factors for EE are analyzed and summarized in Table 2. According to univariate analysis, age ≥ 60 yr, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, ESEM, and HH were significant risk factors. In multivariate analysis, however, old age, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, and HH were significant risk factors. ESEM was not shown to be a significant risk factor in EE.
In Korea, it is generally accepted that the nationwide prevalence of reflux esophagitis is lower than that in Western countries. However, recent studies have shown an increasing trend in the number of patients with reflux esophagitis (17, 18). In addition, EE is increasing in Asia (14). For example, it has increased from 3% in the late 1970s to 10%-15% in the late 1990s, as reported by a Japanese study of upper gastrointestinal endoscopies (19). In addition, it has increased from 3% in the early 1990s to 13% in 2000-2001, based on a Malaysian study (20). A recent large-scaled nationwide multicenter Korean study revealed that prevalence of EE in healthy subjects who had routine check-ups was 7.9% in Korea (n = 25,536) (13). In this study, endoscopic examination indicated that the overall prevalence of EE in Korean Medicaid recipients and beneficiaries over the age of 40 yr was 6.7%.
The Korean National Cancer Screening Program (NCSP) was initiated in 1999 for the purpose of reducing cancer-related mortality through early detection of most common cancers in Koreans through mass screening programs (21). The target five most common cancers, which are among the leading causes of death in Korea, include stomach cancer, breast cancer, cervical cancer, liver cancer, and colon cancer. In particular, the Korean government offers this cancer screening program for free to the general population who are over the age of 40 yr, including beneficiaries in the National Health Insurance Corporation, which is a kind of social security health system in Korea, as well as Medicaid recipients who are low income members of the Korean population (22).
Most epidemiologic studies on EE, particularly those from Korea, have not shown population-based results. Thus, the present study could be representative of the general Korean population who are over the age of 40 yr.
Although we did not evaluate the grade of minimal change in erosive esophagitis due to its flaw of low interobserver agreement, endoscopic evaluation showed that most of the subjects had mild grade EE with grade A. Mild degree of EE in this study might explain the lower prevalence of EE in Korea compared with other Asian countries, such as Japan (5). This difference among countries is observed in the distribution based on the LA classification of EE. In Korea, LA-A accounted for 71%, LA-B 28%, and LA-C plus LA-D 1% in this study, which differs from LA-C plus LA-D of 12% reported in Japan (23) and LA-C plus LA-D of 20% reported in Malaysia (20). These differences regarding prevalence and severity of EE in Asian populations are not easily explained, but may be a result of genetic background, diet, or Helicobacter pylori infection status (14).
In this study, we divided the subjects into two groups according to the presence of EE on upper endoscopy. Clinical features and endoscopic findings between the two groups were compared.
Based on several results from Asian studies, probable risk factors are presumed to be related to EE; age ≥ 60 yr old, male gender, obesity, especially BMI ≥ 25, H. pylori eradication history, smoking, alcohol consumption, and endoscopic findings of HH are shown to be significant risk factors (13, 24). In accordance with previous reports, this study revealed that old age, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, and hiatal hernia were significant risk factors for EE. ESEM was not proven to be a significant risk factor in EE, although it was predominant in subjects with EE in comparison to those without EE.
Interestingly, a recent report from Korea suggests that EE might represent the disease spectrum of the metabolic syndrome showing significant relationship of EE to obesity, low HDL cholesterol, high triglyceride, high blood pressure, and elevated fasting glucose (4). In this study, BMI was not significantly different between subjects with EE and those without EE; however, the percentage of BMI ≥ 25 was found to be higher in subjects with EE than in those without EE. This suggests that obesity, one of the components of metabolic syndrome, is associated with EE.
With regard to endoscopic evaluation of EE, HH could be an important clue to diagnosis of GERD and it also implies possible progression to EE. Although this study did not ascertain the significance of ESEM in diagnosis of EE, ESEM may remain as an important endoscopic finding in Barrett's esophagus, one of the complications of EE. There was some limitation in this study. Because our study was a retrospective study, GERD-related symptoms, such as heartburn and acid regurgitation, were not investigated. Furthermore, lack of information on H. pylori eradication history failed to elucidate the relationship between H. pylori infection and EE.
In conclusion, the prevalence of EE was 6.7% in low socioeconomic Korean population, and it is close to that of recent reports in healthy individuals who voluntarily underwent personal annual medical check-ups. Risk factors for EE among them include old age, male sex, BMI ≥ 25, current smoking, alcohol consumption, fasting glucose level ≥ 126 mg/dL, and HH.
Figures and Tables
Fig. 1
Endoscopic findings between subjects with and without erosive esophagitis (EE). Endoscopic findings were compared between the two groups. Prevalence of gastric ulcer (GU) and duodenal ulcer (DU) were not significantly different between the two groups. However, prevalence of endoscopically suspected esophageal metaplasia (ESEM) and hiatal hernia (HH) were significantly higher in subjects with EE than in those without.

AUTHOR SUMMARY
Prevalence and Risk Factor of Erosive Esophagitis Observed in Korean National Cancer Screening Program
Beom Jin Kim, Won Seok Cheon, Hyoung-Chul Oh, Jeong Wook Kim, Jung Duck Park, and Jae G. Kim
This study was conducted to estimate prevalence of erosive esophagitis (EE) among low socioeconomic population in Korea and to investigate risk factors for EE. We reviewed the medical records of 7,278 subjects who were examined by upper endoscopy in the Korean National Cancer Screening Program at Chung-Ang University Yong-san Hospital from March 2003 to March 2008. The study population included subjects over 40 yr of age who were Medicaid recipients and beneficiaries in the National Health Insurance Corporation. As a result, prevalence of EE was 6.7% (486/7,278), which is similar to that in report of personal annual medical check-ups. According to the LA classification system, LA-A in 344 subjects, LA-B in 135 subjects, and LA-C and D in 7 subjects. Risk factors for EE among them include old age, male sex, BMI over 25, current smoking, alcohol consumption, fasting glucose level over 126 mg/dL, and hiatal hernia.
References
1. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Globale Konsensusgruppe. The Montreal definition and classification of gastroesophageal reflux disease: a global, evidence-based consensus paper. Z Gastroenterol. 2007. 45:1125–1140.
2. Lind T, Havelund T, Lundell L, Glise H, Lauritsen K, Pedersen SA, Anker-Hansen O, Stubberöd A, Eriksson G, Carlsson R, Junghard O. On demand therapy with omeprazole for the long-term management of patients with heartburn without oesophagitis--a placebo-controlled randomized trial. Aliment Pharmacol Ther. 1999. 13:907–914.
3. Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008. 23:1785–1793.
4. Song HJ, Shim KN, Yoon SJ, Kim SE, Oh HJ, Ryu KH, Ha CY, Yeom HJ, Song JH, Jung SA, Yoo K. The prevalence and clinical characteristics of reflux esophagitis in Koreans and its possible relation to metabolic syndrome. J Korean Med Sci. 2009. 24:197–202.
5. Wong RK, Yeoh KG, Gwee KA, Tay HW, Ho KY. Validation of structured scoring using the LA classification for esophagitis and endoscopically suspected Barrett's esophagus in a tertiary Asian endoscopy center. J Gastroenterol Hepatol. 2009. 24:103–106.
6. Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005. 54:710–717.
7. Kang JY. Systematic review: geographical and ethnic differences in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004. 20:705–717.
8. Cho YS, Choi MG, Jeong JJ, Chung WC, Lee IS, Kim SW, Han SW, Choi KY, Chung IS. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005. 100:747–753.
9. Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol. 2009. 44:518–534.
10. Tseng PH, Lee YC, Chiu HM, Huang SP, Liao WC, Chen CC, Wang HP, Wu MS, Lin JT. Prevalence and clinical characteristics of Barrett's esophagus
in a Chinese general population. J Clin Gastroenterol. 2008. 42:1074–1079.
11. Lee SJ, Song CW, Jeen YT, Chun HJ, Lee HS, Um SH, Lee SW, Choi JH, Kim CD, Ryu HS, Hyun JH. Prevalence of endoscopic reflux esophagitis among Koreans. J Gastroenterol Hepatol. 2001. 16:373–376.
12. Hwang JK, Kim J, Hong SG, Jung SJ, Joo MK, Lee BJ, Park JJ, Kim JS, Bak YT. A prospective multicenter study on the prevalence and symptoms of erosive reflux esophagitis in secondary and tertiary hospitals in Korea. Korean J Gastroenterol. 2009. 53:283–291.
13. Shim KN, Hong SJ, Sung JK, Park KS, Kim SE, Park HS, Kim YS, Lim SH, Kim CH, Park MJ, Yim JY, Cho KR, Kim D, Park SJ, Jee SR, Kim JI, Park JY, Song GA, Jung HY, Lee YC, Kim JG, Kim JJ, Kim N, Park SH, Jung HC, Chung IS. H. pylori and GERD Study Group of Korean College of Helicobacter and Upper Gastrointestinal Research. Clinical spectrum of reflux esophagitis among 25,536 Koreans who underwent a health check-up: a nationwide multicenter prospective, endoscopy-based study. J Clin Gastroenterol. 2009. 43:632–638.
14. Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS, Rew JS, Moon JS, Kim S, Park SH, Jung HC, Chung IS. H. pylori and Gerd Study Group of Korean College of Helicobacter and Upper Gastrointestinal Research. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther. 2008. 27:173–185.
15. Lee HY, Park EC, Jun JK, Hahm MI, Jung KW, Kim Y, Han MA, Choi KS. Trends in socioeconomic disparities in organized and opportunistic gastric cancer screening in Korea (2005-2009). Cancer Epidemiol Biomarkers Prev. 2010. 19:1919–1926.
16. Fujiwara Y, Higuchi K, Shiba M, Yamamori K, Watanabe Y, Sasaki E, Tominaga K, Watanabe T, Oshitani N, Arakawa T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am J Gastroenterol. 2005. 100:754–758.
17. Goh KL, Chang CS, Fock KM, Ke M, Park HJ, Lam SK. Gastro-oesophageal reflux disease in Asia. J Gastroenterol Hepatol. 2000. 15:230–238.
18. Yeom JS, Park HJ, Cho JS, Lee SI, Park IS. Reflux esophagitis and its relationship to hiatal hernia. J Korean Med Sci. 1999. 14:253–256.
19. Hongo M, Shoji T. Epidemiology of reflux disease and CLE in East Asia. J Gastroenterol. 2003. 38:Suppl 15. 25–30.
20. Rosaida MS, Goh KL. Gastro-oesophageal reflux disease, reflux oesophagitis and non-erosive reflux disease in a multiracial Asian population: a prospective, endoscopy based study. Eur J Gastroenterol Hepatol. 2004. 16:495–501.
21. Ahn YO. Cancer in Korea: present features. Jpn J Clin Oncol. 2002. 32:Suppl. S32–S36.
22. Yoo KY. Cancer control activities in the Republic of Korea. Jpn J Clin Oncol. 2008. 38:327–333.
23. Okamoto K, Iwakiri R, Mori M, Hara M, Oda K, Danjo A, Ootani A, Sakata H, Fujimoto K. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003. 48:2237–2241.
24. Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007. 41:131–137.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download